Abstract
Background
A framework for adolescent and young adult (AYA) survivors that addresses developmental milestones, short and long-term impacts of cancer on relationships is needed to understand the long-term consequences of cancer treatment and why AYAs do not participate in long-term follow-up care.
Objectives
Develop a theoretical framework of end-of-treatment and early post-treatment based on a systematic review of the literature and suggest future directions for research that derive from the review.
Method
A systematic review of published research from 1994 to 2014 was conducted using three databases: PubMed, CINAHL, Psych Info using search terms survivors AND end of treatment OR transition* AND cancer.
Results
The framework is organized along a time trajectory that includes treatment and post-treatment separated by the critical transition of end-of-treatment. The framework explores links between AYA development; changes in survivor’s relationships with parents, peers, siblings, health care providers; and evidence of issues at end-of-treatment for survivors and parents.
Conclusion
Results from the systematic review suggest that end-of-treatment and early post-treatment are particularly challenging for survivors and parents. Five areas of future research are identified: provider behaviors that contribute to AYA’s feelings of abandonment; end-of-treatment and follow-up visits; survivor and parent expectations at end-of-treatment and actual challenges in post-treatment; convergence or discordance between the AYA’s and parent’s concerns and how parents’ concerns may conflict and thwart survivors’ efforts to achieve developmental milestones; and peers’ perceptions and concerns.
Introduction
The landscape is changing for adolescent and young adult (AYA) cancer survivorship. Approximately 80% of the more than 14,000 AYA (10 to 25 years) diagnosed with cancer each year will become long-term survivors [1]. Cancer survivorship begins with diagnosis, proceeds through treatment and post-treatment, and continues until life ends. Post-treatment survivorship for AYA survivors often involves facing late effects, which can occur years after treatment ends. Late effects include recurrent and secondary cancers, cardiovascular disease, cardiomyopathy, pulmonary fibrosis, cognitive dysfunction, musculoskeletal problems, and endocrinopathies [2-4]. Despite significant lifetime risks for late effects, less than 50% of AYA survivors participate in long-term follow-up care [3,5]. Current frameworks for AYA survivorship emphasize disease and symptoms. Although important for understanding the long-term consequences of cancer treatment, they fail to address developmental milestones; the short and long-term impact of cancer on their relationships with parents, siblings, and peers; and they fail to explain why AYAs do not participate in long-term follow-up care.
The two purposes to this paper are to: 1) develop a theoretical framework of the end-of-treatment transition and early post-treatment for adolescent and young adult (AYA) cancer survivors that derives from a systematic review of the literature and 2) suggest needed future directions for research that derive from the theoretical framework. Although the review and theoretical framework focus on the survivor, parental issues are included because of their central importance in supporting survivors during and after treatment. The paper is organized into threesections. The first section contains a systematic review of the literature; the second section presents the proposed theoretical framework of end-of-treatment and early post-treatment that derives from that review. The final section identifies needed future directions for research with AYA cancer survivors and their families.
Systematic review of literature: end-of-treatment and early post-treatment
A systematic literature review was conducted using three databases: PubMed, CINAHL, and Psych Info. These search terms were used to access articles within the past 20 years: survivors AND end of treatment OR transition* AND cancer. The searches were limited to school age (6-12 years), adolescents (13 to 18 years) and young adult (19 to 24 years). Papers were included if they were data based, focused on parents and/or AYA survivors (12 to 24 years old) at end of treatment or early post-treatment (i.e.,< 5 years). Papers were excluded if they focused primarily on adults (i.e., > 24 years) or long-term survivorship (i.e.,> 5 years). A total of 461 abstracts were retrieved and reviewed for relevance. Of these abstracts, 449 were omitted because they were duplicates, non-English, not data based, focused primarily on adults or adult cancer diagnoses, or participants had completed treatment five or more years prior to data collection. The remaining 12 articles were retrieved and read in full. Four additional articles were identified from reference lists, resulting in a total of 15 articles [6-20]. Findings from these 15 articles were further organized into two broad areas for the current analysis: feeling abandoned by healthcare providers; feeling unsupported, unsafe, and unprepared for end-of-treatment and post-treatment; and parental distress.
