Abstract
Acute abdominal aortic occlusion is a rare phenomenon that requires rapid diagnosis and intervention. Patients are presented with severe pain and ischemia of the bilateral lower limbs with paresthesia or paraplegia. Acute occlusion can occur via de novo thrombus formation on an atherosclerotic aortic plaque and embolization of a central thrombus. Here we present a case with acute infrarenal abdominal aortic occlusion.
Key words
abdominal aorta, acute occlusion, thrombus, surgical treatment
Introduction
Acute abdominal aortic occlusion is a rare phenomenon that requires rapid diagnosis and intervention on account of high mortality rate. Patients are presented with severe pain and ischemia of the bilateral lower limbs with/without paresthesia or paraplegia. Acute occlusion can occur via de novo thrombus formation on an atherosclerotic aortic plaque and embolization of a central thrombus [1]. The Emory study determined that 55% of the patients have sensory or motor deficit [2]. These patients can easliy be misdiagnosed as a neurologic disorder, so meticulous physical examination for pulses is essential. Sudden paraplegia is related with the acute occlusion of the Adamkiewicz artery [3]. Acute occlusion with neurologic compromise significantly enhances the mortality rate. Acute aortic occlusion occurs in general heavy smoker young women with dyslipidemia. Risk factors are atrial fibrillation, cardiomyopathy, valvular heart disease, previous cardiac surgery and myocardial infarction. If there is sufficient collateralization due to atherosclerosis, acute aortic occlusion does not occur significant threat to the lower limbs. Here we present a case with acute infrarenal abdominal aortic occlusion.
Case report
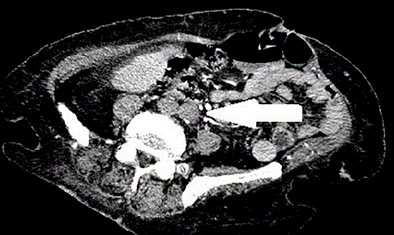
82-year-old woman presented to the emergency department with a 24 hours pain, numbness, paleness on the right lower limp, chronic atrial fibrillation and history of peripheral vascular disease with bilateral cladication intermittents. Her physical examination revealed that her femoral pulses were both nonpalpable, especialy her right lower limp was cold and pale. A clinical diagnosis of acute aortic occlusion with saddle embolism was suspected and then Doppler US performed, did not detect any pulse at the bilateral common femoral arteries, and the abdominal contrast enhanced computed tomography (CT) that was subsequently conducted revealed total occlusion of the abdominal aorta with only minor collateral flow on the left lower limb distally (Figure 1). We decided to perform emergency surgery. Under local anesthesia bilateral transfemoral aortoiliac and femoral embolectomies were performed using a balloon-tipped Fogarty catheter (Edwards Lifesciences, Irvine, California, USA), and a large amount of fresh thrombus material was retrieved from the aorta with satisfactory backbleeding from the legs during this procedure. Immediately after femoral circulation was restored. After the operation the patient was transferred to intensive care unit. No other complaint was reported. Four days after the surgery she was discharged home on warfarin and statin therapy.
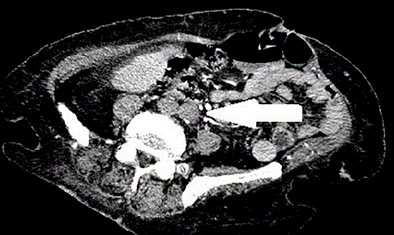
Figure 1. Computed tomography angiography (CTA) view of the thrombus inside the infrarenal abdominal aorta.
