Abstract
Medical lasers for various clinical procedures including dermatology and plastic surgery, wound healings, nerve stimulation, dentistry, cancer therapy, and ophthalmic surgeries are reviewed. The fundamental principles behind the technologies are also presented. The laser spectra of UV (200-400) um, visible (400-700) nm, near-IR (700-2900) nm, and mid-IR (3-5) um having various penetration depths define invasive and noninvasive procedures. Diode lasers have been widely used in many surgical procedures including soft tissue cutting, coagulation and cancer thermal therapy. Various photosensitizers are presented in matching the laser absorption wavelengths. Finally, the principles and applications of photothermal therapy (PTT) and photodynamic therapy (PDT) are discussed in great details.
Keywords
lasers; medical applications; photothermal therapy; photodynamic therapy; dermatology; plastic surgery; wound healings; dentistry; cancer therapy; ophthalmology
Introduction
Lasers have been used for various medical procedures such as dermatology and cosmetic surgery [1-9], wound healings [10], nerve stimulation [11], dentistry [12,13] ophthalmology applications for vision corrections [14-16] and corneal deceases [17]. and many other therapeutic procedures. Combining the nanoparticles, diode lasers have been also used for cancer therapy [18], bio-sensing, bio-imaging, drug delivery and diagnostics of cancer cell [19-23].
Lasers in the near infrared (IR), wavelength of (750-1200) nm, have deeper tissue penetration depths than that of visible lasers. Therefore, near IR lasers are good candidates for procedures which need deep penetrations such as hair removal [6] and nano-gold mediated cancer therapy [18]. On the other hand, visible lasers (430 – 680) nm with strong absorption in blood and color-dyes have been used for phototherapy of oral cancer, retina deceases and tattoo removal [7]. Mid-IR lasers (1.9-3.0) um and (9.3 -10.6) um with strong absorption in water and tissue have been used for super surface procedures [3-8] or ablative type procedures such as soft and hard tissue ablation. Other IR lasers (1.3-1.6) um have been used for so called minimally invasive procedures such as resurfacing due to their smaller tissue absorption than that of mid-IR lasers [3,4].
In this review article, the fundamental principles behind the medical laser applications will be presented, including the laser spectra of UV (200-400) um, visible (400-700) nm, near-IR (700-2900) nm, and mid-IR (3-5) um having various penetration depths which define invasive and noninvasive procedures. Diode lasers for various surgical procedures including soft tissue cutting, coagulation and cancer thermal therapy will be reviewed. Various photosensitizers are presented in matching the laser absorption wavelengths. Finally, the principles and applications of photothermal therapy (PTT) and photodynamic therapy (PDT) will be discussed in great details.
Fundamentals
1)The basic definition and units
Most lasers are defined by their output “colors”, i.e, wavelength (or spectrum)
as follows:
UV (200-400) um, visible (400-700) nm, near-IR (700-2900) nm, and
mid-IR, (3-5) um, where 1 um=1,000 nm.
The output of a laser is defined by the following units:
Power (P) in mW (or W), 1W=1,000 mW.
Intensity (I) in mW/cm2 (power density per unit area).
Energy (E) in mJ; Fluence (F) in mJ/cm2 (energy density).
Relations: E=It , P=I/area, F=E/area
2)Laser-matter interaction
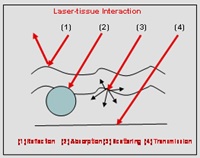
Laser-tissue (or other media) interaction, in general, could be categorized into three processes: (a) pure thermal, (b) non-thermal, and (c) combined thermal and non-thermal effects. As shown in Figure 1, laser can be reflected, absorbed, scattered or transparent to the matter. These processes are governed by not only the tissues (media) optical properties but also the laser parameters such as its wavelength, energy, intensity, pulse-width, repetition rate and the operation modes, continuous wave (CW) or pulsed mode. For example, an ablative Er:YAG laser operated at short pulse could become a thermal laser when it is operated at low power and/or long pulse; whereas a thermal laser at 1540-nm operated at long pulse could become an ablative, non-thermal laser when it is operated at very short pulse, say less than 10 picoseconds. Furthermore, laser at very short wavelength such as (154-193) nm, could ablate tissues without causing too much heat. Other short pulsed lasers can ablate matter via so-called plasma-assisted process. Various fiber structures for effective delivery of the laser energy to the treated areas are also critical in specific applications.