The end-of-treatment transition and early post-treatment period were described as confusing periods of physical, psychological, and social adjustment [10]. Survivors reported a range of emotions at end-of-treatment [6]. They felt grateful to be alive [6], relieved treatment was over; but “weird” and worried about going back to school [7]. They felt angry about opportunities missed because of treatment such as prom and studying abroad; and opportunities that may have been delayed such as college, graduate school, marriage, and children [6,9]. Although parents expressed a sense of relief about finishing treatment, they reported primarily negative emotions [7,14,16]. Parents felt scared, anxious, helpless, uncertain, and lonely; terrified of relapse, and under constant stress [7,14,16].
Feeling abandoned by healthcare providers; unsupported, unsafe, and unprepared forend-of-treatment and survivorship
AYA survivors and their parents’ descriptions of the end-of-treatment transition and early post-treatment period were characterized by feeling abandoned, unsupported, unsafe, and unprepared [6,7,10,16,18].
Feeling abandoned
AYA survivors felt abandoned by healthcare providers [6,7,10,16,18]., “thrown out there,”[7]and grossly unprepared for end-of-treatment [6]. Feelings of abandonment by healthcare providers were related to three issues: abrupt changes in care delivery and monitoring, losing caringrelationships, and lack of preparation for end-of-treatment and post-treatment [10,15]. Few survivors reported having a formal opportunity with their health care provider to discuss the end-of-treatment transition, or ask questions about their treatment and future care [10,15].
Parents also felt an intense loss of the close relationships they developed with healthcare providers [6,7,16,18]. They reported losing important sources of practical, informational, and emotional support from healthcare providers [16]. They also felt an increased burden of responsibility for their child’s care at a time when financial and social supports were declining [16].
Unsupported and unsafe
Survivors reported a sudden shift in healthcare providersexpectations of them from dependence to independence. Post-treatment they did not know who to contact for help, what follow-up care to pursue, or how to respond to symptoms associated with treatment. They felt alone and unsupported in making the transition from a patient role during treatment to a self-management role in survivorship [10].
Survivors reported interactions with healthcare providers at follow-up visits illustrated their feelings of being unsupported and unsafe. Survivors reported they no longer felt they were a priority for healthcare providers since they were no longer acutely ill or receiving treatment [6]. While survivors were seeking help with symptoms, recovery from treatment, and late effects, providers focused solely on surveillance for recurrence [15,10]. Many survivors experienced late effects that affected their physical, psychological, and social health [15]. Although providers were sympathetic, they documented the survivors’ problems but did not provide the action plans that survivorsexpected [15,10]. Survivors were disappointed by healthcare providers’ responses to their issues and found their lack of understanding particularly difficult to accept [15], after the comprehensive care they received during treatment.
Unprepared for survivorship
Feeling unprepared for end-of-treatment and early post-treatment was also shocking for survivors and parents after the thorough preparation healthcare providers provided at diagnosis and during treatment [10]. Because of the lack of preparation, survivors were not able to anticipate the challenges they would face when resuming everyday life and did not have strategies to deal with them [15]. Because of the lack of preparation for end-of-treatment, AYA survivors expected a smooth transition to their normal lives, which were not met in reality [15]. Many survivors experienced physical and psychological long-term side effects and late effects from their treatment, describing themselves as being in a state of “in-between,” “on standby,” “in an unknown world,” “neither sick nor healthy”[15]; somewhere “between being cured and being healed”[6]. They did not know how to manage their symptoms or integrate the positive and negative aspects of the cancer experience into their evolving identity [8,6,15,19].
Survivors were not prepared for their feelings of being “out of place” in school, work, and cancer settings [9]. They had missed out on everyday social experiences with peers, and faced a life-threatening illness that their peers had difficulty comprehending [6]. They reported their peers were often uncomfortable and reluctant to hear about the cancer experience, and expected the survivor to return to normal and put the cancer behindthem [6,8,9]. AYA survivors did not have strategies for explaining their cancer experience to peers [15].
AYA survivors were surprised to find that they felt out of place in cancer settings when they returned for follow-up visits. They found themselves in primarily pediatric settings with young children or in adult settings with older adults, coined by one AYA survivor as a paradox of “diapers to dentures”[9]. They did not find support from older or younger cancer survivors because their challenges were very different from their own [15]. AYA survivors wanted to meet other AYA survivors who shared their experience and understood their challenges. They also wanted assistance developing skills to communicate their cancer experience and to connect with peers without cancer [13,15].