Discussion
Patients presented with instantaneous severe lower limb pain, coolness, paleness, absence of pulses with or without sensory or motor deficits are diagnosed as acute thrombotic occlusion of the infrarenal abdominal aorta. Patients diagnosed with history of peripheral artery disease (approximately 75% of the cases) might present with relatively mild clinics due to the presence of collaterals. Heart disease, female gender, smoking, diabetes are risk factors [4]. Conditions such as dehydration, diabetic ketoacidosis, and heart failure slow down the circulation on the stenotic level that can precipitate occlusion [5]. In the presence of accompanying chronic atrial fibrillation with large left atrium, large burden of thrombus originate from the heart can occlude the aorta. Other causes of large emboli are fungal/bacterial vegetations, prosthetic valve thrombus, primer malignencies of the heart especially atrial myxomas. Despite occlusion can be seen any part of the aorta, infrarenal abdominal aorta, especially the iliac bifurcation portion are the most frequent site. Mortality (%21) and morbidity rates are higher, on account of that limb loss is seen in 90% of Patients [6]. Some authors indicates that the morbidity rate exceeds 75% [5]. From the beginning of the symptoms, elapsed time to revascularization can significantly affects the mortality rate. Dossa et al. stated that neurologica deficit is more important rather than ischemia time. Albeit,
acute aortic occlusion can be diagnosed clinically, aortography is the gold standard test. However, Doppler US, contrast-enhanced CT and magnetic resonance angiography (MRA) can also used for the diagnosis [7]. Delay in diagnosis and prompt intervention have a significant affect on morbidity and mortality. Decisions should be made based on the patient’s clinic and comorbidities. In order to maintain sufficient circulation early surgical intervention is recommended including bilateral femoral embolectomy, medical therapy with thromboliytics and anticoagulation. Unfortunately medical therapy have poor results [1]. Some authors reported that aortic reconstruction should be performed due to the potential risk of propagation of thrombosis at the distal aorta up to the renal and mesenteric arteries [8]. However, McCullough et al. determined that there was no significant reduction in life expectancy in who did not undergo surgery [9]. Thrombus that are on a level with renal arteries, aortic reconstruction or femoral revascularization via aortofemoral bypass should be made promptly. We performed surgery under local anesthesia by using balloon-tipped fogarty catheters via a transverse arteriotomies made on both common femoral arteries without any delay. Taking into account current comorbidities, surgery was the best treatment option for the patient and she benefited from treatment. In conclusion, patients admitted to the hospital because of sudden lower limb ischemia should be diagnosed and treated promptly due to the burden of thrombus in the aorta.
Declaration of conflicting interests
The authors declared no conflicts of interest with respect to the authorship and/or authorship of this article.
Funding
The authors received no financial support for the research and/or authorship of this article.
References
- Surowiec SM1, Isiklar H, Sreeram S, Weiss VJ, Lumsden AB (1998) Acute occlusion of the abdominal aorta. Am J Surg 176: 193-197. [Crossref]
- Shaw A1, Anwar H, Targett J, Lafferty K (2008) Cauda equina syndrome versus saddle embolism. Ann R Coll Surg Engl 90: W6-8. [Crossref]
- Olearchyk AS1 (2004) Saddle embolism of the aorta with sudden paraplegia. Can J Surg 47: 472-473. [Crossref]
- Dossa CD1, Shepard AD, Reddy DJ, Jones CM, Elliott JP, et al. (1994) Acute aortic occlusion. A 40-year experience. Arch Surg 129: 603-607. [Crossref]
- Babu SC1, Shah PM, Nitahara J (1995) Acute aortic occlusion--factors that influence outcome. J Vasc Surg 21: 567-572. [Crossref]
- Ting JY1, Dehdary A (2011) Acute severe non-traumatic muscle injury following reperfusion surgery for acute aortic occlusion: case report. Int J Emerg Med 4: 20. [Crossref]
- Singh A, Naqvi T, M2021 Copyright OAT. All rights reservhrombotic complete occlusion of the aorta: accurate, immediate clinical decision-making by echocardiography. Am J Med 122:e1. [Crossref]
- Lee SB, Hall CW, Wijdicks EF (2005) Monoplegia due to acute aortic occlusion. Muscle Nerve 32: 686-687. [Crossref]
- McCullough JL Jr, Mackey WC, O'Donnell TF Jr, Millan VG, Deterling RA Jr, et al. (1983) Infrarenal aortic occlusion: a reassessment of surgical indications. Am J Surg 146: 178-182. [Crossref]