Abstract
This is a descriptive and analytical longitudinal study that asseses the management of type 2 diabetes mellitus (T2DM), the treatment of T2DM and the prevalence of complications in T2DM with the aim to evaluate the effectiveness of recommended actions and to assess the patient's disease profile in follow up analysis. We analyzed the medical records of patients with T2DM in follow up at the Endocrinology Reference Center in Santa Casa Medical School. Due to the chronic pathology of T2DM, which is characterized by population heterogeneity and phenotypic complexities, T2DM is responsible for increased complications, morbidity and mortality, especially cardiovascular and cerebrovascular disease, all of which explain our interest in demonstrating the epidemiological characteristics of follow-up in patients in our medical service. By analyzing patients medical records as part of a follow-up procedure, we have a wider visualization of the pathology of T2DM and thus the possibility of better clinical management.
Key words
type 2 diabetes mellitus, prevalence, diabetes complications
Introduction
T2DM is a metabolic disorder that is known as one of the principal causes of mortality worldwide. It has been present in 90.0%-95.0% of diabetes cases, according to International Diabetes Federation (IDF). Most of these patients have been overweight or obese and also suffer from related diseases: hypertension; dyslipidemia; polycystic ovary syndrome and vascular diseases. T2DM can occur at any age, but it is usually diagnosed after the age of 40 [1-3].
American Diabetes Association (ADA) showed in 2012 that 29.1 million Americans, or 9.3% of the population, had a diabetes diagnosis. Of the 29.1 million, 21.0 million were diagnosed and 8.1 million were undiagnosed. The percentage of Americans age 65 and older remains high, at 25.9%, or 11.8 million seniors (diagnosed and undiagnosed), while, approximately 1.4 million Americans are diagnosed with T2DM every year [2].
Recent studies in Brazil demonstrated that T2DM accounted for 5.3% of all deaths in 2011, with a mortality rate of 33.7 deaths per 100,000 inhabitants, despite the reduction of 1.7% per year recorded in the period 2000-2011. The mortality from acute complications of the disease, almost always preventable by emergency service, showed a rate of 2.45 deaths per 100 thousand inhabitants in 2010 [3,4].
According to recent estimates by the IDF, the number of patients living with T2DM globally is about 382 million. T2DM likely will become the most prevalent health issue worldwide as the number of patients is expected to reach 592 million by 2035. This increase has been attributed to lifestyle changes and the environment resulting from industrialization. According to Narayan, it is also important to consider in this process the demographic and epidemiological transition that occurred in the last century [1,5-7].
Quantifying the prevalence and evaluating the attention given to patients with this condition is essential for a rational planning of financial resources and expenses associated with the disease and its complications, especially considering the fact that adherence to long-term treatment is around 50% in developed countries and about 20% in developing countries [5-8].
Direct costs for the care of T2DM range from 2.5% to 15.0% of national health spending. The variance depends on local prevalence and complexity of treatment available. Patients with T2DM need at least two to three times more resources to care for their health than non-diabetics. In the United States, the total costs of diagnosed T2DM were $245 billion in 2013, $176 billion for direct medical costs and $69 billion in reduced productivity. In addition to financial costs, people with diabetes often suffer from pain, anxiety, inconvenience and lower quality of life for themselves and their families. Additionally, people diagnosed with T2DM can alsobe seen as a burden to society as a result of lost productivity at work, early retirement and premature mortality [1,5-8].
Population heterogeneity and phenotypic complexities complicate the management of T2DM amongst most patients. Few studies have been done to understand follow up treatment and identify the possible causes of failure even with many drug options available [1,2,9].
In this context, we established our interest in assessing T2DM management at the Endocrinology Reference Center in Santa Casa Medical school to identify, amongst other factors, the complication prevalence in this service health population in relation to the national average of 7.51%, the treatment follow-up and related complications [8].
Aim
The aim of this study is to assess the prevalence of complications in T2DM patients undergoing treatment at the Endocrinology Reference Center in Santa Casa Medical School and to evaluate epidemiological characteristics, treatment management and related diseases.