Parents too felt unprepared. They did not know how to respond to their child’s health and psychosocial concerns, how to support their return to school or work, deal with self-consciousness about their appearance and abilities, or their feelings of isolation and uncertainty about the future [16]. In addition, parents lacked knowledge about medical follow-up and differences between treatment complications and late effects [7,16].
AYA survivors wanted healthcare providers to prepare them for end-of-treatment and post-treatment. They wanted information that was timely, repeated at regular intervals, and explained in terms of benefit to them. Most importantly, they wanted information about issues pertinent to their developmental stage: body image, lifestyle choices [13]; returning to school or work [7,16]; connecting with other AYA survivors [9,10,15]; andcommunicating their experience with peers without cancer [13]. In addition, they wanted information and resources about medical follow-up, treatment complications versus late effects specific to their particular cancer, and financial support for AYA survivors [7,9,13,16].
Parental Distress
Psychological distress can be especially high in the first two yearspost-treatment. In one prospective study of 129 parents, at two months post-treatment, 72% of mothers and 60% of fathers reported clinically elevated levels of psychological distress [11]. This distress decreased slowly over time and reached normal levels at two years post-treatment [11].
The small but compelling literature on AYA survivorship suggests that both clinicians and scientists are failing to recognize the intense struggle AYA survivors and their parents experience at the end-of-treatment and early post-treatment. The evidence is that AYAs and parents have no idea what to expect after treatment--they have no roadmap for what lies ahead for them. Their only anchor is life before cancer, a hope that life will “return to normal,” and a deep knowing that life is forever changed.
Theoretical Framework of End-of-Treatment and Early Post-Treatment for AYASurvivors
