Abstract
Invasive cervical root resorption (ICR) is an uncommon external root resorption which initiates at the cervical aspect of the tooth. ICR is a rare entity with an estimated frequency of less than 0.1% and could be misdiagnosed as cervical root caries. This can result in inappropriate management of the lesion with continuing resorption and eventual loss of tooth. This case highlights the need to increase the awareness of this uncommon clinical entity and the role of cone beam CT in its diagnosis and treatment planning. This case report involves a case of cervical root resorption which was initially misdiagnosed and managed as gingivitis, root sensitivity, pulpitis and trauma from occlusion. It was later diagnosed with cone beam CT and the lesion microsurgically removed and restored with resin filling material. The cone beam CT could contribute in avoiding any practice of iatrogenic dentistry is emphasized, as effective management can only be carried out if the exact location and nature of the lesion is understood.
Key words
root defect, sensitivity, subgingival root filling, cone beam computed tomography, panoramic radiography
Aim and objective of the article
A clinical case is presented to demonstrate the importance of CT scanning and its necessity. To be able to reach a definitive diagnosis with 3D imaging during treatment planning in spite of misleading chief complaint.
Introduction
Cervical external resorption also called as invasive cervical resorption is a clinical term used to describe a relatively uncommon, insidious and often aggressive form of external tooth resorption, which may occur in any tooth of permanent dentition [1-14]. Invasive cervical resorption is defined as ‘a localized resorptive process that commences on the surface of root below the epithelial attachment and the coronal aspect of the supporting alveolar process, namely the zone of the connective tissue attachment [2]. Radiographic features of lesions vary from well-delineated to irregularly bordered mottled radiolucencies, and these can be confused with dental caries. A characteristic radiopaque line generally separates the image of the lesion from that of the root canal, because the pulp remains protected by a thin layer of predentin until late in the process. Histopathologically, the lesions contain fibrovascular tissue with resorbing clastic cells adjacent to the dentin surface. More advanced lesions display fibro-osseous characteristics with deposition of ectopic bonelike calcifications both within the resorbing tissue and directly on the dentin surface [2].
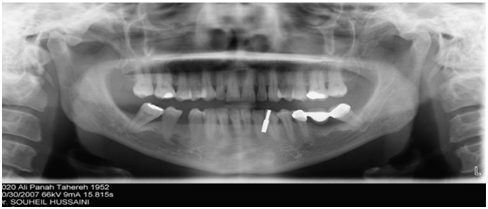
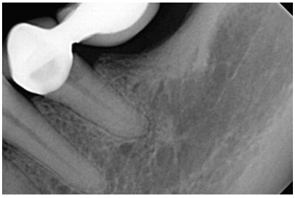
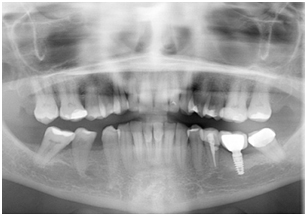
A 61 year non smoking female with history of heart problem with controlled medication. Chief complaint “An irritating discomfort on a tooth in the left lower jaw” that requires examination for either a filling or root sensitivity. The patient was examined with a panoramic (Figure 1) radiograph achieved and followed with peri-apical (Figure 2) and also no definitive diagnosis was made and hence further investigations lead to the definitive diagnosis.
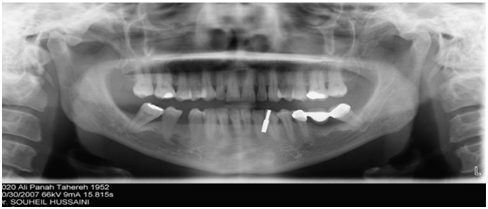
Figure 1. Initial panoramic radiograph
Case report
A 61-year-old non smoking female with no medical history with a Chief complaint of an irritating pain on left lower quadrant (FDI # 35) that requires examination for her localized chronic discomfort. During the evaluation of panoramic radiograph (Figure 1), no anatomic or etiologic factor for her chief complaint was detected hence, a periapical radiograph (Figure 2) was taken and the result of which were also inconclusive. Provisional diagnosis was root sensitivity and patient induced mild periodontal marginal gingivitis due to gingival irritation. Prophylaxis cleaning and scaling was performed. The patient returned with the same chief complaint and a Palliative treatment with desensitizer fluoride gel (Appendix 1) also was performed and given to the patient for 2 weeks home application. The patient returned with the same chief complaint and the next provisional diagnosis was muscular in nature and hence low level laser therapy (LLL) 1200J /300 seconds therapy (Figure 3) (Appendix 2) was performed for 2 sessions with 3 day intervals with no effective results.
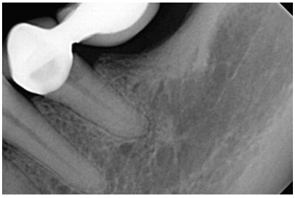
Figure 2. Initial periapical radiograph

Figure 3. Biolase laser used for LLL (Low level Laser Therapy)
The patient returned with the same chief complaint and the patient was then referred to an endodontist and root canal treatment on #35 performed. The chief complaint remained as it is. The chief complaint was not resolved and the missing tooth in #36 was planned for an implant (Appendix 3) with the rationale that if we were to balance the force distribution the load on tooth #35 could be controlled and the chronic irritating stimulus disappear. The bridge was sectioned and 3 single fixed restorations were advised with an implant supported fixed partial denture in #36 area.
