Abstract
Rowell syndrome is an uncommon clinical entity defined as the association of Erythema Multiforme (EM) like lesions in a patient with Systemic Lupus Erythematosus (SLE). We report the case of a 23-years-old married woman, mother of two healthy children, with no personal or family history of autoimmune disease, who was admitted to our emergency department for cutaneous lesions. The investigations showed positive autoantibodies indicative of SLE (such as anti-Smith and anti-Ro/SAA), which helped in establishing the diagnosis. The importance of Rowell syndrome as the first presentation of SLE is underscored and calling for vigilance and prolonged observation.
Keywords
rowell syndrome, systemic lupus erythematosus (SLE), erythema multiforme (EM), autoantibodies, early diagnosis, multidisciplinary approach
Introduction
Rowell syndrome is a distinct clinical entity, which was first described in the 1960s and consists of both erythema multiform-like cutaneous lesions and systemic lupus erythematosus. The syndrome is characterized by several autoantibodies, such as the speckled ANA pattern, as well as anti-RO/SSA and anti-La/SSB antibodies. The association of Rowell syndrome with autoimmune diseases, especially SLE, highlights the value of early diagnosis and appropriate management [1,2].
Case presentation
A 23-year-old woman, married and mother of two healthy children, was admitted to the emergency department with erythema multiforme like lesions on the face (Figure 1), decolletage, hands and feet. The patient complained of bilateral and symmetrical inflammatory arthralgias involving both small and large joints, without shoulder or pelvic girdle involvement.
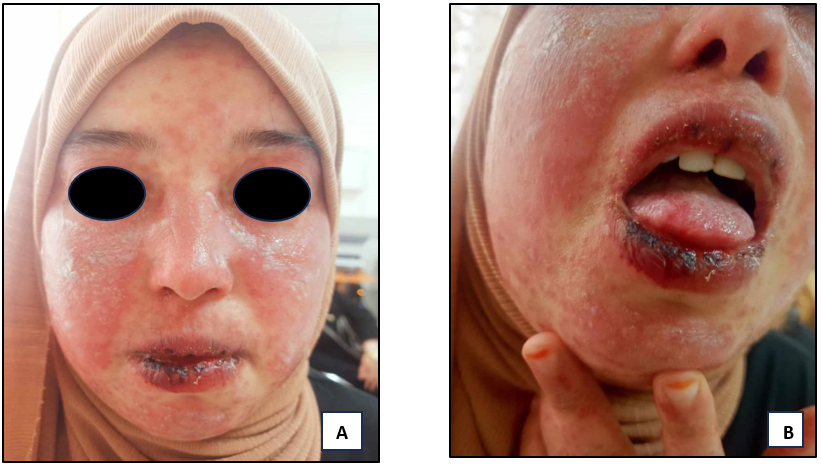
Figure 1. A and B show the cutaneous lesions of erythema polymorph-like in the course of Rowell’s syndrome upon the patient’s admission to the emergency department
An autoimmune workup was performed, which showed positive results for:
-Anti-ANA:1/1000
-Anti-Sm: Positive
-Anti-TRIM21: Positive
-Anti-Ro60: Positive
-Anti-SSB: Positive
-Anti-polymerase: Positive
-Anti-U1RNP: Positive
Although the patient did not show signs of Sjögren syndrome, a biopsy of the accessory salivary glands was considered to rule out underlying pathology. A thrombophilia analysis was also requested because of the clinical suspicion of systemic Lupus Erythematosus.
The obstetric history of the patient was unremarkable, without any previous miscarriages or thromboembolic events. In light of the clinical cutaneous and articular presentation in the patient, treatment with corticosteroids at a dose of 0,5 mg/kg/day was started concomitantly with hydroxychloroquine at 400 mg daily. The response was spectacular, with complete clearing of the cutaneous lesions and complete resolution of inflammatory arthralgias (Figure 2 after 15 days of treatment and Figure 3 after 1 month of treatment).