Methods
Retrospective longitudinal study approved by the Research Ethics Committee (REC) of Santa Casa Medical School. The study relied on data obtained and analyzed from the medical records of 129 patients with T2DM in follow-up at the Endocrinology Reference Center.
The personal characteristics of patients with T2DM observed in this study are as follows: Sex: male, female, Age range: 30-39; 40-49; 50-59; 60-69; 70-79 and 80 and over; socioeconomic characteristics of patients observed in this study are distinguished primarily by education according to years of study. The following strata are used: uneducated; 1 to 4 years; 4 to 8; 8-12 years and more than 12 years. With regards to a previous diagnosis of T2DM, patients observed in this study exhibited a plasma glucose value of fasting equal to or greater than 126 mg/dL, a value observed in both measures, and plasma glucose levels two hours after ingestion of seventy-five grams of glucose equal to or greater than 200 mg/dL and glycated hemoglobin greater than or equal to 6.5%. All of these values have been recently reviewed by the Brazilian Society of Diabetes and approved by the World Health Organization. The symptoms that lead the diagnosis were high frequent urination, excessive thirst, increased hunger, weight loss, tiredness, lack of interest and concentration, a tingling sensation or numbness in the hands or feet, blurred vision, frequent infections, slow-healing wounds, vomiting and stomach pain.
To assess T2DM risk factors, we collected medical records from patients with any of the following characteristics: 1) ages greater than forty-five years 2) Body Mass Index (BMI) greater than 25 kg/m2 3) first-degree relatives with T2DM 4) sedentary lifestyle 5) blood pressure above 140/90 mmHg or in medications use 6) prediabetes previously identified 7) history of gestational diabetes or macrosomic fetus8) polycystic ovary syndrome and vascular disease 9) high density lipoprotein (HDL-cholesterol) less than 45 mg/dl or triglyceride levels greater than 200 mg/dl, or in medications use 10) waist circumference greater than 80 cm (female) and greater than 94 cm (male), according to IDF.
Regarding the treatment of T2DM, we assessed the following management strategy: education, lifestyle modification, increased physical activity and reorganization of eating habits, along with concomitant treatment of other risk factors and medications.
The data were stored and analyzed by the software Epi Info version 3. 3. 2, tab to WindowsR platform, statistical significance p <0.05
Results
The prevalence of patients assessed in follow up in the Endocrinology ambulatory, were women, with 69.80%, the age range is 60-69 years with 47.70% and education less than 4 years of 74.40%. (Table 1)
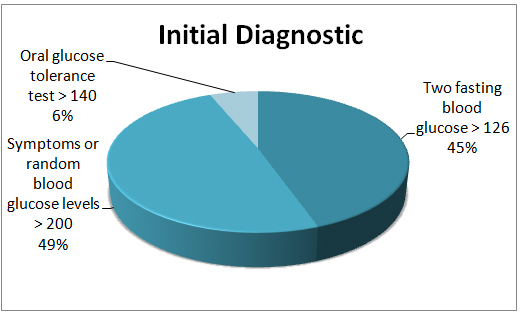
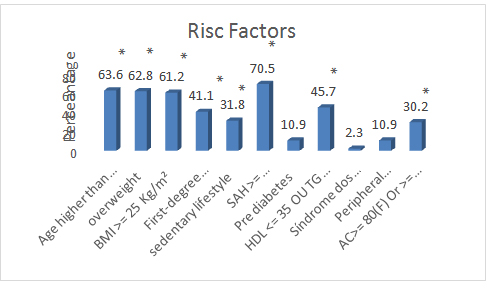
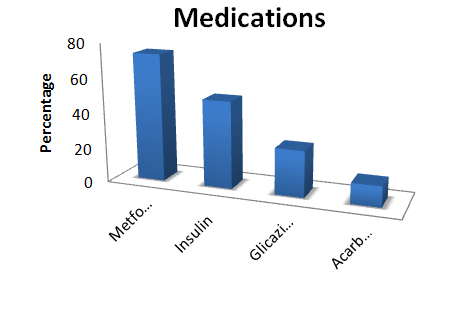
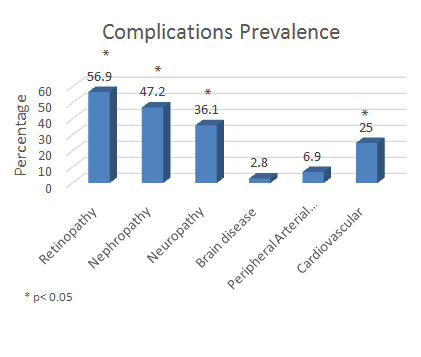
The prevalent method of initial diagnostic was symptoms or glucose random above 200 mg/dl in 49% of the analyzed (Figure 1). The identification of risk factors, 63.6% of cases, patients had more than 45 years. In 62.8% of cases the patients were overweight. In 41.1% it was reported that the patient had first degree relative with T2DM. Hypertension arterial systemic was present in 70.5% of cases (Figure 2).