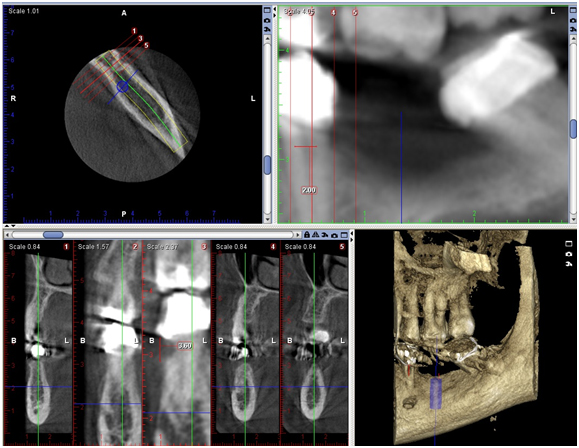
The patient was inquired about the findings in order to know whether she had any sensorial disturbance in the region of the LLQ. She presented no sensorial bilateral disturbance in the regions supplied by the mental nerve. In the panoramic radiograph, the right and left mental foramen (MF) were observable and not relevant to the chief complain, as a normal expected radiolucent area between the left mandibular premolars (Figure 1). For accurate implant placement A CBCT (Appendix 4) images were evaluated in axial, coronal and transversal reformatations (Figure 4), using 1.00 mm slice thickness for implant placement on #36. The image corresponding to the LLQ was clearly demonstrating a depression in the root area above the crestal bone level in the assessed CBCT slices. The measurement of the ICR lesion height and width (3.6/2.0 mm, respectively) was measured using ‘‘distance’’ tool of the software in the most representative CBCT transversal slice (Figure 5).
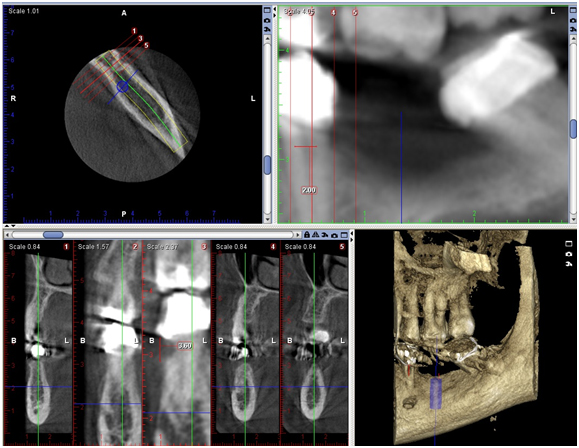
Figure 4. CBCT images
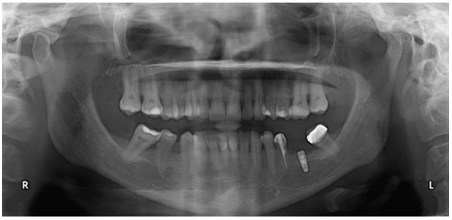
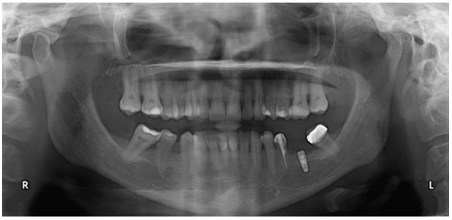
Figure 5. OPG taking at the time of implant surgery
CBCT is a modern technology, which allows the evaluation of maxillofacial structures in three dimensions (sagittal, axial and coronal). CBCT has many advantages such as absence of superimposition of structures in obtained slices, acquisition of a 3-D reconstruction, as well as use of lower radiation doses in comparison to medical CT [15-24]. MF location, size, shape and its possible variations can be properly assessed by CBCT [24].
At the time of the implant surgery the ICR lesion was attended to, the lesion was cleaned and restored with a Composite Resin restoration (Appendix 5) while maintaining absolute moisture control. An OPG (Figure 5) was taking at the time of lesion restoration demonstrating adequate seal of the ICR lesion with the Resin restoration. A Three year follow up panoramic radiograph (Figure 6) was taken which demonstrated successful cassation of the Invasive cervical resorption, an Increase in the surrounding bone level and a symptom free patient.
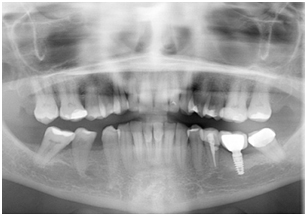
Figure 6. A 3 year follow up OPG
Differential diagnosis in time line and the treatment performed accordingly
Mild gingivitis: scaling and polishing (30/10/2012), root sensitivity: fluoride gel application (07/11/2012), muscular fatigue: Low level laser therapy(5 sessions over a period from (10/11/2012-25/11/2012), partial pulpal necrosis: root canal treatment (28/11/2012), trauma from occlusion: single crowns on each tooth and implant placement on edentulous area(25/12/2012), ICR: Composite Resin restoration (25/12/2012).