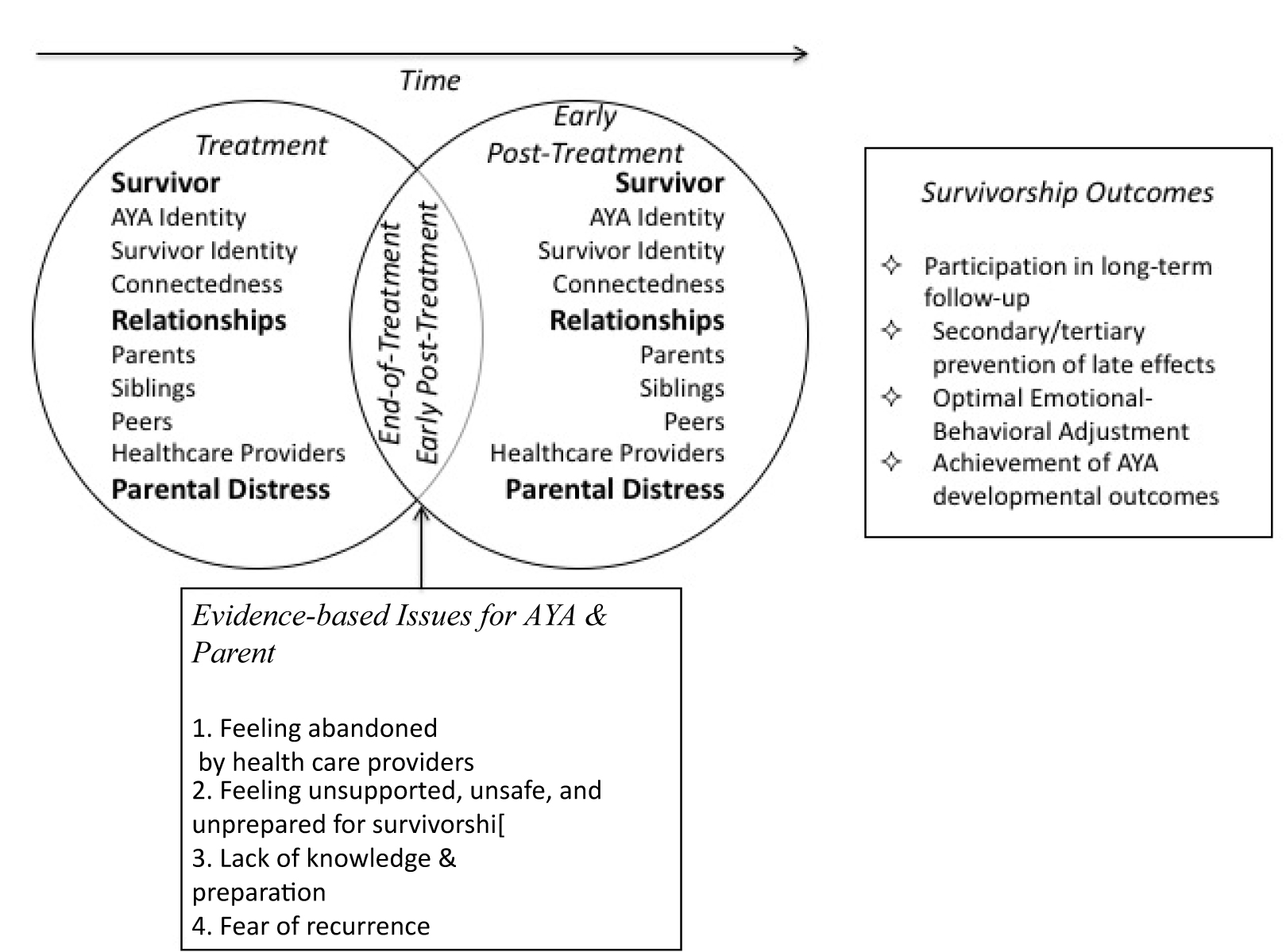
The theoretical framework that derives from the systematic review integrates and extends three theories that we propose fit the results from the systematic review: Psychosocial Development Theory [21,22], Adolescent Connectedness Theory [23], and Transition Theory [24]. The concepts of identity formation [21,22]; connectedness [23], and transition [24] are central to the theoretical framework. See Figure 1; the text below moves from left to right in the figure.
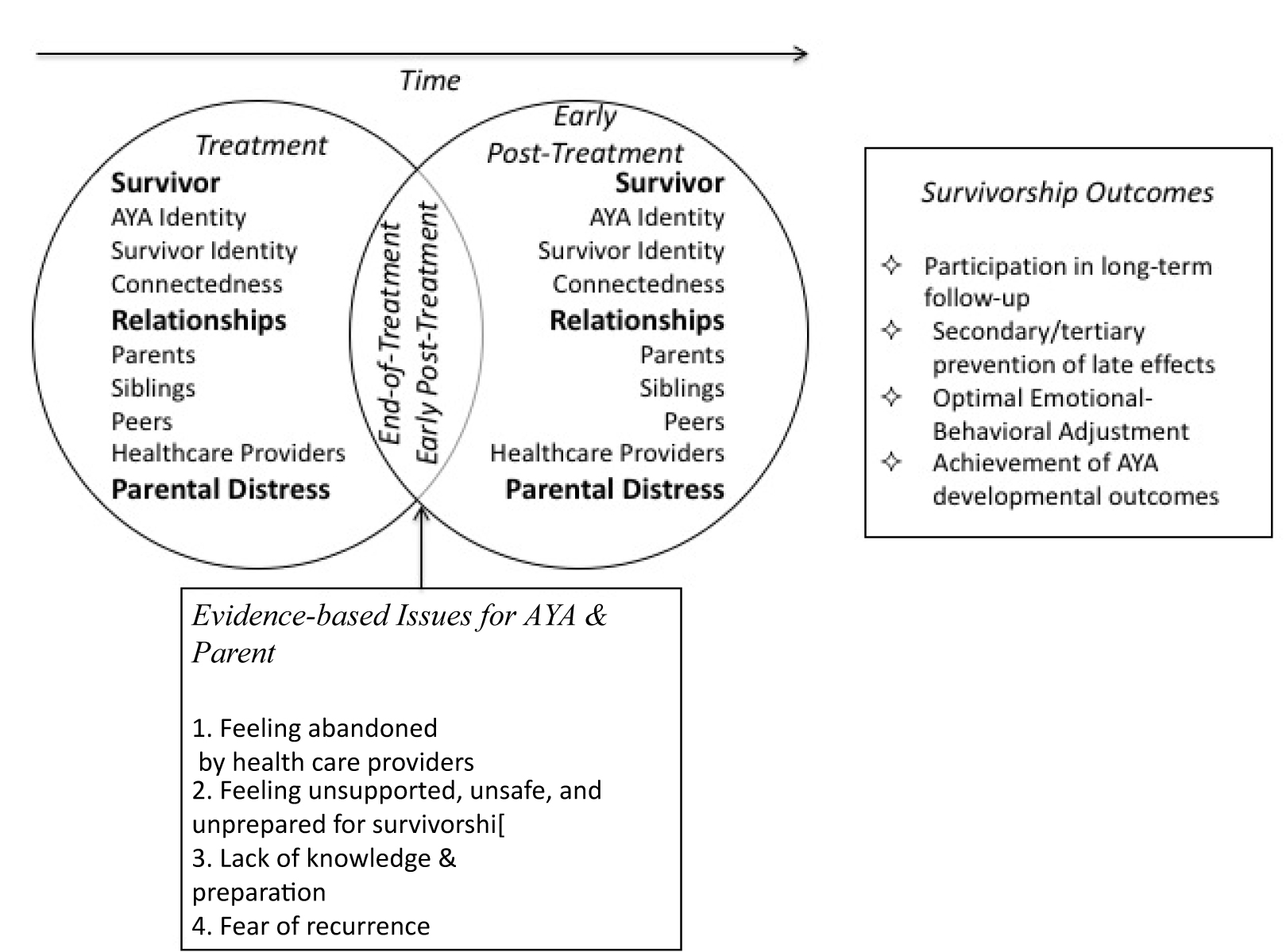
Figure 1. Theoretical framework for end-of-treatment and early post-treatment
The theoretical framework consists of two distinct chronological phases: treatment and post-treatment. End-of-treatment is a critical transition that heralds the significant shifts that occur post-treatment in AYA survivors’ relationships with parents, siblings, peers, and healthcare providers. In this theoretical framework, a transition is a passage from one life phase to another, which includes process, time, and perception [25]. The end-of-treatment transition is more than a passage from treatment to post-treatment. Rather it is a period of suspension between what is and what has not yet become [26]. Parental distress at end-of-treatment is important to understand in the framework since parents are deeply involved with the survivor during and after treatment. Their distress can impact their ability to assist their AYA in survivorship. The primary assumption of the framework is that experiences and events that occur during treatment, end-of-treatment, and early post-treatment, including changes in relationships with parents, siblings, and peers have a sustained impact on AYA survivors and their families. This sustained impact can affect emotional-behavioral adjustment and developmental and health outcomes, including participation in long-term follow-up care.
AYA Relationships
