Atrial fibrillation (AF) is one of the most important risk factors for stroke, heart failure, and other cardiac disturbances, but little is known about the association with metabolic diseases such as diabetes mellitus (DM). Although several reports have studied their association, the results have been controversial and no large scale study has been reported in the real world clinical practice. We investigated the frequency of AF in 13,868 patients (DM: 6,202, AF: 309) who consulted our hospital in the last two years. We conducted a cross-sectional case-control study and examined the association between AF and metabolic diseases (DM, dyslipidemia) and cardiovascular and renal diseases (hypertension, heart failure, chronic renal failure). AF was observed in 3.26% of the DM group and 1.37% in the control group. The occurrence frequency between AF and DM was 2.40 as shown by the odds ratio of the risk of DM for AF (95% confidence interval; 1.89-3.06, p< 0.01%). We demonstrated for the first time in a large scale investigation in the real world clinical practice that DM would significantly increase the risk of the onset of AF. It is recommended that patients with DM should take electrocardiography regularly and be intervened at an early stage.
atrial fibrillation, diabetes mellitus, risk factor, large scale, association
Atrial fibrillation (AF) is the most common arrhythmia in clinical practice, and is associated with an increased risk of cerebral infarction, heart failure, and overall mortality. Recently, AF has been attracting attention due to its increased treatment options by release of the novel oral anti-coagulants. Nevertheless, the important concept of the management of AF remains to be its prevention. Therefore, identification of risk factors is important, especially in the real world clinical practice.
In Japan, the number of patients with AF and the prevalence are on the increase, and are estimated to exceed one million by 2050 [1]. Diabetes is also on the increase just as AF, and is likely to exceed 30 million by 2018. It is important to prevent the onset of cerebral infarction in the management of patients with AF. As for the CHADS2 score which is known as a risk factor of cerebral infarction [2], it is evident that diabetes is the second most important factor following age [3]. The influence of diabetes becomes larger especially when the disease duration prolongs to 8 to 10 years. The risk factors of the onset of AF have long been studied so far. And one of the old but good examples is Framingham study, in which diabetes is considered as one of the significant risk factors (odds ratio (OR): 1.4 for men and 1.6 for women) [4].
Recent meta-analysis has reported that diabetes can be a risk factor of AF [5]. However, some studies report conflicting findings [6,7], partly because most of these studies are case-control studies that are likely to be biased. Although there have been reports of large-scale study, most of them are based on community-based medical checkup [8]. To our knowledge, there has been no report of the large-scale study from the real world clinical practice. Therefore, this conclusion is not fully agreed. We worked on the issue, because we are from one of the hospitals that hold the largest number of diabetic patients in Japan.
Ethics
The study design was based on the Japanese government's Ethical Guidelines Regarding Epidemiological Studies in accordance with the Declaration of Helsinki. The protocol of the present study was approved by the institutional review board.
Study subjects
Subjects were selected from those who came to our hospital during the study period from May 2011 to April 2013. Diagnoses were made by attending physicians and were input into disease name database. Medical history was investigated based on the disease name database.
Statistical analysis
We conducted a cross-sectional case-control study for the analysis. Statistical analysis was conducted to calculate odds ratio. Here, we simply used Chi-square test for independence by two-by-two contingency table. The presence or absence of the history of treatment was not investigated.
Patient characteristics
Total 13,868 subjects were enrolled in this cross-sectional study during the study period.
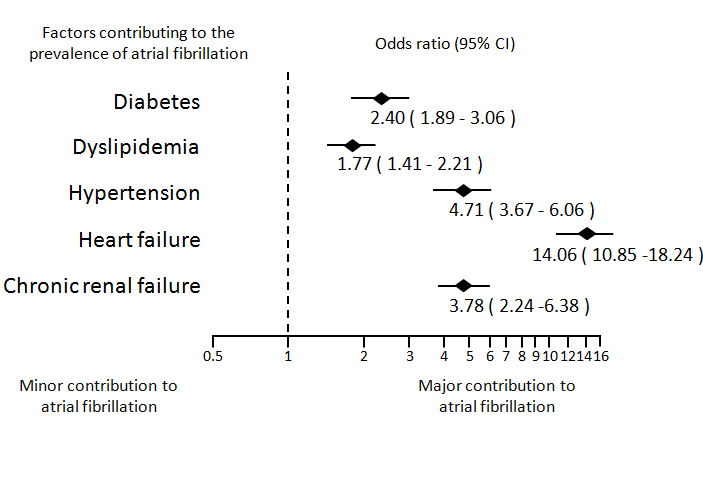
We first investigated the relationship between AF and metabolic diseases (DM, dyslipidemia). A significant relationship was seen between AF and diabetes. This means that diabetes is actually a risk factor of AF. The OR was 2.40 (95% confidence interval (CI); 1.89 - 3.06, p<0.0001) (Table 1). We next investigated the relationship between AF and dyslipidemia. There was also a significant relationship between them. The OR was 1.77 (95% CI; 1.41 - 2.21, p<0.0001) (Table 2).