Figur0e 2. A, B and C show the spectacular response after only 15 days under corticosteroids and hydroxychloroquine

Figure 3. A and B show the complete clearing of the cutaneous lesions after 1 month under corticosteroids and hydroxychloroquine
Discussion
Rowell syndrome represents a distinct and rare condition closely linked to Systemic Lupus Erythematosus. The appearance of EM-like lesions with established markers of SLE should lead clinicians to consider the diagnosis of autoimmune disease in patients presenting with atypical manifestations of the skin. Previous publications on Rowell syndrome have documented its clinical features and association with a variety of immunological profiles [3-5].
One of the defining characteristics of Rowell syndrome consists of its histopathological resemblance to Lupus Erythematosus and Erythema multiforme. The histological pattern, marked by interface dermatitis and dense lymphocytic perivascular infiltrates, warrants careful investigation to distinguish it from the features of either SLE or erythema multiforme [6]. Other differential diagnoses to consider are drug-induced lupus, which superficially resembles both conditions, and Stevens-Johnson syndrome, particularly with mucosal involvement [7].
The clinical profile of our patient clearly highlights the difficulties inherent in managing autoimmune disease, particularly when multiple autoantibodies are involved. The presence of anti-Ro and anti-La antibodies is an important finding, as these are linked to subacute cutaneous lupus erythematosus and strongly suggest a risk of systemic progression [8,9]. When we manage an atypical lupus presentation, these serological markers become indispensable to assess a correct diagnosis. To ensure optimal long-term outcomes for patients with cutaneous autoimmune manifestations, a standard of care requiring a multidisciplinary approach between dermatology and internal medicine is essential. Crucially, the patient’s strong response to the rapid initiation of therapy underscores the profound clinical value of early intervention in managing related autoimmune conditions like SLE [10,11].
Conclusion
This case illustrates the importance of identifying that cutaneous findings may be the initial manifestation of Systemic Lupus Erythematosus. The clinical profile including Rowell syndrome features and serological results, requires intensive investigation for systemic autoimmune disease, facilitating early management and a better prognosis.
Conflicts of interest
The authors declare that there are no competing interests.
References
- Rowell NR, Beck JS, Anderson JR (1963) Lupus Erythematosus and erythema multiforme-like lesions. A syndrome with characteristic immunological abnormalities. Arch Dermatol 88: 176-180. [Crossref]
- Lee D, Waseh S, Motaparthi K, Hsu S (2023) Rowell syndrome in a middle-aged woman: A case report. Cureus 15: e39631. [Crossref]
- Bahat RY, Varma C, Bahatt S, Balachandran C (2014) Rowell syndrome. Indian Dermatol Online J 5: S33-S35. [Crossref]
- Gallo L, Megna M, Festa B, Stellato P, di Pinto R, et al. (2020) Rowell syndrome: A diagnostic challenge. J Clin Aesthet Dermatol 13: 40-42. [Crossref]
- Imtiaz R, Hornback C, Eslam M, Crowson AN, Levin J (2021) Targetoid lesions in a patient with systemic lupus erythematosus. Dermatol Online J 27: 13030. [Crossref]
- Zeitouni NC, Funaro D, Cloutier RA, Gagné E, Claveau J (2000) Redefining Rowell’s syndrome. Br J Dermatol 142: 343-346. [Crossref]
- Kim SS, Magro C, Granstein RD, Bass A, Erkan D (2013) Systemic lupus erythematosus associated with Rowell's syndrome: A clinical pathology conference held by the division of rheumatology at hospital for special surgery. HSS J 9: 289-292. [Crossref]
- Sethy M, Padhan P, Abirami C, Maikap D (2021) Rowell's syndrome: A case report and literature overview. Indian Dermatol Online J 12: 608-610. [Crossref]
- Singh S, Sheffield S, Chowdhury N, Nuthulaganti S, Vaghaiwalla Z, et al. (2021) Utilization of rituximab for refractory Rowell syndrome. Case Rep Rheumatol 2021: 2727382. [Crossref]
- Challa M, Baisya R, Devarasetti PK (2022) Rowell syndrome with good response to methotrexate. Mediterr J Rheumatol 33: 92-93. [Crossref]
- Zhang M, Lu J, Zhang B, Li Z, Wu W (2020) Rowell's syndrome with lupus hepatitis: A case report from China. Indian J Dermatol 65: 549-550. [Crossref]
