Abstract
Herein, we report a case of classical Hodgkin’s lymphoma (HL) in an otherwise healthy 27- year-old female who came to the office of her general practitioner with flu-like illness and left supraclavicular swelling of uncertain nature, without other symptoms. An ultrasound of the neck detected many enlarged lymph nodes in the left supraclavicular region, and a chest X-ray showed left mediastinal enlargement. Subsequent Computed Tomography scan of the chest and abdomen confirmed the presence of many enlarged lymph nodes in the neck, mediastinum and liver, and a FDG-PET/CT scan showed multiple scattered consolidation lesions involving also the bones. The diagnosis of classical Hodgkin’s lymphoma, nodular sclerosis subtype, was made on a subsequent cervical lymph node biopsy.
Key words
Hodgkin's lymphoma, nodular sclerosis CHL (NSCHL), asymptomatic lymphadenopathy
Introduction
The modern classification of Hodgkin’s disease was introduced by Lukes and Butler [1].
The Revised European American Lymphoma (REAL) classification in 1994 included Hodgkin’s lymphoma as one of the lymphoid neoplasms, and distinguished between 2 major types: nodular lymphocyte predominant Hodgkin’s lymphoma (NLPHL) and classical Hodgkin’s lymphoma (CHL). CHL was further classified into 4 subtypes: nodular sclerosis CHL (NSCHL), mixed cellularity CHL (MCCHL), lymphocyte-rich CHL (LRCHL), and lymphocyte-depleted CHL (LDCHL) [2].
The terminology recommended in the REAL classification was incorporated into the World Health Organization (WHO) classification of tumors of hematopoietic and lymphoid tissues, including the substitution of the term Hodgkin’s lymphoma for Hodgkin’s disease [3,4].
There are five types of Hodgkin lymphoma classified by the World Health Organization: nodular sclerosing, mixed cellularity, lymphocyte depleted, lymphocyte rich and nodular lymphocyte-predominant [3]. Clinical presentation of Hodgkin lymphoma [5] is the following:
- a) Asymptomatic lymphadenopathy may be present (above the diaphragm in 80% of patients);
- b) Constitutional symptoms (i.e., unexplained weight loss [>10% of total body weight], unexplained fever, night sweats) are present in 40% of patients; these are known as "B symptoms";
- c) Intermittent fever is observed in approximately 35% of cases;
- d) Chest pain, cough, shortness of breath, or a combination of those may be present due to a large mediastinal mass or lung involvement;
- e) Patients may present with pruritus; pain at sites of nodal disease, precipitated by drinking alcohol, occurs in fewer than 10% of patients but is specific for Hodgkin lymphoma;
- f) Back or bone pain may rarely occur.
A family history is also helpful; in particular, nodular sclerosis Hodgkin lymphoma (NSHL) has a strong genetic component and has often been previously diagnosed in the family. Hodgkin lymphoma is a potentially curable lymphoma.
Here the authors report a classical presentation of Hodgkin's disease in an otherwise healthy 27-year-old female.
Case report
In August 2015 an otherwise healthy 27-year-old female comes to the General Practitioner's office after experiencing flu-like symptoms with swelling on the left side supraclavicular region of the neck. Her past and recent medical histories were fine and no other remarkable co-morbidities were reported. Her family history was unremarkable.
The patient did not report any systemic symptoms including night sweats; weight loss or fever. The physical examination confirmed the presence of fixedlymph nodes of hard consistency in the left latero-cervical and supraclavicular area with an estimated size of 2.4 cm and without the evidence of any other superficial lymphadenopathy or organomegaly.
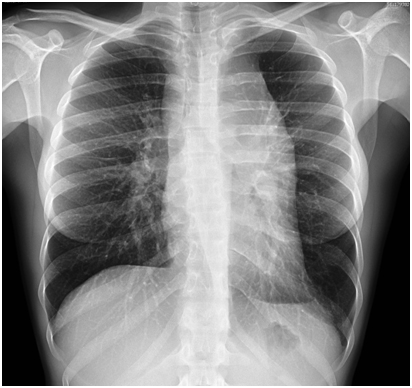
Subsequently laboratory test analysis were prescribed: complete blood count with differential, hepatic and renal function tests; protein electrophoresis; lactate dehydrogenase (LDH); serum electrolytes; protein electrophoresis; serology tests for Epstein-Barr virus (EBV), toxoplasmosis, HIV, and erythrocyte sedimentation rate (ESR); and C-reactive protein (CRP) inflammatory tests. An ultrasound exam of the neck and a chest X-ray were also prescribed. The biochemical results showed increased ESR and CRP as well as a neutrophilic leukocytosis of approximately 13,000 leukocytes per microliter. The neck ultrasound confirmed the presence of enlarged lymph nodes in the left supraclavicular side (2.4 × 1.3 cm) of the neck, with pathological aspects that were consistent with a lymphoproliferative disorder. The chest X-ray showed a left mediastinal enlargement (Figure 1).