Table 1. Relationship between the number of patients with atrial fibrillation and those with diabetes
|
AF |
Total |
Yes |
No |
DM |
Yes |
209 |
6,202 |
6,411 |
No |
100 |
7,127 |
7,275 |
Total |
309 |
13,329 |
13,868 |
Odd ratio = 2.40 (1.89 - 3.06)
Chi-squared = 54.012 (p<0.0001)
Table 2. Relationship between the number of patients with atrial fibrillation and dyslipidemia
|
AF |
Total |
Yes |
No |
DL |
Yes |
154 |
4,880 |
5,034 |
No |
155 |
8,679 |
8,834 |
Total |
309 |
13,559 |
13,868 |
Odd ratio = 1.77 (1.41 - 2.21)
Chi-squared = 24.458 (p<0.0001)
We then looked into the relationship between AF and cardiovascular diseases. We found that there was a significant relationship between AF and hypertension. The OR was 4.71 (95% CI; 3.67 - 6.06, p< 0.0001) (Table 3). We similarly analyzed heart failure, and we found that it is also a significant risk factor of AF. The OR of heart failure was as high as 14.06 (95% CI; 10.85 -18.24, p< 0.0001) (Table 4).
Table 3. Relationship between the number of patients with atrial fibrillation and those with hypertension
|
AF |
Total |
Yes |
No |
HTN |
Yes |
223 |
4,811 |
5,034 |
No |
86 |
8,748 |
8,834 |
Total |
309 |
13,559 |
13,868 |
Odd ratio = 4.71 (3.67 - 6.06)
Chi-squared = 175.848 (p< 0.0001)
Table 4. Relationship between the number of patients with atrial fibrillation and those with heart failure
|
AF |
Total |
Yes |
No |
CHF |
Yes |
96 |
421 |
517 |
No |
213 |
13,138 |
8,834 |
Total |
309 |
13,559 |
13,868 |
Odd ratio = 14.06 (10.85 -18.24)
Chi-squared = 658.209 (p<0.0001)
Table 5. Relationship between the number of patients with atrial fibrillation and those with chronic renal failure
|
AF |
Total |
Yes |
No |
CRF |
Yes |
16 |
193 |
209 |
No |
293 |
13,366 |
13,659 |
Total |
309 |
13,559 |
13,868 |
Odd ratio = 3.78 (2.24 -6.38)
Chi-squared = 28.692 (p<0.0001)
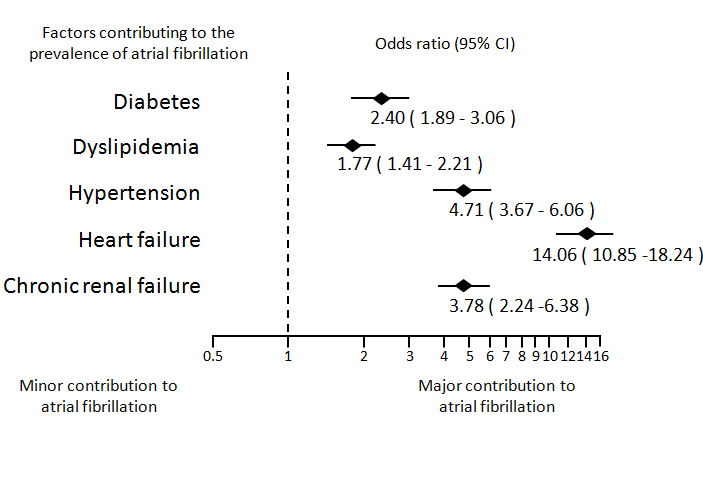
Figure 1. Summary of risk factors contributing to the onset of atrial fibrillation. A forest plot graph shows independent correlates of AF in patients with DM, dyslipidemia, hypertension, heart failure, and chronic renal failure.
