Abstract
Background
Cool Teens is a computerised cognitive behavioural therapy (CCBT) program designed for anxious adolescents that has demonstrated efficacy in a university clinic.
Aims
The effectiveness of this program in real world settings has not been evaluated. This study aimed to examine the benefits and acceptability of using CCBT in a community mental health setting.
Method
An adolescent girl (aged 16) with anxiety completed CCBT as a first step to therapy in a community mental health setting. She completed the program on her home computer supported by brief therapist phone calls. Further face-to-face sessions were provided post-CCBT and focused on practicing the skills learnt in CCBT. Self-reported adolescent anxiety was measured pre-treatment, post-CCBT, post-face-to-face therapy, and at 3 month follow up. The participant and therapist also provided feedback on the CCBT program and its usefulness at post-treatment.
Results
Changes in self-reported anxiety scores over time were observed for CCBT, with further reductions after face-to-face therapy. Both the adolescent and therapist reported positive benefits to using CCBT as the first step in treatment, and identified few barriers.
Conclusions
CCBT is a promising first step in treatment that can be utilised in community mentalhealth settings with the likely benefits of increased user satisfaction (due to decreasing in therapy waiting times) and reduced therapist time per client.
Key words
adolescent, anxiety, computerized cognitivebehavioral therapy, stepped-care, translation
Introduction
Anxiety disorders are common in adolescents and left untreated can predict anxiety and depression in adulthood [1-3]. Cognitive behavioral therapy (CBT) has been shown to be effective in treating adolescent anxiety in individual and group treatment formats[4,5].Computerized cognitive behavioral therapy (CCBT) treatments for anxiety disorders in adolescents are emerging and have demonstrated efficacy in university settings. The Cool Teens program has previously been demonstrated to be efficacious in a pilot case series and in a randomized controlled trial[6,7]with 41% of adolescents being free from their primary anxiety disorder at post-treatment. The BRAVE ONLINE program for anxious adolescents has also been shown in case studies [8]and in a randomized controlled trial to be efficacious in reducing adolescent anxiety [9]with 34% diagnosis free at post-assessment, and with impressive outcomes at 1 year follow-up with 78% being free from their primary anxiety disorder. In fact, Spence et al.[9]reported that online CBT was equivalent to face-to-face individual CBT for anxious adolescents, suggesting that CCBT holds great promise for treating anxious adolescents in the future.
Both of these computerized programs focus on core CBT anxiety management skills such as: psycho-education, cognitive restructuring and graded exposure and use written information, exercises, cartoons and homework to teach and practice the skills. Both programs are also supported by the adolescent’s parent and a therapist who calls the family regularly throughout the program to offer motivation, support and answer any questions about the skills as needed. These programs typically require minimal therapist time either delivered over the phone or over the internet. For example, in the Cool Teens program a maximum of 3 hours telephone time per family is required. As a result, these programs offer alternative treatment formats for adolescents with anxiety that might be particularly useful where access to face-to-face treatments is difficult to access, such as in rural areas, or when access to services is limited due to waiting periods. These CCBT programs also have the ability to reduce service use costs by requiring less therapist time [10].
Long waiting times exist for mental health services in many areas including child and adolescent mental health, with a mean waiting period in Canada of 30 days for high priority cases and 109 days for low priority cases [11]. Further shortages in clinicians trained in delivering face-to-face CBT exist worldwide. With preliminary studies suggesting around 40% of adolescents would be recovered from their anxiety disorder after CCBT, computerized CBT programs may be useful to treat a large number of adolescents with less therapist time needed e.g. with <3 hours per participant[7].However, current results suggest that approximately 60% of adolescents would still meet criteria for their primary anxiety disorders after CCBT. Therefore, they would need to go on to receive further assistance. What this additional assistance should be is not known. However, it is possible that CCBT could be followed by additional face-to-face CBT. This recommendation is based on an assumption that the CCBT approach failed for a reason that might be overcome with face-to-face therapy. The sorts of reasons for treatment failure that might be tackled in face-to-face CBT might be things like: failure to complete the program, failure to implement the skills, failure to understand the skills, or failure to do sufficient exposure to feared stimuli.