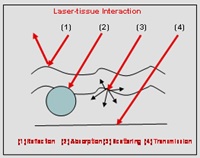
Figure 1. Laser can be reflected, absorbed, scattered or transparent to a matter.
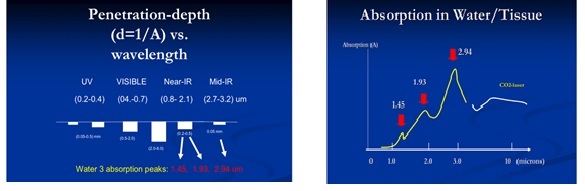
As shown in Figure 2 (top), tissue penetration depth (d) of various lasers depends on their wavelength, or their tissue/water absorption coefficients (A), where A is inverse proportional to d (i.e. d=1/A). Figure 2 (low) shows the absorption spectrum in water (or tissue) having 3 major peaks at 1.45 um, 1.93 um and 2.94 nm, besides the high absorption of CO2 lasers (9.6 to 10.6 um).
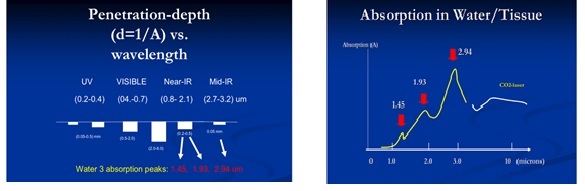
Figure 2. Tissue penetration depth (d) of lasers at various wavelength; the absorption spectrum in water (or tissue).
3)The coupling equations
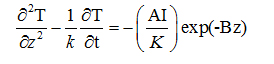
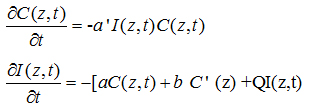
The key equations describing the laser-matter interaction may be governed by the following heat diffusion equation (for PTT) and kinetic equation (for PDT) [8,14,18]
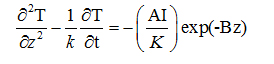
where T is the temperature of the absorbing medium; z is the laser propagation direction along the depth of the GNRs solution, k and K are, respectively, the thermal conductivity and diffusivity of the solution, I is the laser intensity (or power density), B is the extinction coefficient, which can be expressed by B=[A(A+2s)]1/2, where A and s are the absorption and scattering coefficient.
where C(z,t) is the concentration of the photosensitize; a’=ap is the coupling constant with p being the quantum yield for a type-I PDT process; Q is the tissue absorption coefficient; a and b are the extinction coefficient of the photosensitize and its photolysis products. Both analytic and numerical solutions of Eq. (1) and (2) have been presented by Lin et al [8,14] in cancer therapy and in photopolymerizations.
Medical Applications
Lasers have been used for various medical procedures including dermatology, plastic surgery, wound healings, nerve stimulation, dentistry, ophthalmology and many other therapeutic and surgical procedures [1-17]. Combining the nanoparticles and photosensitizers, diode lasers have been also used for cancer diagnosis and therapy [18-23]. Selected medical laser systems (devices) which have been commercialized or used for research are shown in Table 1 for both photodynamic and photothermal and applications, where pulsed lasers are in energy per pulse (mJ) and CW lasers are in power (W).
Laser type |
Wavelength (pulse width) |
Energy/power |
Ti:sapphire |
780 nm (p.s. and f.s.) |
(0.01 – 0.1) mJ |
Nd:YAG/YLF |
1064/1053 nm (n.s. and p.s.) |
(1.0 – 20) mJ |
Ho:YAG |
2100 nm (µs) |
(10 – 20) mJ |
Er:YAG |
2940 nm (µs) |
(10 – 20) mJ |
Fiber-laser |
0.5-3.2 microns (n.s-p.s) |
(0.05 – 0.1) mJ |
UV excimer laser |
193, 308 nm (ns) |
(5 -20) mJ |
Solid state laser |
213, 266, 532 nm (ns) |
(2-10) mJ |
Solid state laser |
430-1064 (cw) |
0.5 – 10 W |
Gas lasers |
413, 488, 580,647 nm (cw) |
0.5-10W |
Diode laser |
360 -2100 nm (cw) |
0.1 – 50 W |
Table 1: Laser candidates for various medical applications.