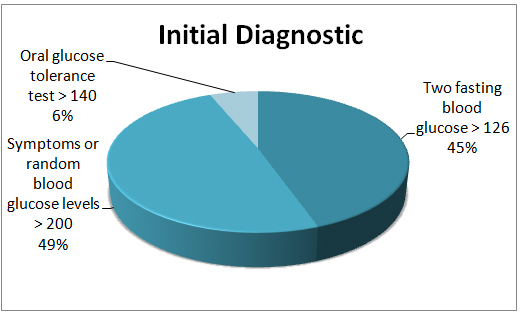
Figure 1. Diagnostic initial assessed
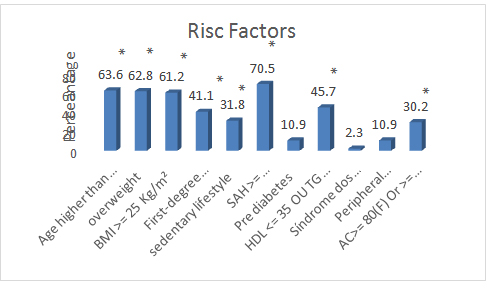
Figure 2. Analysis of risk factors related in patients with T2DM
*p< 0.05; SAH: Systemic Arterial Hypertension
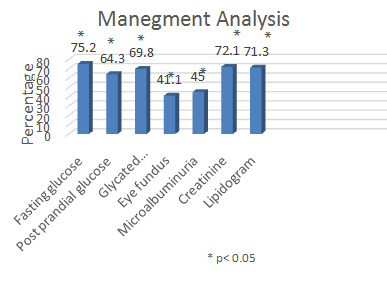
We have assessed the goal of treatment recommended by the DCCT and UKPDS, which have been Achieved mostly the target with high percentages, however, with reservations in eye fundus, due to not depend directly from our unit (Figure 3) [10,11].
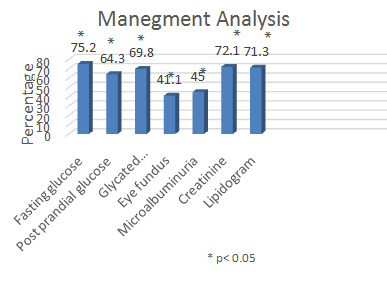
Figure 3. Analysis in laboratorial tests management
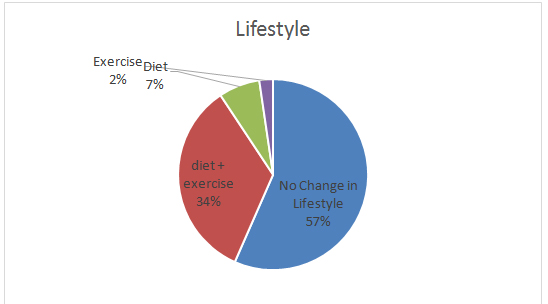
Unfortunately, the change of habit of life, much emphasized in the consultations, still keeps impaired mostly (Figure 4). While the medications used, as provided by the government and recommended as initial treatment, presents metformin prevalent (Figure 5) [1,2]. Of complications, retinopathy and nephropathy are the most prevalent in our Endocrinology unit (Figure 6).