Such a stepped approach might result in cost savings and reduced waiting times as a clinician could manage a larger caseload of CCBT cases with shorter phone calls needed. Further, although it is currently untested, subsequent face-to-face therapy time might be reduced after an adolescent has completed CCBT and learned some of the basic skills. While the existing CCBT programs for anxious adolescents provide promising options for wide spread, low cost treatment, no research has specifically examined their effectiveness in community mental health settings or if they can be used in a stepped care model as a step before face-to-face CBT. With the United Kingdom seeking to extend the Improved Access to Psychological Therapies for children and adolescents in the near future year, and other countries likely to follow, research examining the effectiveness of computerized CBT interventions in real world settings and as a first step in therapy is desperately needed. It is also not known what barriers or benefits might exist to using CCBT as a first step, followed by face-to-face CBT for adolescents whose anxiety was not resolved after CCBT.
This study starts to bridge this gap and presents a case study of the first adolescent to use this program in a stepped care approach in a community based child and adolescent mental health service. The paper presents changes in self-reported adolescent anxiety at each step of treatment, as well as feedback from the adolescent about the barriers to treatment and user preferences of using the Cool Teens program as a first step to face-to-face CBT in a community mental health setting. Finally, the paper presents the therapist’s feedback on using this program in this setting in this way.
Method
Participants
AB was a 16 year old female of white British background and middle income from an urban area. The family reported that her maternal aunt was a “worrier”, but there was no other significant family psychiatric history. She presented to the local community mental health center for difficulties related to anxiety with a history of four years duration. She reported excessive worry in a number of areas. She specifically worried about her own and the health of others (family members), with an overwhelming sense of responsibility for the safety and welfare of both herself and others. For example, AB would express concerns that she could “accidentally” drink too much water and harm herself in this way. She also worried that she could contract lead poisoning by “accidentally” putting her pencil in her mouth. In addition, she was concerned over her mother’s safety when her mother had to travel long distances, and she was worried that she also worried too much. In addition, she reported anxiety on separating from her mother or from her home. As a result she was unable to stay home alone, attend sleep-overs, had difficulty going to sleep on her own, and was very worried whenever her mother had to be away from home. Although a formal diagnostic instrument was not used (as this was not standard practice in the mental health service), based on clinical assessment using the Diagnostic and Statistical Manual 4th Edition (DSM-IV) criteria she met criteria for a primary diagnosis of Generalized Anxiety Disorder, and features ofSeparation Anxiety Disorder. AB reported no other significant mood or psychiatric difficulties.
Materials
Questionnaires
Spence Children’s Anxiety Scale–Child Version(SCAC-C:Spence, 1998). Pre- and post-treatment anxiety symptoms at each treatment step were measured using the SCAS-C. This 45-item measure assesses adolescent reports of anxiety symptoms, closely corresponding to those in the DSM-IV, using a four point Likert scale (0 = “Never”, 3 = “Always”) and has six subscales: generalized anxiety, separation anxiety, obsessive compulsive, panic/agoraphobia, social anxiety, fears of physical injury. It has good psychometric properties with respect to reliability and validity and has been normed in adolescent populations [12-16].
Barriers to Treatment. To gauge the barriers to treatment of the Cool Teens program a short questionnaire was used that had been previously developed for evaluating the Cool Teens program in a case series and randomized controlled trial [6,7,17]. The scale had 10 questions about the delivery of computerized treatment (e.g., “Finding time to use the CD-ROM was difficult”, “I had technical problems with the CD”). Questions were answered using a scale from 1 (“Never a problem”) to 5 (“Very often a problem”).
Preferences and Attitudes Questionnaire. This questionnaire was previously developed for evaluating the program[6,7,17], and asked the participant to list their likes and dislikes about the Cool Teens program and to rate each of the multimedia components (e.g. videos, voiceovers) on a 5-point scale (“Very Bad” to “Very Good”), and the eight CBT modules on a 4-point scale (“Very Useful” to “Not Useful”).
CBT Program
The Cool Teens is a computerized program based on the Cool Kids anxiety management program and teaches cognitive behavioral therapy techniques for managing anxiety in 8 therapy modules of 30 minutes, with a strong focus on cognitive restructuring and graded exposure. The content of the 8 modules is shown in Table 1 [7,10,18-20]. The program uses a combination of multi-media formats (text, audio, illustrations, cartoons, and live video) to deliver information, examples, activities, and homework in an engaging way. The program includes 6 video case studies of adolescents discussing different anxiety problems and applying skills to their particular problem. Although an internet version of the program is currently being developed, in this trial the program was delivered using a password protected CD-ROM sent to the adolescent to use at home. Adolescents are supported by their parent and by therapist calls to the adolescent and parent. Brief parent handouts provide an overview to parents of the core strategies (psycho-education, goal setting, and graded exposure) so that they can support their adolescent; however, the parents have a minimal role. The program is generally used over a 12 week period. The Cool Teens program is designed to be supported by brief regular therapist phone calls to the adolescent and parent. In previous trials [6,7], the total duration of phone calls to the family was less than 3 hours.