AYA survivors are defined as persons diagnosed or treated for cancer during adolescence or young adulthood (10 to 25 years). This period can be divided into four stages: early adolescence, junior high or middle school (10 to 13 years); middle adolescence, high school (14 to 17 years); late adolescence, college or work (18 to 21 years); and young adulthood, early career and family (22 to 25 years) [27]. The developmental goals of AYA are to develop a self-identity separate from parents and peers, and to increasingly navigate physical,economical, and psychosocial situations on their own [28]. The achievement of developmental milestones occurs gradually over approximately 15 years. The dominant issues for AYA are the development of their identity, autonomy, intimacy, sexuality, and academic achievement [27].
Relationships with parents, siblings, and peers provide the primary social context for adolescence and young adulthood, each playing a crucial, contrasting role in promoting healthy psychosocial development [27]. As the systematic review revealed, the challenges and concerns AYA survivors face at end-of-treatment occur within the context of their relationships with parents, siblings, peers, and healthcare providers. In these relationships, adolescents seek a sense of connectedness, defined as feelings of relatedness and belonging with self and others [23]. Connectedness is mutable: behaviors and attitudes that promote connectedness can be increased or decreased, shaped and developed to improve outcomes [29].
Parents
The quality of the parent-adolescent relationship is the single most consistentpredictor of adolescents’ mental health and well-being [30,31]. As a child moves through adolescence, the parental role shifts from providing primarily nurturance, protection, and socialization to providing support, guidance, and direction. The adolescent gradually begins to navigate physical, economic, and psychosocial situations on his or her own [28]. During and after treatment, parental relationships are the only relationships that remain stable for survivors. Future research needs to explore whether parental concerns and challenges conflict or thwart AYA efforts to achieve developmental milestones.