Photodynamics therapy (PDT)
Interaction of light (coherent or non-coherent) with cells may be categorized to:
(a) Endogeneous: direct absorbing by the constituents of the cells or tissue, and
(b) Exogeneous: light absorbed via the added photosensitizer, a process called photodynamics therapy (PDT) can be used to destroy cancerous or diseased cells and/or unwanted abnormal tissues.
PDT involves selective light (often low-power laser light or LED) absorption by the external chemical agent, or a PDT drug. As shown in Table 2, various dyes (drugs) have been developed at specific laser absorption wavelengths from visible to near-IR. The PDT drugs may be administered either intravenously or topically depending on applications. Three principal mechanisms have been proposed for the destruction of cells and tissues by PDT: localized cell damage by targeting on a specific organelle by a particular drugs, including apoptosis (localized in mitochondiria) and necrosis (localized in plasma membrane); vascular damage induced by PDT action. For example, the porphyrin-induced PDT produces a rapid onset of vascular blood flow stasis (stopping) and hemorrhage causing tumor cell death; and immunological response of PDT results a strong inflammatory reaction which contributes to tumor destruction.
Dermatology & Cancers |
- Early stage (micro-invasive) lung cancer
|
- Lung tumors (endobronchial, mesothelioma)
|
|
|
|
- Chronic skin diseases (psoriasis, vitiligo)
|
- Wound healing, oral cavity (anti-bacterial)
|
Ophthalmology |
- Age-related macular degeneration (AMD)
induced CNV |
- Pathologic myopia induced CNV
|
|
Table 2: Applications of photodynamic therapy (PDT).
The photochemical process of PDT for cell damage further involves 2 chemical processes: photoaddition reaction (type-I) in which the light-excited photosensitizer convalently bonds to a constituent molecule of the cell, where type I is the major path for crosslinking process; and photoxidation reaction (type-II) in which the excited state of the photosensitizer produces a highly reactive oxygen specie such as an excited singlet oxygen, a superoxide anion, or a free radical of H* and it often involves a chain reaction, where type II is the major path for cancer cell damage.
As shown in Table 2, PDT offers many applications in dermatology, ophthalmology and cancer treatments in various parts of human body.
As shown in Table 3, various photosensitizers are available for the absorption of lasers in visible (630-700) nm, and near-IR (700-1000) nm. These lasers are commercially available; dye lasers (at about 665 nm) pumped by a green laser; Nd:YAG (at 1064 nm); diode lasers (630-1100) nm; tunable Ti:sapphire laser (690-1100) nm; Alexandrite laser (720-800) nm. Tunable near-IR source may be also generated from an optical parametric oscillation (OPO) or amplification (OPA), where a green laser (at about 532 nm) may be used as a pump to produce tunable (900-1300) nm near-IR output (see Figure 3). In addition, high-brightness LED in visible (550-680) nm are also available for PDT using 5-ALA as the photosensitizer [24].
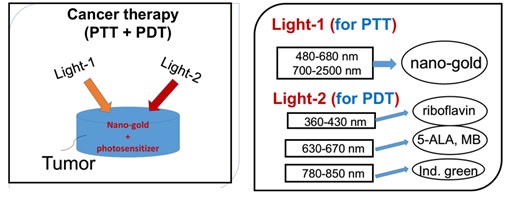
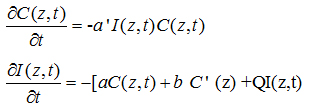
Figure 3. Combining PDT and PTT uisng nanogold and various photosensitizers [24].
Absorbing Extinction |
|
wavelength (nm) |
Coeff. (1/M/cm) |
Name of PDT drug |
- |
- |
Riboflavin (B2) |
365 |
- |
Photofrin (porfimer sodium) |
630 |
3,000 |
5-ALA |
635 |
5,000 |
Meta-THPC |
652 |
22,400 |
Methylene blue |
660 |
- |
pyropheophorbides (HPPH) |
665 |
- |
verteporfin |
680-690 |
- |
Lu-Tex |
732 |
42.000 |
Phthalocyanines (PTC), na-PTC |
670-780 |
100,000 |
Indocyanin green (ICG) |
805 |
- |
Si(IV)-naphthalocyanines |
770-790 |
240000 |
Table 3: Summary of photosensitizers [24].