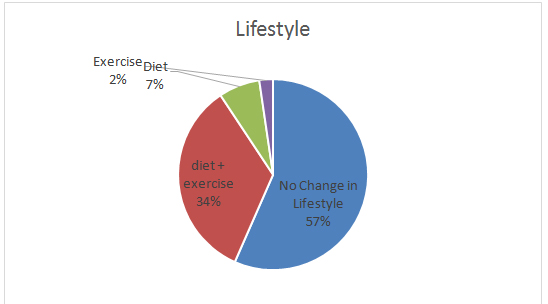
Figure 4. Analysis of change lifestyle
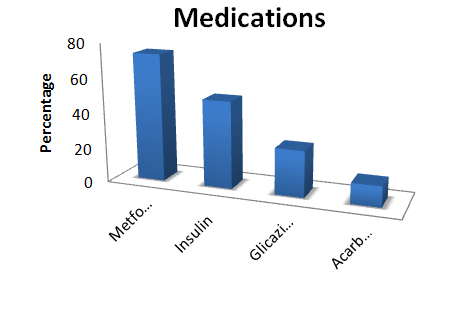
Figure 5. Pharmacological treatment
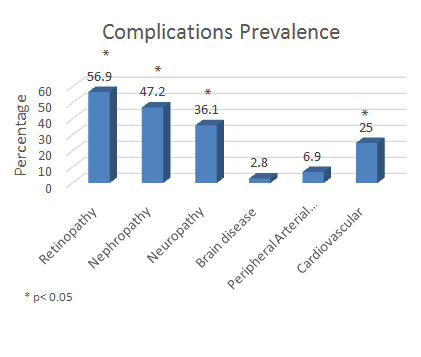
Figure 6. Prevalence of complications in T2DM patients
Discussion
The T2DM treatment and follow up is heterogeneous, which makes understanding the clinical and laboratory aspects of each individual the key better management of this challenging pathology. Unfortunately, few studies reveal the epidemiologic characteristics of each T2DM treatment center [2,3,9].
Our study demonstrated similar numerical results in gender, with increased female prevalence, compared to other Brazilian services statistics. Increased demand for female services, especially during pregnancy, and awareness amongst women about the importance of taking care of health may explain this female prevalence. Otherwise, a review in United States conducted in 2004 showed an overall similar incidence in men and female, but in older ages females predominated [12,13].
Regarding the age of onset, prevalence is 60 to 69 years old. In Brazil and in the state of São Paulo, however, 50-59 years old is the predominant age. The incidence and prevalence of T2DM markedly increases with age, particularly after subjects turn forty. Some studies reveal that in chronic diseases, there exists a remarkable prevalence between age and T2DM. In this context, increasing age is associated with reduced physical activity and, in some situations, changes in metabolism resulting from aging itself even when eating habits remain unchanged. Because of the increased risk of diabetes in older patients it is necessary to track risk factors of the disease in people from age 45, when increases the occurrence of the disease, in order to obtain earlier diagnoses [9,13,14].
The T2DM tends to be more prevalent among people of lower education. Previous results of a cohort study conducted in six Brazilian capitals showed that the overall prevalence and the previously diagnosed diabetes was lower among the population level of higher education, while we found a 65% higher adjusted prevalence among adults who did not complete Fundamental (is Fundamental the equivalent of high school? Or college? You need to clarify) [15,16].
The fact that the T2DM occurs more frequently in the population with limited access to health services demonstrates not only the influence of social determinants in health, but also the role of the education level and attitudes taken by the individual regarding their own health [17].
Although population-based studies are rare in Brazil, the few studies that have been conducted reveal epidemiology about realization of diagnostics criteria. The most important finding in these studies was that symptoms and glycemic higher than 126 mg/dl twice. A lower frequency in routine medical consultations likely explains this result [4].