Module 1 |
Module 2 |
Module 3 |
Module 4 |
Module 5 |
Module 6 |
Module 7 |
Module 8 |
Understanding Anxiety:
-Psychoeducation |
Setting Goals:
-Goal Setting |
Realistic Thinking I:
-Linking thoughts and feelings
-Identifying unrealistic thoughts
-Challenging unrealistic thoughts |
Step Ladders I:
-Introduction to graded exposure
-Creating the first step ladder |
Step Ladders II:
-Creating additional step ladders
-Problem solving barriers and difficulties |
Realistic Thinking II:
-Extended challenging unrealistic thoughts
-Realistic Thinking on the go (doing it in your mind) |
Coping Skills:
-Problem Solving
-Adaptive Coping Skills (Calming Activities)
-Avoid unhelpful coping |
Treatment Maintenance and Relapse Prevention:
-Review progress
-Set new goals
-Review skills learned |
Table 1. Skill Content Cool Teens Program
In this case study, the adolescent and her mother received a total of 5 fortnightly phone calls of approximately 20 minutes duration (5 minutes with the mother and 15 minutes with the adolescent) with a total family phone call duration time of less than 2 hours. The phone calls focused on AB’s specific questions regarding application of the skills taught in the program, as well as encouragement for her to continue with the program. The calls to the mother focused on psychoeducation, goal setting and how to support graded exposure. Her therapist for both the Cool Teens component was an experienced clinical psychologist.AB competed all of the modules and was able to implement the skills on her own with some success. However, during the CCBT program she was able to address minor worries and health worries such as: “I didn’t drink enough water today”, but found her thought “I can cope” very difficult to challenge on her own. She was also only able to face “small” fears such as: staying on her own at home for short periods of time (fear of being burgled), socializing more with friends, and waiting for her mum to pick her up in town after her friends had already left. She was too afraid to try larger fears on her own due to a strong fear that she wouldn’t be able to cope.
Face-to-face therapy
After the adolescent completed the Cool Teens program the adolescent continued to score highly on the anxiety measures and so she was offered face-to-face sessions with the same therapist. Because the adolescent had already completed Cool Teens she already understood the basics of anxiety and cognitive behavioral therapy and so face-to-face therapy spent little time on introductory concepts such as psycho-education, basic cognitive skills such as identifying thoughts, and introducing graded exposure and safety behaviors. Instead, face-to-face therapy initially consisted of establishing a case formulation to work out what areas needed further work and which CBT skills would be used to address these. AB and the therapist decided that further work was needed to build AB’s skills in cognitive restructuring and graded exposure. AB therefore was supported by her therapist to continue to practice skills for identifying and challenging irrational thoughts, particularly for her worry that “I can’t cope on my own”. She also extended the steps that she had achieved in the graded exposure component of the Cool Teens program. In particular she needed therapist support to motivate her to take big steps to overcome her fears of doing things on her own such as: staying home alone for extended periods of time, walking to school with a friend, and then on her own, and going to the shopping mall on her own, while reducing reassurance seeking from her mother. Finally, she worked on extending graded exposure to incorporate invivobehavioral experiments, for example, testing whether she would get lead poisoning by putting a pencil in her mouth (with the benefit of the therapist also demonstrating this step). AB was seen for 7 weekly sessions followed by 3 fortnightly sessions and 3 monthly sessions before termination. The number of face-to-face sessions was not predetermined, and the clinician followed standard practice in the community mental health center which was to space out final sessions and terminate when the client and therapist had agreed that the client’s anxiety was no longer causing significantly life interference.
Procedure
Ethical approval was gained for the study. Both adolescent and parental written and informed consent were obtained. AB conducted intake and was placed on the community mental health wait list for face-to-face CBT. She was offered access to the Cool Teens program supported by therapist calls due to her primary anxiety problems. AB completed the SCAS-C, and began the Cool Teens program on her home computer.AB and her mother received 5 fortnightly phone calls from the therapist to support her during the program. At the end of the program, AB completed the SCAS-C, and the Barriers to Treatment and User Preferences Scale regarding the Cool Teens program. AB then completed 13 sessions of individual face-to-face CBT and recompleted the SCAS-C at post-individual treatment and at 3 months follow up.