High intensity ultra-short pulse lasers have been used in PDT using a 2-photon absorption. These include: mode-locked Ti:sapphire laser (at 800 nm), peak power about 5MW/cm2, pulse duration 70 fsec and energy of 4 nJ/pulse; mode-lock Alexandrite laser (at about 780 nm) and a near IR-laser called Cr:forsterite (at 1230 nm). These near-IR lasers at longer wavelength offers deeper penetration than that of visible lasers, in addition to the minimal thermal effects and spatial selectivity which may be important in certain treatments such as brain cancers.
Laser penetration of tissues is limited by its absorption in melanin and oxyhomoglobin and it is a decreasing function of laser wavelength. Therefore near-IR lasers have deep penetration than visible lasers and have been used in various therapies which require deep penetrations, such as laser for hair removal and laser for acupunctures [6].
For ophthalmic application, retinal photocoagulation has been reported by using various visible and IR lasers such as argon blue-green laser (488/514 nm), double-YAG green laser (at 532 nm), krypton laser (at 647 nm) and diode lasers (at 806-810 nm). Photocoagulation process was also used to seal leak blood vessels for the treatment of age-related macular degeneration (AMD) which has two types, the choroidal neovascular (“CNV”, wet) and non-neovascular (dry). In the wet AMD, the vascular ingrowth causes photoreceptor destruction, or bleeding with extensive loss of vision. The major drawback of photocoagulation to destroy the vascular growth beneath the retina is the nonselective necrotic damage to the adjacent normal retina and the thermal damage in the subfocal area which can cause the recurrence of the neovascular tissue. However, a short-pulse (about 3 ns) green laser has been successfully used for the treatment of open-angle glaucoma, a procedure called selective laser trabeculoplasty (SLT) which shows advantages over the conventional system using an argon cw laser.
PDT for the treatment of subfocal choroidal neovascularization (CNV) using verteporfin as the phtosensitizer has been proven for subfoveal. CNV in both AMD and in pathologic myopia (or non-AMD) patients. CNV may be also treated by a procedure called transpupillary thermotherapy (TTT) using diode laser at 810 nm, where PDT drug is not needed.
Photothermal therapy (PTT)
In contrast to the PDT without too much heat involved, photothermal therapy (PTT) is a thermal process with heat generated by the thermal lasers. Examples of PTT for various applications in cancer therapy, cosmetic and dermatology are presented as follows.
Cancer therapy lasers
Combining the nanoparticles, diode lasers have been also used for cancer therapy [18], bio-sensing, bio-imaging, drug delivery and diagnostics of cancer cell [19-20]. Various nanoparticles (gold, polymers, silica etc) have been explored for the use of surface plasmon resonance (SPR) including shapes in spheres, rods, boxes, cages and shells [8-11]. For example, by changing the shape of nanogold from sphere to nanorod, the absorption and scattering peaks change from visible (about 530 nm) to the near-infrared (NIR) regime (about 750 to 980 nm) [18]. Comparing to the visible light, light in the NIR regime offers the advantages of larger absorption and scattering cross sections and much deeper penetration depth in tissues [18]. The in vivo studies in animal and/or human cancer therapy shall include the non-uniform gold nanorod (NGR) concentration in the tumor, the multi-layer normal-cancer tissue medium with multiple thermal parameters, and the blood flowing of the laser-targeted areas. The design of multiple-wavelengths laser system shall partially overcome the issues of GNRs non-uniform and multiple thermal medium for a 3-dimensional-therapy, in which various absorption penetration depths are available via the fiber-coupled multiple-wavelength laser simultaneously targeting the cancer tumors [18].
Combining PDT and PTT using nanogold and various photosensitizers for cancer therapy is shown in Figure 4 [24]. The critical factors of the synergistic therapy efficiency to be discussed include: the concentration of the initiator (nanogold or photosensitizers) in the treated medium, the wavelength, energy and the irradiation period of the light applied to the medium.