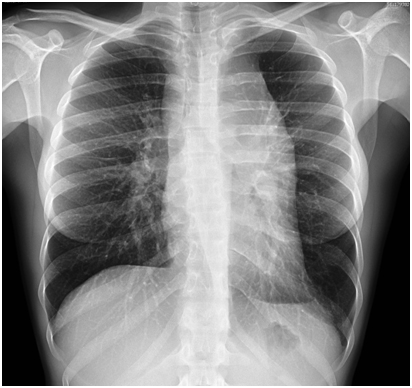
Figure 1. Chest X-ray showed a marked left mediastinal enlargement.
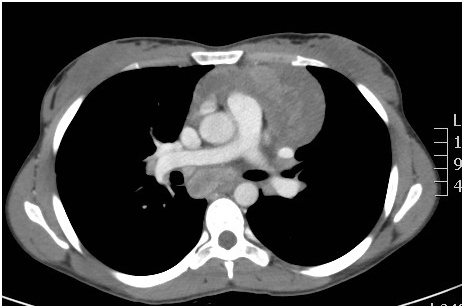
To accelerate diagnostic procedures the patient was admitted to the internal medicine department. Chest Computed Tomography (Figure 2) showed enlarged nodes in the left supraclavicular and cervical regions, in the upper mediastinum including paratracheal prevascular, subcarinal, bilateral lung hilum sites, and bilaterally in the axillas. The largest node was 10 × 5 cm in diameter.
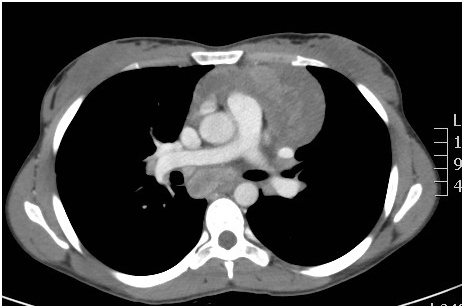
Figure 2. Chest CT scan showed enlarged nodes in the supraclavicular and cervical regions, in the upper mediastinum including paratracheal prevascular, subcarinal, bilateral lung hilum sites, and bilaterally in the axillas.
The spleen was normal buta focal liver lesion of 3 × 2.7 cm inside the 4th segment was detected. Also a FDG-PET/CT scan (Figure 3) confirmed the presence of multiple pathological accumulations of enlarged lymphoadenopathy already described, but also more skeletral localizations.
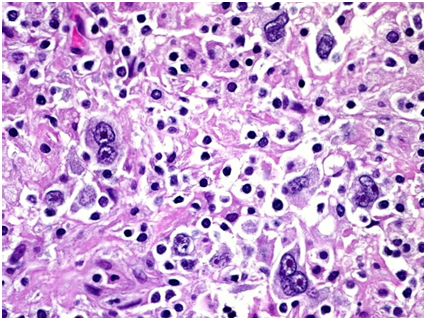
Figure 3. FDG-PET/CT scan revealed marked hypermetabolic nodes bilaterally in the laterocervical, supraclavicular and axillary regions, in the mediastinum, and within the left para-aortic space. The spleen was normal. An area of slightly increased glucose metabolism was also described in the IV° segment of the liver.
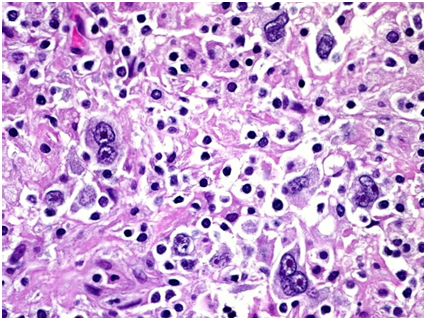
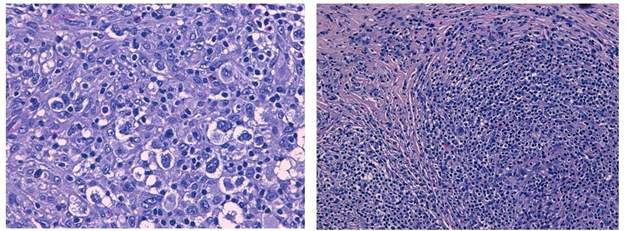
Supraclavear lymph node biopsy, histologic examination and immunohistochemical analysis made the diagnosis of classical Hodgkin’s lymphoma (nodular sclerosis subtype) by finding the diagnostic Reed-Sternberg cells and CD30 positive (Figure 4).