We finally analyzed chronic renal failure, and we found that it is a significant risk factor of AF. The OR of chronic renal failure was as high as 3.78 (95% CI; 2.24 -6.38, p< 0.0001) (Table 5).
The results of risk factors contributing to the prevalence of AF are summarized in Figure 1.
Although several reports have reported an association between DM and AF, the results have been controversial and no large scale study has been reported in the real world clinical practice. To our knowledge, this is the first study which revealed the association in a large scale in the real world clinical practice.
Diabetes is important as one of the risk factors of the AF. Therefore, preventative treatment intervention is recommended, because the prognosis of asymptomatic patients with AF is poor. Early detection of the AF by periodical examination such as electrocardiography might be useful for the prevention of the onset of cerebral infarction for the patients with diabetes as well.
In general, onset frequency of the AF increase with the duration of DM. In many cases of DM, we found that paroxysmal AF tends to shifts to sustained AF, and finally to chronic AF. This is consistent with the experimental findings that atrial electromechanical function is impaired in diabetic rabbits, and is associated with atrial fibrosis and interatrial electrical conduction delay, promoting the onset of AF [9-11].
In conclusion, we demonstrated for the first time in a large scale investigation in Japan that DM would significantly increase the risk of the onset of AF. Therefore, it is recommended that patients with DM should take electrocardiography regularly and be intervened at an early stage in the real world clinical practice.
The authors report no conflicts of interest.
- 1. Inoue H, Fujiki A, Origasa H, Ogawa S, Okumura K, et al. (2009) Prevalence of atrial fibrillation in the general population of japan: An analysis based on periodic health examination. Int J Cardiology; 137:102-107. [Crossref]
2021 Copyright OAT. All rights reserv
- 2. Gage BF, van Walraven C, Pearce L, Hart RG, Koudstaal PJ, et al. (2004) Selecting patients with atrial fibrillation for anticoagulation: Stroke risk stratification in patients taking aspirin. Circulation 110:2287-2292. [Crossref]
- 3. Olesen JB, Lip GY, Hansen ML, Hansen PR, Tolstrup JS, et al. (2011) Validation of risk stratification schemes for predicting stroke and thromboembolism in patients with atrial fibrillation: Nationwide cohort study. Bmj 342:d124. [Crossref]
- 4.
Management AIAFF-uIoR (2002) Baseline characteristics of patients with atrial fibrillation: The affirm study. Am Heart J 143:991-1001. [Crossref]
- 5.
Huxley RR, Filion KB, Konety S, Alonso A (2011) Meta-analysis of cohort and case-control studies of type 2 diabetes mellitus and risk of atrial fibrillation. Am J Cardiology108:56-62. [Crossref]
- 6.
Frost L, Hune LJ, Vestergaard P (2005) Overweight and obesity as risk factors for atrial fibrillation or flutter: The danish diet, cancer, and health study. Am J Medicine. 118:489-495. [Crossref]
- 7.
Ruigomez A, Johansson S, Wallander MA, Rodriguez LA (2002) Incidence of chronic atrial fibrillation in general practice and its treatment pattern. J Clin Epidemiol 55:358-363. [Crossref]
- 8.
Watanabe H, Tanabe N, Watanabe T, Darbar D, Roden DM, et al. (2008) Metabolic syndrome and risk of development of atrial fibrillation: The niigata preventive medicine study. Circulation. 117:1255-1260. [Crossref]
- 9.
Chowdhry MF, Vohra HA, Galinanes M (2007) Diabetes increase apoptosis and necrosis in both ischemic and nonischemic human myocardium: Role of caspases and poly-adenosine diphosphate-ribose polymerase. J Thoracic Cardiovascular Surgery 134:124-131, 131 e121-123. [Crossref]
- 10. Fu H, Liu C, Li J, Zhou C, Cheng L, et al. (2013) Impaired atrial electromechanical function and atrial fibrillation promotion in alloxan-induced diabetic rabbits. Cardiology J 20:59-67. [Crossref]
- 11. Liu T, Zhao H, Li J, Korantzopoulos P, Li G (2014) Rosiglitazone attenuates atrial structural remodeling and atrial fibrillation promotion in alloxan-induced diabetic rabbits. Cardiovascular Therap 32:178-183. [Crossref]