Siblings
Like parents, siblings share kinship and long histories of interactions with theAYA. Conflict is common among siblings because they do not fear the dissolution of the relationships like they do with peers [30], and siblings lack the authority of parents. Because they are often close in age, siblings assist AYA’s in the process of individuation [30]. Future research needs to explore the needs and concerns of non-ill siblings including their adjustment and the quality of their relationships with their ill sibling and parents.
Peers
Peers provide critical functions in the development of identity, autonomy,intimacy [27]; and a sense of connectedness [29]. Peers provide social feedback as AYA experiment with roles and personalities and a platform for testing decision-making skills without the presence of adults. Further, intimate relationships are cultivated between peers who are relative equals [27].
Healthcare providers
Relationships with healthcare providers become an importantsocial context for AYA during the treatment phase of cancer. AYA and families depend on healthcare providers for medical and psychosocial support during treatment [6,16].
Treatment and Post-treatment
Treatment
Prior to diagnosis, AYA are seeking greater independence and autonomy[27]. They spend approximately 30% of their waking time at school or work, and another, 20 to 30% interacting with their peers [32,33]; only 15% of their time with adults, which include their parents [27]. Treatment starts within hours or days of diagnosis and the 60% of time previously spent with peers at school and work [32, 33] isreplaced by time with adults—parents at home, and parents and health care providers at the hospital and outpatient clinic.
AYA are treated with standardized, risk-based protocols depending on the clinical and laboratory features of their disease [34] that can include chemotherapy, surgery, and radiation. Although diagnosis and treatment pose significant threats to AYA and parents, survivors and families receive significantly more support and guidance during these periods than any other period along the treatment trajectory. Survivors and parents are provided with detailed roadmaps for treatment and support services, and are closely monitored by healthcare providers. Although uncertainty remains, they are prepared for each procedure and treatment, including side effects and psychosocial challenges, and are supported by health care providers including nurses, physicians, and social workers.
Treatment for AYA cancer is long and arduous, and literally changes the biographies of survivors [17]. AYA report that during treatment their lives are disrupted at a critical time when significant opportunities for autonomy and independence must be relinquished or postponed. During treatment they struggle with “feeling left behind” and fear the long-term impact of cancer on their life trajectory [17]. Adolescents also report struggling with existential issues [35]. They worry about their loss of autonomy and independence, the burden of cancer on their parents and siblings, not being able to spend time with friends and disconnection from their lives at school, the possibility of not reaching developmental milestones, and not surviving cancer [35]. They feel isolated, trapped, stuck, and imprisoned by cancer, especially in the hospital [35]. They spend much of their time “waiting” and feel their lives are “on hold” [35]. They long to escape the cancer world and return to a normal life [35].The developmental impact of treatment varies by the age of the adolescent. Early adolescents likely will be more dependent on their parents than late adolescents or young adults, some of whom are living on their own when diagnosed. Healthcare providers become an important social context for AYA’s due to the amount of time spent in the clinic and hospital and the support they provide. To some degree time with health care providers replaces time with peers during treatment [6,16]. AYA become more dependent on their parents for physical and emotional support and are increasingly isolated from their peers. Parents are forced to navigate entire new domains of parenting behavior to support their AYA and themselves with the demands and uncertainty of cancer treatment. Relationships with siblings also change as a result of frequent hospitalizations, clinic visits and changes in family dynamics [20].
End-of-treatment transition
End-of-treatment is defined by two important criteria inthis framework: the last treatment, when something is actively done to fight the cancer; and disengagement from healthcare providers, when follow-up visits are extended to every three to six months. The systematic review revealed three issues for AYA survivors and their parents: 1) feeling abandoned by healthcare providers, 2) feeling unsupported, unsafe, and unprepared for survivorship, and 3) fear of recurrence.