In terms of diagnosing the T2DM, risk factors are an important place to start. In 91.18% of cases, risk factors were present. Obesity is one of the most prevalent comorbidities with T2DM. Our study supports this theory, as does a study by Kuhn and Araujo thatfound that only 32% of diabetic patients had normal body mass index, while 32% were in the overweight range and the majority, 36%, were obese. According to the Brazilian Society of Diabetes, it is estimated that 60% to 90% of diabetes patients are obese [18].
Another important risk factor is whether or not any first degree relatives suffer from diabetes. In our study, we found that 67.65% of diabetes patients had first-degree relative with T2DM. T2DM especially has a genetic hereditary factor that is greater than in type 1. Additionally, those who identified as having first-degree relatives with T2DMwere two to six times more likely to develop T2DM than patients with no family history [8].
As for lifestyle, most of the patients are sedentary. The lack of physical activity has an important correlation with genetic susceptibility. Lack of physical activity also is associated with increased insulin resistance, yet another risk factor that leads to diabetes. Finally, lack of physical activity can promote obesity, which as discussed previously isitself is a major risk factor for T2DM [19-21].
According to some studies, T2DM and arterial hypertension are generally related diseases. The importance of blood pressure detection is one of the criteria for detecting diabetes in asymptomatic individuals. Cardiovascular risks may worsen significantly with the association of hypertension and T2DM. Our study demonstrated the same higher prevalence results in this association as did other surveys [10,16,17,22].
The prevalence of dyslipidemia in our study was similar to other studies, with high Triglycerides and low HDL. Some surveys even demonstrated variability in the dyslipidemia population prevalence [23,24].
Peripheral arterial disease (PAD) is a condition characterized by atherosclerotic occlusive disease of the lower extremities, which leads to a higher risk factor for lower-extremity amputation. Additionally, those who suffer from PAD are more likely to have symptomatic cardiovascular and cerebrovascular disease. 12 million people in the U.S. suffer from PAD, and it is uncertain how many of those also have T2DM. Data from the Framingham Heart Study revealed that 20% of symptomatic patients with PAD had diabetes, but this is likely a gross underestimate given that many more people with PAD are asymptomatic rather than symptomatic. Unfortunately, there are few studies about prevalence. Our survey showed a higher association between T2DM and PAD [10,11,25-28].
Another important risk factor for T2DM is waist circumference, specifically circumference greater than 80 for women and greater than 94 for men. The distribution of fat around the waist indicates a health risk, and the ratio of waist circumference to hips is the measure most often used to diagnose adiposity [1,7,22].
The national complications incidence for diabetes is 7.51%, with the most common complications being diabetic foot, amputation, kidney disease and modified eye fundus. The last study conducted by WORLD HEALTH ORGANIZATION showed that after 15 years of disease, 2% of affected individuals reported blindness, 10% reported severe visual illness and 30% to 40% reported some degree of retinopathy. Among other complications, 10% to 20% of individuals had nephropathy, 20% to 35% had neuropathy, and 10% to 25% had cardiovascular diseases. Our study revealed a prevalence of complications in over half of the patients analyzed. Our study also showed a higher incidence in retinopathy and nephropathy diseases. Population phenotype and/or conditions of diagnosis may help explain the discrepancies between the findings in our study and the study conducted by the WHO [22,29,30].
A forthcoming study revealed that many diabetes patients were referred from other health services and often received incomplete solicitation in the initial diagnosis received from the public health system. What is more, the number of patients who follow up in our service directly relates to the frequency of consultation and solicitation tests overall. The United Kington Prospective Diabetes Study Group recommends that patients at risk of a T2DM (UKPDS) [22,24].
It has been established previously physical activity in combination with a balanced, nutritious diet are essential for the treatment of diabetes, because together they help decrease the amount of fat cells, while also reducing visceral fat and insulin resistance. As with other studies, patients in our study exhibited a low proclivity for proper diet and exercise habits [1-3,25].
In the case of prescription medication, the American, European and Brazilian Diabetes Society recommend metformin, with necessary changes to diet and exercise, to a high number of patients. However, it is important to emphasize that due to the public health system in Brazil, many patients do not have the financial resources afford treatment with medications. Because of the lack of affordability, few drug treatment options exist [26,27,29].