Cosmetic and dermatology lasers [1-9]
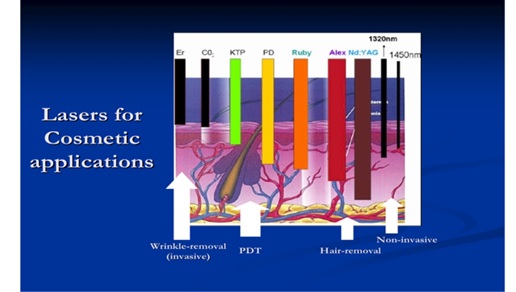
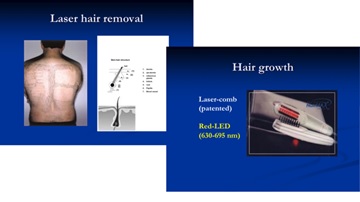
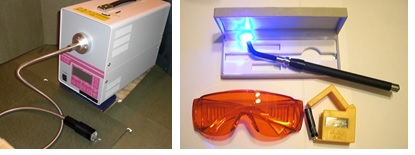
Figure 4 shows various cosmetic lasers and their applications for invasive and non-invasive uses defined by their tissue penetration depth (d). Lasers with small depth (d<0.1 mm) suitable for invasive wrinkle or tattoo removal, whereas large depth (with d> 2 mm) suitable for non-invasive simulation or hair removal. Figure 4 can be compared with Figure 2 for the penetration depth. Figure 4 shows the commercial laser for hair removal (using a diode laser at 810 nm with large penetration depth about 4 mm) and hair growth device (using a red, 635 -690 nm, LED or laser with smaller penetration depth and low power for surface stimulation). Figure 5 shows a UV (308 nm) light device for the treatment of psoriasis; and a pen-type blue laser (at 405 nm) combined with a red laser (at 660 nm) for the treatment of acne.
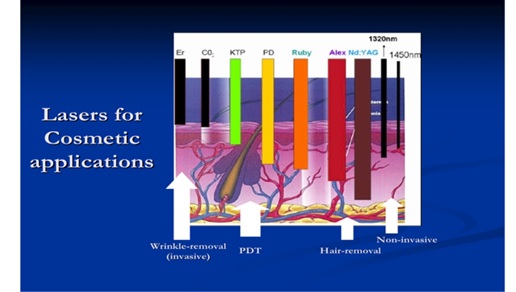
Figure 4. Cosmetic lasers and their tissue penetration depth which defined their applications in both invasive and non-invasive uses [5-9].
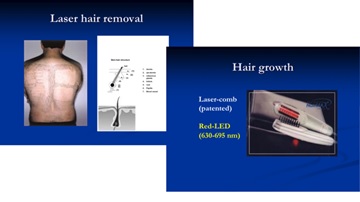
Figure 5. The commercial laser for hair removal (using a diode laser at 810 nm) and hair growth device (using a red, 635 - 690 nm LED or laser) [5,6].
Dental lasers [12,13]
Lasers (or LEDs) currently commercialized for dental applications include: (1) low power red laser (or LED, see Figure 6) activating methylene blue for antimicrobial photodynamic therapy (aPDT) to treat periodontal deceases; (2) diode laser (at 808 or 980 nm) for soft tissue cutting and stimulation; (3) Er:YAG laser, also called as “water-laser” (made by Biolase, US) for hard tissue cutting; (4) low power UV-blue laser (at 405 nm) for caries and cancer detection via light stimulated fluorescence.
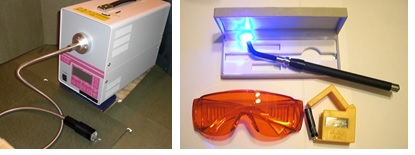
Figure 6. (Left) a UV (308 nm) light for the treatment of psoriasis; (Right) a pen-type blue laser (at 405 nm) for the treatment of acne (made by New Vision Inc.) [25].

Figure 7. (Right) power red laser (or LED) for antimicrobial photodynamic therapy (aPDT) and (Left) diode laser (at 808 or 980 nm) for soft tissue cutting [25].