Post-treatment
Aside from the small l2021 Copyright OAT. All rights reservearly post-treatment, research has focused on the long-term health and psychosocial outcomes of childhood cancer survivors rather than their experience, and developmental and psychosocial challenges. Future research needs to include intensely focused studies with AYA survivors and parents who choose not to participate in long-term medical surveillance and follow-up. Such studies are essential to identify barriers to participation; to fully elaborate both AYA and parentalframeworks of understanding about survivorship and what it takes to survive; and to identify particular challenges parents and AYA experienced that, despite best efforts, leave them “stuck.”
Future needed directions for research and intervention
Given what we know about challenges for AYA survivors and parents at end-of-treatment from the systematic review, five areas of needed research are identified. First, studies are needed to describe the events and behaviors of healthcare providers that contribute to AYA survivor’s feelings of abandonment. These data can be used to develop education programs for providers not only to prevent these behaviors, but to develop models for follow-up treatment that address these issues. Second, studies are needed to describe the end-of-treatment visit-if and when it occurs, what is and is not discussed, questions asked, and what preparation if any they receive about end-of-treatment and early post-treatment. These data can be used to develop and test an effective guide for the content of this visit. Third, descriptive studies are needed to more fully elaborate AYA and parent’s expectations for end-of-treatment and early post-treatment; the actual challenges they experience in their transitions to home and school life; and how these early experiences influence survivors’ compliance with long-term follow-up care. Fourth, descriptive studies are needed to understand if and where the issues and concerns of AYA and parents are discordant with each other. More specifically, studies are needed to explore whether the concerns held by parents conflict and thwart AYA efforts to achieve developmental milestones. Fifth, descriptive studies are needed to elucidate peers’ understandings of cancer treatment and post-treatment so that interventions can be developed to educate peers and assist survivors in communicating with peers. Pending results from the descriptive studies, programs and services need to be developed to address the end-of-treatment and early post-treatmenttransition. Without this research, evidence-based programs and services for AYA and parents will not exist.
References
- Ries LAG, Melbert D, Krapcho M, Mariotto A, Miller BA, et al. (2007) SEER Cancer Statistics Review, 1975-2004, National Cancer Institute, Bethesda, Md.
- Hudson MM, Ness KK, Gurney JG, Mulrooney DA, Chemaitilly W, et al. (2013) Clinical ascertainment of health outcomes among adults treated for childhood cancer. JAMA 309: 2371-2381. [Crossref]
- Nathan PC, Greenberg ML, Ness KK, Hudson MM, Mertens AC, et al. (2008) Medical care in long-term survivors of childhood cancer: a report from the childhood cancer survivor study. J Clin Oncol 26: 4401-4409. [Crossref]
- Oeffinger KC, Mertens AC, Sklar CA, Kawashima T, Hudson MM, et al. (2006) Chronic health conditions in adult survivors of childhood cancer. The New England Journal of Medicine 355: 1572-1582.
- Buchbinder D, Mertens AC, Zeltzer LK, Leisenring W, Goodman P, et al. (2012) Cancer prevention and screening practices of siblings of childhood cancer survivors: a report from the childhood cancer survivor study. Cancer Epidemiol Biomarkers Prev 21: 1078-88.
- Cantrell MA, Conte TM (2009) Between being cured and being healed: the paradox of childhood cancer survivorship. Qual Health Res 19: 312-322. [Crossref]
- Duffey-Lind EC, O'Holleran E, Healey M, Vettese M, Diller L, et al. (2006) Transitioning to survivorship: a pilot study. J Pediatr Oncol Nurs 23: 335-343. [Crossref]
- Jones BL, Parker-Raley J, Barczyk A (2011) Adolescent cancer survivors: identity paradox and the need to belong. Qualitative Health Research 21: 1033-1040.