Results
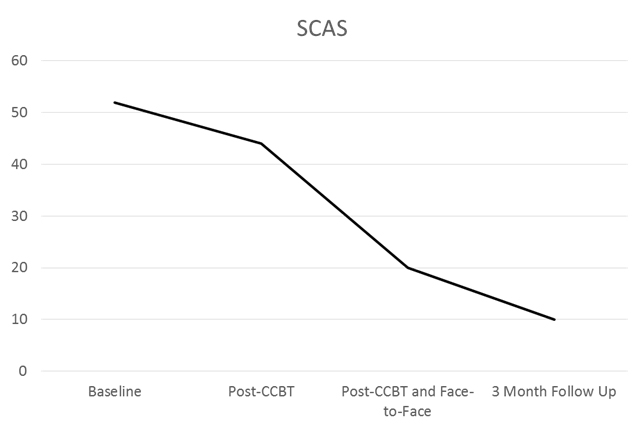
AB’s rawscores on the SCAS-C and z-scores (converted using population means and standard deviations (SDs)) are reported[12] (Table 2). At baseline her total score was 52 (z-score = 1.71) which was more than 1.5 SDs above the population mean. At post-CCBT, her total score was 44 (z-score = 1.07), a 0.7 SD decrease in anxiety, reflecting a moderate to large effect size change; however this score was still more than 1SD above the population mean. At post-CCBT, AB had a total score of20 (z-sore = -0.45) which is in the normal range, and her score remained in the normal range, 10 (z-score -1.09) at the 3 month follow up (Figure 1).
|
Baseline |
Post-CCBT |
Post-CCBT and Face to Face |
3 Month Follow Up |
SCAS Total |
52 (1.71)* |
44 (1.07)^ |
20 (-0.45) |
10 (-1.09) |
Table 2. Changes in Scores on the Spence Child Anxiety Scale over Time (Z-Scores in Brackets)
Note: * = >1.5 standard deviations above the population mean, ^ = >1 standard deviation above the population mean
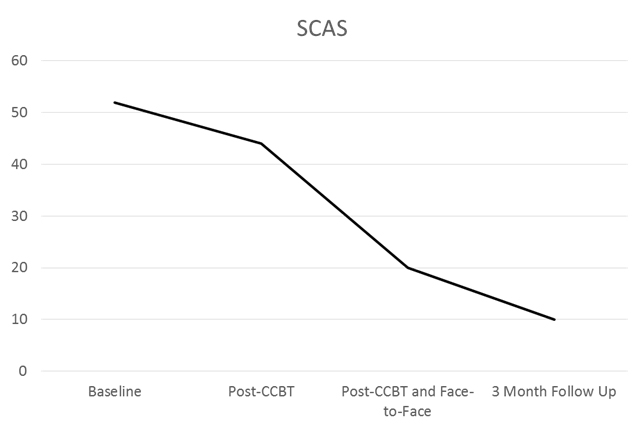
Figure 1. Change in scores on the Spence Child Anxiety Scale over time
Note: CCBT = Computerzed Cognitive Behavioral Therapy, GAD = Generalized Anxiety Disorder, OCD = Obsessive Compulsive Disorder
Feedback from the client and therapist was that CCBT was useful. AB reported that CCBT: reduced her anxiety, ‘helped me to get a better understanding of the basic CBT principles’ and helped her to feel that she wasn’t ‘abnormal’. The therapist reported several benefits of the stepped care approach including reduced waiting time (AB was able to start using CCBT immediately when a 3 month waiting list existed for face-to-face CBT in this clinic) and some improvements in anxiety with CCBT alone. The therapist also reported that he felt that subsequent face-to-face therapy was more efficient, as AB learnt the basics of CBT using the Cool Teens program with only 2 hours of therapist time needed. For example, at the start of face-to-face therapy, AB already had a good understanding of psycho-education of anxiety, linking thoughts and feelings, and the process of graded exposure, and these concepts did not need to be covered again, so therefore they were able to start face-to-face sessions with an immediate focus on graded exposure and therapist-led exposure to tackle her greatest fears.
On the Barriers to Treatment and User Preferences and Attitudes Scales AB reported few barriers to the CCBT program. She reported the following were ‘never’ or ‘occasionally’ a problem: technical problems, understanding content, privacy/security issues, not having enough therapist support, difficulty understanding the skills and homework. She reported she ‘sometimes’ lost interest with the program and found it boring. She reported the biggest barriers were finding time to use the program (‘often’), and not wanting to do the tasks (‘very often’). She reported that she most liked the psycho-education module and found it ‘very useful’, but rated the two graded exposure modules as ‘not useful’.