The national complications incidence is 7.51%, such as diabetic foot, amputation, kidney disease and modified eye fundus. The last study conducted by WORLD HEALTH ORGANIZATION showed that after 15 years of disease, 2% of affected individuals represented blindness, being 10% of those with severe visual illness and 30% to 40% with some degree of retinopathy. Among other complications, 10% to 20% of individuals had nephropathy 20% to 35% neuropathy and 10% to 25% cardiovascular diseases. Our study demonstrated prevalence of complications in over than a half of the patients analyzed, and also higher incidence in retinopathy e nephropathy diseases. It may be occurs depending the population phenotype and conditions of diagnosis [22,29,30].
The data in our study comes from a section of patients in follow up at the Endocrinology Reference Center who suffer from T2DM. Importantly, most of these patients are referred to the Endocrinology Reference Center from other health services with a diabetes diagnosis and difficulty managing the disease. Overall, our study reveals a prevalence of female and middle-aged adults with high risk comorbidity factors such as obesity, hypertension and dyslipidemia. There is also a significant association with family history of DM.
Conclusion
Our study demonstrated the importance of knowing the epidemiological profile and associated comorbidities of patients undergoing follow-up service for T2DM in order to establish the best treatment management approach for their T2DM and its complications. Ultimately, because T2DM is a multifactorial disease that exhibits phenotypic variability and increased morbidity and mortality, more epidemiological studies are needed in order to better understand and improve the therapeutic management of follow-up patients with T2DM.
References
- Ceriello A1, Colagiuri S (2008) International Diabetes Federation guideline for management of postmeal glucose: a review of recommendations. Diabet Med 25: 1151-1156. [Crossref]
- American Diabetes Association - < http://www.diabetes.org/diabetes-basics/statistics/#sthash.7QdcnSr6.dpuf>. Accessed in Jan.2016
- Diretrizes Da Sociedade Brasielira De Diabetes 2013-2014. . Accessed in: Jan.2016
- Prevale^ncia de diabetes autorreferido no Brasil: resultados da Pesquisa Nacional de Sau´de 2013. Epidemiol. Serv. Sau´de, Brasi´lia, 24(2): 305-314, abr-jun 2015 305
- World Healty Organization. Prevalence of diabetes worldwide. < http://www.who.int/diabetes/facts/world_figures/en/> . Accessed in Jan.2016
- Chen L1, Magliano DJ, Zimmet PZ (2011) The worldwide epidemiology of type 2 diabetes mellitus--present and future perspectives. Nat Rev Endocrinol 8: 228-236. [Crossref]
- Toscano, Cristiana M.. National screening campaigns for chronic non-communicable diseases: diabetes and hypertension. Ciênc. Saúde Coletiva, Rio de Janeiro, v. 9, n. 4, 2004
- Self-reported diabetes prevalence in Brazil: results from National Health Survey 2013, Epidemiol. Serv. Sau´de, Brasi´lia 24: 305-314.
- Nathan D, Buse J, Davidson M, Fer- rannini E, Holman R, et al. (2009) Medical Management of Hyper- glycemia in Type 2 Diabetes: A Consensus Algorithm for the Initiation and Adjustment of Therapy: A consensus statement of the Ame- rican Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care 32: 193-203.
- American Diabetes Association Position Statement (1993) Implications of the Diabetes Control and Complications Trial. Diabetes Care 19: S50-52.
- (1995) U.K. prospective diabetes study 16. Overview of 6 years' therapy of type II diabetes: a progressive disease. U.K. Prospective Diabetes Study Group. Diabetes 44: 1249-1258. [Crossref]
- Instituto Brasileiro de Geografia e Estati´stica. Pesquisa Nacional por Amostra de Domici´lios: um panorama da sau´de no Brasil – acesso e utilizac¸a~o dos servic¸os, condic¸o~es de sau´de e fatores de risco e protec¸a~o a` sau´de 2008. Rio de Janeiro: Instituto Brasileiro de Geografia e Estati´stica; 2010.