Ophthalmology lasers [14-17]
As shown by Table 3, various lasers have been used for various ophthalmic applications including retinal photocoagulation using argon blue-green laser (488/514 nm), double-YAG green laser (at 532 nm), krypton laser (at 647 nm) and diode lasers (at 806-810 nm). Photocoagulation process was also used to seal leak blood vessels for the treatment of age-related macular degeneration (AMD).
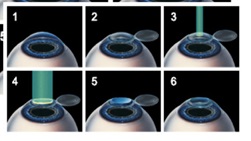
Figure 8 shows a surgical procedure called LASIK for vision corrections (myopia, hypeopia and astignism) using a UV excimer laser to reshape the corneal surface. Femto-second (f.s.) lasers combined with excimer laser are alo commercialized for the so-called bladeless LASIK procedure, in addition to the fetom-second laser cataracts treatment [16].
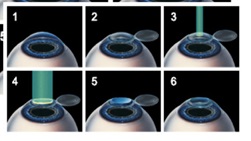
Figure 8. Surgical procedure called LASIK for vision corrections, where the corneal flap is prepare (either by microkeratom or a femtosecond laser), then an excimer UV laser (at 193 nm) is applied to cut a thin surface layer of the central part of the stroma tissue to reshape its curvature (for myopic correction); the corneal flat is placed back for healing [15,16].
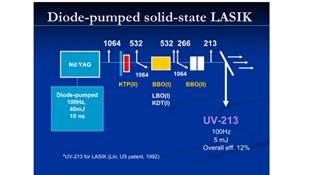
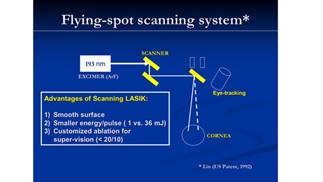
Figure 9 shows a patented system using a solid-state (213 nm) laser for PRK and LASIK in replacing the gas excimer laser, where nonlinear crystals are sued to convert the 1064 nm laser to its fifth harmonics at 213 nm. Figure 10 shows a scanning Lasik system using a small flying spot for customized vision corrections.
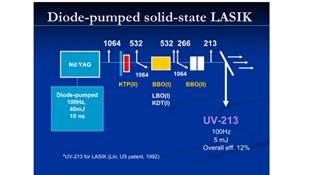
Figure 9. shows a patented system using a solid-state (213 nm) laser for PRK and LASIK (JT Lin, US 1992 patent) [14].
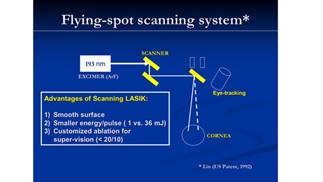
Figure 10. shows a scanning Lasik system using a small flying spot for customized vision corrections (JT Lin, US patent, 1993) [14-16].
Figure 11 shows a diode laser (at 808 or 980 nm) for photocoagulation of the corneal tissue for glaucoma treatment. Figure 12 shows two systems (made by New vision Inc. and MLase AG) using UV LED (at 365 nm) for corneal collagen crosslinking (CXL) for the treatment of keratoconus and other corneal deceases [17].

Figure 11. shows a diode laser (at 808 or 980 nm) for photocoagulation of the corneal tissue for glaucoma treatment, where a probe tip connected to the fiber is used to deliver the laser energy [25].

Figure 12. shows two systems (made by MLase AG, Germany, top; and New vision Inc. , Taiwan, low) using UV LED (at 365 nm) for corneal collagen crosslinking (CXL). Also shown is a pen-type CXL specially designed for VET uses [25].
Conclusion
Applications of medical lasers are characterized by the properties of the tissues and the matching absorption wavelengths. For PDT procedures, the properties of the activated photosensitizers also play an important role. Synergistic therapy efficiency may be improved by combining PDT and PTT using nanogold and various photosensitizers. Recent new technology also combines the nanomateirials for improved clinical outcomes.
References
- Zhang R, Ramirez-San-Juan JC, Choi B, Jia W, Aguilar G, et al. (2006) Thermal responses of ex vivo human skin during multiple cryogen spurts and 1,450 nm laser pulses. Lasers Surg Med 38: 137-141. [crossref]
- Tieny E, Hanke CW (2009) Randomized controlled trial: comparative efficientcy for the treatment of facial telagiectasias with 532 nm versus 940 nm diode laser. Lasers Surg Med 41: 555-562.