Conclusions
This case study is the first examination of CCBT used in a stepped care model with face-to-face therapy to treat anxiety in an adolescent community mental health setting. This study builds on previous research conducted using CCBT in university settings in which 41% of participants no longer met criteria for their primary anxiety disorder after completing the Cool Teens program with 3 hours of therapist support [7]. These results are similar to the findings from the BRAVE ONLINE program, in which 34% of adolescents didn’t meet criteria for their primary disorder after completing the program [9]. Although in this case study, AB required further treatment after completing CCBT, it is likely that if computerized programs were to be more routinely delivered to adolescents on waiting lists for face to face therapy that around 35-41% wouldn’t need any further treatment at the conclusion of the CCBT program. Further, in this case, the therapist’s opinion was that CCBT shortened the length of additional face-to-face therapy for this very anxious adolescent. Therefore with potentially 41% of cases able to be treated with CCBT alone, and further cases potentially needing less face-to-face sessions than usual, this combined approach has the potential for cost savings (with reduced therapist costs), and reduced waiting times as was found in this case (AB was able to be seen 3 months earlier than usual). Therefore using CCBT in adolescent mental health services might lead to great cost cutting benefits as well as reducing waiting times.
In terms of barriers to treatment using the Cool Teens program, the therapist reported no barriers, and few barriers were reported by the adolescent. The main barriers that she identified were that she had trouble finding time to do the CCBT program and that she didn’t like having to do the homework tasks. These findings replicate the same barriers identified in other trials of the program, but are unlikely to be specific to this program and are consistent with barriers common in CBT programs with adolescents in general [17].Innovative methods for reducing homework and shortening treatments would be useful steps forward. AB identified that the psycho-education module was the most helpful, but she reported that the graded exposure modules were the least helpful. As graded exposure is a core anxiety management skill it is problematic that AB was not engaged with this skill. Although this has not been reported as a major barrier in other evaluations of this program, it is likely that AB did not make as much progress in CCBT due to her belief that exposure was not helpful. It is likely that because AB engaged in a lot of reassurance seeking behaviors, that implementing graded exposure on her own was particularly difficult as she needed to both approach the fear but also stop the reassurance seeking.
Face-to-face therapy after CCBT mainly focused on encouraging AB to complete exposure and involved in-session therapist-lead exposure that is likely to have led to the further reductions in anxiety. AB was unable to push herself to face her biggest fears without the face-to-face encouragement of her therapist, who also assisted by demonstrating some of the steps, e.g. putting a pencil in his mouth (fear of lead poisoning), and helping her to do invivoexposure in session. This is a common problem in therapy, motivating a client to face their fears in graded exposure, but perhaps was made more difficult with CCBT rather than face to face therapy in which invivo exposure is easier to conduct. This might be particularly true when the adolescent is not that keen to give up anxious behaviors, and when family factors such as excessive reassurance from parents can produce barriers to achieving effective graded exposure. Future developments with CCBT would need to focus on incorporating more motivation enhancement strategies, and perhaps including skype calls to encourage invivoexposure during sessions.
Limitations of this study include that this is a single case study, and that anxiety symptoms were only measured with adolescent self-report. This occurred because it is standard practice for evaluating treatment outcomes in this community service to only use adolescent self-report. More research with larger numbers of cases, structured diagnostic interviews at pre and post treatment, and measures of parental reported adolescent anxiety is needed to further these promising initial findings. This study does, however, demonstrate the feasibility of CCBT programs in adolescent community mental health settings and suggests that CCBT is a promising way forward that could reduce waiting times and therapist costs. Feedback from both the adolescent and therapist about using CCBT in an adolescent community mental health service was positive and few barriers were identified to using CCBT as a first step to treatment. More research is needed with larger numbers to evaluate the effectiveness of CCBT when delivered by both specialist and generalist mental health workers in these settings.
Acknowledgement
Thanks to the client and her family for providing access to her data.
Conflict-of-Interest Statement
2021 Copyright OAT. All rights reserv
NM was the therapist for this case.