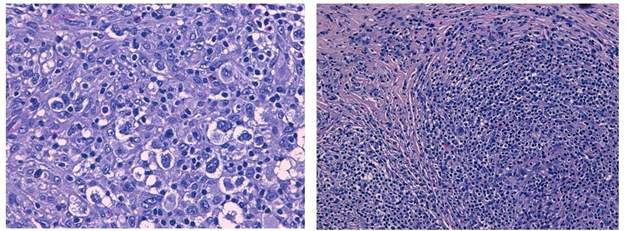
Figure 4. The histologic examination of lymph node biopsy specimens showed Reed-Sternberg cells and CD30 positive
Finally, a bone marrow biopsy was done but was negative for lymphoma. Based on the complete staging workup the final diagnosis for this 27-year-old patient was classical HL, nodular sclerosis, stage IV A. Her international prognostic score was 1 due to the advanced stage.
Discussion
Usually Hodgkin’s lymphoma occurs in the mediastinum and head and neck regions but its presentation may be insidious. Therefore the diagnosis could be tardive.
Because Hodgkin lymphoma is considered a curable malignancy and the differential diagnosis is broad, medico-legal problems may arise from failure to diagnose the disease in a timely manner, possibly due to the following factors: 1)The misinterpretation of B symptoms; A lack of follow-up for abnormal chest radiographs or physical examination findings; 3) A missed pathologic diagnosis because a needle biopsy was obtained rather than an excisional lymph node biopsy [6].
As this case study reportsa histologic diagnosis of Hodgkin lymphoma is always required. An excisional lymph node biopsy is recommended because the lymph node architecture is important for histologic classification.
Furthermore, the Ann Arbor classification [7] is used most often for Hodgkin lymphoma, as follows:
- Stage I: A single lymph node area or single extra-nodal site
- Stage II: 2 or more lymph node areas on the same side of the diaphragm
- Stage III: Lymph node areas on both sides of the diaphragm
- Stage IV: Disseminated or multiple involvement of the extra-nodal organs
2021 Copyright OAT. All rights reserv
Based on the clinical scenario, staging and degree of end-organ damage in patients with HL can be categorized into the following 3 groups:
- Early-stage favorable
- Early-stage unfavorable (bulky and non-bulky)
- Advanced-stage (this classification has impact in treatment selection and must be performed carefully in every patient with HL)
Our patient was promptly investigated and diagnosis of HL was timely. She was affected by Hodgkin's Disease (Nodular sclerosis classic HL) in advanced-stage (Stage IVA), but her prognostic score, based on the IPS score, can be categorized at good risk (IPS 0-1) [8].
In conclusion, this case report is anecdotal but emblematic because it stresses once again the importance of early diagnosis, staging and risk stratification of Hodgkin's disease in primary care settings and internal medicine, to improve the survival rate of patients.
Acknowledgements
The authors thank Dr. Luca Riccioni, pathologist, for his courtesy.
Disclosure
The authors declare no conflict of interest.
References
- Lukes R, Butler J, Hicks E (1966) Natural history of Hodgkin’s disease as related to its patholgical picture. Cancer 19: 317–344
- Harris NL, Jaffe ES, Stein H, Banks PM, Chan JK, et al. (1994) A revised European-American classification of lymphoid neoplasms: a proposal from the International Lymphoma Study Group. Blood 84: 1361–1392. [Crossref]
- Jaffe ES, Harris NL, Stein H, Vardiman JW (2001) Pathology and Genetics of Tumours of Haematopoietic and Lymphoid Tissues. IARC Press, Lyon, France.
- Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, et al. (2008) WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues. International Agency for Research on Cancer, Lyon, France.
- Eichenauer DA, Engert A, Dreyling M, ESMO Guidelines Working Group (2014) Hodgkin's lymphoma: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 6: iii55-58. [Crossref]
- NCCN Clinical Practice Guidelines in Oncology: Hodgkin Lymphoma. Version 2.2015. National Comprehensive Cancer Network.
- Carbone PP, Kaplan HS, Musshoff K, Smithers DW, Tubiana M (1971) Report of the Committee on Hodgkin's Disease Staging Classification. Cancer Res 31: 1860–1861. [Crossref]
- Hasenclever D, Diehl V (1998) A prognostic score for advanced Hodgkin's disease. International Prognostic Factors Project on Advanced Hodgkin's Disease. N Engl J Med 339: 1506-1514. [Crossref]