- Tark KC, Jung JE, Song SY (2009) Superior lipolytic effect of the 1,444 nm Nd:YAG laser: comparison with the 1,064 nm Nd:YAG laser. Lasers Surg Med 41: 721-727. [crossref]
- Thongsima S, Zurakowski D, Manstein D (2010) Histological comparison of two different fractional photothermolysis devices operated at 1,550 nm. Lasers Surg Med 42: 32-37.
- Maranda EL, Nguyen AH, Lim VM, Hafeez F, Jimenez JJ (2016) Laser and light therapies for the treatment of nail psoriasis. J Eur Acad Dermatol Venereol 30: 1278-1284. [crossref]
- Marc RA, Avram MM, Paul M (2014) Laser and light source treatments for the skin.
- Kent KM, Graber EM (2011) Laser tattoo removal: A Review. Dermatol Surg.
- Weinstein CJ (1994) Ultrapulse carbon dioxide laser removal of periocular wrinkles in association with laser blepharoplasty. Clin Laser Med Surg 12: 205-209.
- Ronald G (1997) Laser-assisted hair removal. Wheeland.
- Dai T, Tegos GP, Zhiyentayev T (2010) Photodynamic therapy for methieillin-resistant staphylococcus aureus infection in a Mouse skin abrasión model. Lasers Surg Med 42: 38-44.
- McCaughey RG, Chlebicki C, Wong BJ (2010) Novel wavelengths for laser nerve stimulation. Lasers Surg Med 42: 69-75. [crossref]
- Fan K, Bell P, Fried D (2006) Rapid and conservative ablation and modification of enamel, dentin, and alveolar bone using a high repetition rate transverse excited atmospheric pressure CO2 laser operating at 9.3 um. J Bio Opt 11: 064008-1 – 06008-11.
- Schelle FI, Polz S, Haloui H (2014) Ultrashort pulsed laser (USPL) application in dentistry: basic investigations of ablation rates and thresholds on oral hard tissue and restorative materials. J Lasers Med Sci 29: 1775-83.
- Lin JT (1992) Multiwavelength solid state laser for ophthalmic applications. Proc SPIE 1644: 266-275.
- Lin JT (1994) Mini-excimer laser corneal reshaping using a scanning device. Proc SPIE 2131: 228-236.
- Lin JT (1995) Critical review on refractive surgical lasers. Opt Engineer 34: 668-675.
- Lin JT (2016) Combined analysis of safety and optimal efficacy in UV-light-activated corneal collagen crosslinking. Ophthalmology Research 6: 1-14.
- Lin JT, Hong YL, Chang CL (2010) Selective cancer therapy via IR-laser-excited gold nanorods. Proc. SPIE 7562, 75620R.
- Murday JS, Siegel RW, Stein J, Wright JF (2009) Translational nanomedicine: status assessment and opportunities. Nanomedicine 5: 251-273. [crossref]
- Huang XH, El-Sayed IH, Qian W, El-Sayed MA (2009) Cancer cells assemble and align gold nanorods conjugated to antibodies to produce highly enhanced, sharp, and polarized surface Raman spectra: a potential cancer diagnostic marker. Nano Lett 7: 1591-1597.
- Chen PC, Mwakwari SC, Oyelere AK (2008) Gold nanoparticles: From nanomedicine to nanosensing. Nanotechnol Sci Appl 1: 45-65. [crossref]
- Tong L, Wei G, Cheng JX (2009) Gold nanorods as contrast agents for biological Imaging: optical properties, surface conjugation and photothermal effects. Photochem and Photobiol 85: 21-32.
- West JL, Halas NJ (2003) Engineered nanomaterials for biophotonics applications: improving sensing, imaging, and therapeutics. Annu Rev Biomed Eng 5: 285-292.
- Lin JT (2017) Analysis of the efficiency of photothermal and photodynamic cancer therapy via nanogolds and photosensitizers. J Cancer Research 4: 1-15.
- New Vision Inc. System catalogs; website: www.site.nvi-laser.com.