- Kent EE, Parry C, Montoya MJ, Sender LS, Morris RA, et al. (2012) "You're too young for this": adolescent and young adults' perspectives on cancer survivorship. J Psychosoc Oncol 30: 260-279. [Crossref]
- Parry C, Morningstar E, Kendall J, Coleman EA (2011) Working without a net: leukemia and lymphoma survivors' perspectives on care delivery at end-of-treatment and beyond. J Psychosoc Oncol 29: 175-198. [Crossref]
- Maurice-Stam H, Oort FJ, Last BF, Grootenhuis MA (2008) Emotional functioning of parents of children with cancer: the first five years of continuous remission after the end of treatment. Psychooncology 17: 448-459. [Crossref]
- Thompson AL, Gerhardt CA, Miller KS, Vannatta K, Noll RB (2009) Survivors of childhood cancer and comparison peers: the influence of peer factors on later externalizing behavior in emerging adulthood. J Pediatr Psychol 34: 1119-1128. [Crossref]
- Stinson JN, Sung L, Gupta A, White ME, Jibb LA, et al. (2012) Disease self-management needs of adolescents with cancer: perspectives of adolescents with cancer and their parents and healthcare providers. J Cancer Surviv 6: 278-286. [Crossref]
- Stam H, Grootenhuis MA, Brons PPT, Caron HN, Last BF (2006) Health-related quality of life in children and emotional reactions of parents following completion of cancer treatment. Pediatric Blood & Cancer 47: 312-319.
- Hauken MA, Larsen TM, Holsen I (2013) Meeting reality: young adult cancer survivors' experiences of reentering everyday life after cancer treatment. Cancer Nurs 36: E17-26.
- Rivero-Vergne A, Berrios R, Romero I (2011) The return to the community after cancer treatment: from safety to reality check. J Psychosoc Oncol 29: 67-82. [Crossref]
- Grinyer A (2007) The biographical impact of teenage and adolescent cancer. Chronic Illn 3: 265-277. [Crossref]
- Haase JE, Rostad M (1994) Experiences of completing cancer therapy: children's perspectives. Oncol Nurs Forum 21: 1483-1492. [Crossref]
- Stegenga K, Macpherson CF (2014) "I'm a survivor, go study that word and you'll see my name": adolescent and cancer identity work over the first year after diagnosis. Cancer Nurs 37: 418-428. [Crossref]
- Mcgrath P (2008) 'Feeling very left out': parents' insights on siblings of children treated for childhood acute lymphoblastic leukaemia. Austral-Asian Journal of Cancer 7: 137-143.
- Erikson EH (1950) Childhood and society, New York, W. W. Norton.
- Gruber HE, Voneche JJ (1995) The essential piaget, Northvale, N.J.
- Karcher MJ, Holcomb MR, Zambrano E (2008) Measuring adolescent connectedness: A guide for school-based assessment and program evaluation. In: Coleman, H. L. K. (Ed.) Handbook of School Counseling. New York: Routledge.
- Meleis AI, Sawyer LM, Im EO, Hilfinger Messias DK, Schumacher K (2000) Experiencing transitions: an emerging middle-range theory. ANS Adv Nurs Sci 23: 12-28. [Crossref]
- Chick N, Meleis AI (1986) ‘Transitions: a nursing concern.’ In: P Chinn (ed.), Nursing research methodology, Boulder, Co: Aspen Publication.
- Lewis FM (1993) Psychosocial transitions and the family's work in adjusting to cancer. Semin Oncol Nurs 9: 127-129. [Crossref]
- Steinberg L (2014) Adolescence, New York, Mcgraw-Hill.
- Steinberg L, Silk JS (2012) Parenting adolescents. In: Bornstein, M. H. (Ed.) Handbook of Parenting Volume 1: Children And Parenting. Second Ed. New York: Psychology Press.
- Karcher MJ (2011) The hemingway: measure of adolescent connectedness. San Antoniio: University of Texas.
- Campione-Barr N, Greer, KB, Kruse A (2013) Differential associations between domains of sibling conflict and adolescent emotional adjustment. Child Development 84: 938-54.
- Resnick MD, Bearman PS, Blum RW, Bauman KE, Harris KM, et al. (1997) Protecting adolescents from harm. Findings from the National Longitudinal Study on Adolescent Health. JAMA 278: 823-832. [Crossref]
- Csikszentmihalyi M, Larson RW (1984) Being adolescent: conflict and growth in the teenage years, New York, Basic Books.
- Larson RW, Verma S (1999) How children and adolescents spend time across the world: work, play, and developmental opportunities. Psychol Bull 125: 701-736. [Crossref]
- Children's Oncology Group (2011) Family handbook for children with cancer. Second Ed. Bethesda, Md.
- Woodgate RL, West CH, Tailor K (2014) Existential anxiety and growth: an exploration of computerized drawings and perspectives of children and adolescents with cancer. Cancer Nurs 37: 146-159. [Crossref]