Conclusion
Early detection of a lesion is essential for successful management of Invasive Cervical Resorption. For patients with an ICR lesion with no apparent identifiable etiologic factor to achieve appropriate diagnosis and management CBCT appears to be a promising diagnostic tool.
References
- Kandalgaonkar SD, Gharat LA, Tupsakhare SD, Gabhane MH (2013) Invasive cervical resorption: a review. J Int Oral Health 5: 124-130. [Crossref]
- Tronstad L (1988) Root resorption--etiology, terminology and clinical manifestations. Endod Dent Traumatol 4: 241-252. [Crossref]
- Vasconcelos Kde F, Nejaim Y, Haiter Neto F, Bóscolo FN (2012) Diagnosis of invasive cervical resorption by using cone beam computed tomography: report of two cases. Braz Dent J 23: 602-607. [Crossref]
- Charara K, Ionescu A, Gagliardi J (2014) "Surgical Management of Invasive External Cervical Root Resorption Aided by Cone-Beam Computed Tomography: A CASE REPORT."
- Kesary R, Mengji AK, Yaga US, Panta P (2014) An unusual case of idiopathic multiple invasive cervical resorption. J Ind Acad Oral Med Radiol 26: 229.
- Tavares WL, Lopes RC, Oliveira RR, Souza RG, Henriques LC, et al. (2013) Surgical management of invasive cervical resorption using resin-modified glass ionomer cement. Gen Dent 61: e16-18. [Crossref]
- Jiang YH, Lin Y, Ge J, Zheng JW, Zhang L, et al. (2014) Multiple idiopathic cervical root resorptions: report of one case with 8 teeth involved successively. Int J Clin Exp Med 7: 1155. [Crossref]
- Gayathri P, Pandey RK, Jain E (2014) Management of internal resorption of central incisor using hybrid technique. BMJ Case Rep 2014. [Crossref]
- Umer F, Adnan S, Raza Khan F (2013) Conservative management of invasive cervical resorption: a case report. J Dent (Tehran) 10: 289-295. [Crossref]
- Johns DA, Shivashankar VY, Maroli RK, Joseph R (2013) Invasive cervical root resorption: Engineering the lost tissue by regeneration. Contemp Clin Dent 4: 536-539. [Crossref]
- Royzenblat, Alexander L, Tordik CPA , Goodell CG (2005) "Cervical resorption." Clin Update 27: 1-2.
- Arora A, Acharya SR, Muliya VS, Sharma P (2012) Multiple idiopathic cervical resorption: a diagnostic dilemma. Quintessence Int 43: 187-190. [Crossref]
- Moody AB, Speculand B, Smith AJ, Basu MK (1990) Multiple idiopathic external resorption of teeth. Int J Oral Maxillofac Surg 19: 200-202. [Crossref]
- Macdonald-Jankowski D (2005) Multiple idiopathic cervical root resorption most frequently seen in younger females. Evid Based Dent 6: 20. [Crossref]
- Angel JS, Mincer HH, Chaudhry J, Scarbecz M (2011) Cone-beam computed tomography for analyzing variations in inferior alveolar canal location in adults in relation to age and sex. J Forensic Sci 56: 216-219. [Crossref]
- Apinhasmit W, Methathrathip D, Chompoopong S, Sangvichien S (2006) Mental foramen in Thais: an anatomical variation related to gender and side. Surg Radiol Anat 28: 529-533. [Crossref]
- de Freitas V, Madeira MC, Toledo Filho JL, Chagas CF (1979) Absence of the mental foramen in dry human mandibles. Acta Anat (Basel) 104: 353-355. [Crossref]
- Fishel D, Buchner A, Hershkowith A, Kaffe I (1976) Roentgenologic study of the mental foramen. Oral Surg Oral Med Oral Pathol 41: 682-686. [Crossref]
- Greenstein G, Tarnow D (2006) The mental foramen and nerve: clinical and anatomical factors related to dental implant placement: a literature review. J Periodontol 77: 1933-1943. [Crossref]
- Haghanifar S, Rokouei M (2009) Radiographic evaluation of the mental foramen in a selected Iranian population. Indian J Dent Res 20: 150-152. [Crossref]
- Hasan T, Fauzi M, Hasan D (2010) Bilateral absence of mental foramen—a rare variation. Int J Anat Variat 3:167–169.
- Jacobs R, Mraiwa N, Van Steenberghe D, Sanderink G, Quirynen M (2004) Appearance of the mandibular incisive canal on panoramic radiographs. Surg Radiol Anat 26: 329-333. [Crossref]
- Liang X, Jacobs R, Lambrichts I (2006) An assessment on spiral CT scan of the superior and inferior genial spinal foramina and canals. Surg Radiol Anat 28: 98-104. [Crossref]
- Naitoh M, Hiraiwa Y, Aimiya H, Gotoh K, Ariji E (2009) Accessory mental foramen assessment using cone-beam computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 107: 289-294. [Crossref]