- Ministe´rio da Sau´de (2014) Secretaria de Vigila^ncia em Sau´de. VIGITEL Brasil 2013: vigila^ncia de fatores de risco e protec¸a~o para doenc¸as cro^nicas por inque´rito telefo^nico. Brasi´lia: Ministe´rio da Sau´de 164 p. (Se´rie G. Estati´stica e Informac¸a~o em Sau´de).
- Stopa SR, César CL, Segri NJ, Goldbaum M, Guimarães VM, et al. (2014) Self-reported diabetes in older people: comparison of prevalences and control measures. Rev Saude Publica 48: 554-662. [Crossref]
- Schmidt MI, Hoffmann JF, de Fátima Sander Diniz M, Lotufo PA, Griep RH, et al. (2014) High prevalence of diabetes and intermediate hyperglycemia - The Brazilian Longitudinal Study of Adult Health (ELSA-Brasil). Diabetol Metab Syndr 6: 123. [Crossref]
- American Diabetes Association (2013) Diagnosis and classification of diabetes mellitus. Diabetes Care 36 Suppl 1: S67-74. [Crossref]
- Barros MB, Francisco PM, Zanchetta LM, César CL (2011) [Trends in social and demographic inequalities in the prevalence of chronic diseases in Brazil. PNAD: 2003- 2008]. Cien Saude Colet 16: 3755-3768. [Crossref]
- Freitas LRS, Garcia LP (2012) Evolução da prevalência do diabetes e deste associado à hipertensão arterial no Brasil: análise da Pesquisa Nacional por Amostra de Domicílios, 1998, 2003 e 2008. Epidemiol Serv Saude 21: 7-19.
- Franco LJ (1988) Estudo sobre a prevalência do diabetes mellitus na população de 30 a 60 anos de idade no município de São Paulo. [dissertação]. São Paulo (SP): Escola Paulista de Medicina.
- Malerbi DA (1991) Estudo da prevalência do diabetes mellitus no Brasil.
- Ministério da Saúde (1993) Secretaria de Assistência a Saúde, Departamento de Assistência e Promoção à Saúde. Coordenação de Doenças Crônico-Degenerativas. Manual de Diabetes. 2nd ed. Brasília (DF): Ministério da Saúde, Brazil.
- (2012) Standards of Medical Care in Diabetes. Diabetes Care 35: S4-10.
- Martinez TLR, Santos RD, Armaganijan D, Torres KP, Loures-Vale A, et al. (2003) National alert campaign about increased cholesterol: determination of cholesterol level in 81.262 brazilians. Arq Bras Cardiol 80: 635-638.
- (1998) Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). UK Prospective Diabetes Study (UKPDS) Group. Lancet 352: 854-865. [Crossref]
- American Diabetes Association (2012) Standards of medical care in diabetes--2012. Diabetes Care 35 Suppl 1: S11-63. [Crossref]
- Lerario AC, Chacra AR, Pimazoni-Netto A, Malerbi D, Gross JL, et al. (2010) Algorithm for the treatment of type 2 diabetes: a position statement of Brazilian Diabetes Society. Diabetol Metab Syndr 2: 35. [Crossref]
- Marre M, Shaw J, Brändle M, Bebakar WMW, Kamaruddin NA, et al. (2009) Liraglutide, a once-daily human GLP-1 analogue, added to a sulphonylurea over 26 weeks produces greater improvements in glycaemic and weight control compared with adding rosiglitazone or placebo in subjects with Type 2 diabetes (LEAD-1 SU). Diabet Med 26: 268–278. [Crossref]
- Framingham Heart Study. Acessed in Jan.2016
- Nauck M, Frid A, Hermansen K, Shah NS, Tankova T, et al. (2009) Efficacy and safety comparison of liraglutide, glimepiride, and placebo, all in combination with metformin, in type 2 diabetes: the LEAD (liraglutide effect and action in diabetes)-2 study. Diabetes Care 32: 84-90. [Crossref]
- (2003) Diet, nutrition and the prevention of chronic diseases. World Health Organ Tech Rep Ser 916: i-viii, 1-149, backcover. [Crossref]
2021 Copyright OAT. All rights reserv