References
- Hofstra MB, van der Ende J, Verhulst FC (2002) Child and adolescent problems predict DSM-IV disorders in adulthood: a 14-year follow-up of a Dutch epidemiological sample. J Am Acad Child Adolesc Psychiatry41: 182-189.[Crossref]
- Rapee RM, Schniering CA, Hudson JL (2009) Anxiety disorders during childhood and adolescence: origins and treatment. Annu Rev Clin Psychol5: 311-341.[Crossref]
- Woodward LJ, Fergusson DM (2001) Life course outcomes of young people with anxiety disorders in adolescence. J Am Acad Child Adolesc Psychiatry40: 1086-1093.[Crossref]
- Cartwright-Hatton S, Roberts C, Chitsabesan P, Fothergill C, Harrington R (2004) Systematic review of the efficacy of cognitive behaviour therapies for childhood and adolescent anxiety disorders. Br J Clin Psychol43: 421-436. [Crossref]
- James A, Soler A, Weatherall R (2005) Cognitive behavioural therapy for anxiety disorders in children and adolescents. Cochrane Database Syst Rev4.
- Cunningham MJ, Wuthrich VM, Rapee RM, Lyneham HJ, Schniering CA, et al. (2009) The Cool Teens CD-ROM for anxiety disorders in adolescents : a pilot case series. Eur Child Adolesc Psychiatry18: 125-129.[Crossref]
- Wuthrich VM, Rapee RM, Cunningham MJ, Lyneham HJ, Hudson JL, et al. (2012) A randomized controlled trial of the Cool Teens CD-ROM computerized program for adolescent anxiety. J Am Acad Child Adolesc Psychiatry 51: 261-270.[Crossref]
- Spence SH, Donovan CL, March S, Gamble A, Anderson R, et al. (2008) Online CBT in the treatment of child and adolescent anxiety disorders: Issues in the development of BRAVE-ONLINE and two case illustrations. Behav Cogn Psychother36: 411-430.
- Spence SH, Donovan CL, March S, Gamble A, Anderson RE, et al. (2011) A randomized controlled trial of online versus clinic-based CBT for adolescent anxiety. J Consult Clin Psychol 79: 629-642.[Crossref]
- Wuthrich VM, Cunningham MJ, Rapee RM (2013) Cool Teens: A computerized intervention for anxious adolescents. In: Essau CA, Ollendick TH (Eds.), The Wiley-Blackwell Handbook of the Treatment of Childhood and Adolescent Anxiety (1stedn), Chicester, Great Britain: John Wiley & Sons, Ltd.
- Kowalewski K, McLennan JD, McGrath PJ (2011) A preliminary investigation of wait times for child and adolescent mental health services in Canada. J Can Acad Child Adolesc Psychiatry 20: 112-119.[Crossref]
- Essau CA, Sasagawa S, Anastassiou-Hadjicharalambous X, Guzman BO, Ollendick TH (2011) Psychometric properties of the Spence Child Anxiety Scale with adolescents from five European countries. J Anxiety Disord25(19-27). [Crossref]
- Muris P, Merckelbach H, Schmidt H, Gadet BB, Bogie N (2001) Anxiety and depression as correlates of self-reported behavioural inhibition in normal adolescents. Behav Res Ther 39: 1051-1061.[Crossref]
- Muris P, Schmidt H, Merckelback H (2000) Correlations among two self-report questionnaires for measuring DSM-defined anxiety disorder symptoms in children: the Screen for Child Anxiety Related Emotional Disorders and the Spence Children's Anxiety Scale. Personality and Individual Differences 28: 333-346.
- Spence SH (1998) A measure of anxiety symptoms among children. Behav Res Ther36: 545–566. [Crossref]
- Spence SH, Barrett PM, Turner CM (2003) Psychometric properties of the Spence Children's Anxiety Scale with young adolescents. J Anxiety Disord 17: 605-625.[Crossref]
- Cunningham MJ, Wuthrich VM (2008) Examination of Barriers to Treatment and User Preferences With Computer-based Therapy Using The Cool Teens CD for Adolescent Anxiety. E J Appl Psychol4: 12-17. [Crossref]
- Cunningham MJ, Rapee RM, Lyneham HJ (2006a) The Cool Teens CD-ROM: A multimedia self-help program for adolescents with anxiety. Youth Studies Australia25: 50-56.
- Cunningham MJ, Rapee RM, Lyneham, HJ (2006b) Feedback to a prototype self-help computer program for anxiety disorders in adolescents. Australian e-Journal for the Advancement of Mental Health5. Retrieved from www.auseinet.com/journal/vol5iss3/cunningham.pdf
- Lyneham HJ, Wuthrich VM, Rapee RM (2010) The Cool Kids Child and Adolescent Anxiety Program Adaptation for Supported Bibliotherapy Therapist Manual. Sydney: Centre for Emotional Health, Macquarie University.