Three cases with keratoacanthoma, two female xerodemoid patients and one male non-xerodermoid patient presented with keratoacanthoma, in 2 patients located on the nose and one under the left eye.
They were treated with topical podophylline 25%solution once weekly. The response to therapy started after few weeks and complete resolution of the lesions occurred within around 2-4 months without topical or systemic side effects.
Keratoacanthoma (KA) is not uncommon skin tumor among healthy people [1], but is a common skin disease among patients with xeroderma pigmentosa [2], xerodermoid types and patients with immune suppression state [3,4], like patients with kidney transplants [5-10].
It has been documented that KA might have natural course of involution and spontaneous clearance [11,12], but this could be rarely recognized in clinical practice. As KA is rapidly growing [2,12,13] tumor that might cause local severe destruction of tissue and behave like squamous cell carcinoma especially when KA is located near important organs like nose and eyes [12,14]. Hence its treatment is mandatory, especially in early lesions where the curettage and cautery is the standard mode of therapy.
In many cases, the patients refuse surgery or in critical areas, the surgical treatment might leave obvious disfigurements that need further Plastic surgery [12].
Podophylline has been used in treatment of many skin diseases like, genital warts in infants [15] and cutaneous leishmaniasis [16]. Most recently, podophyllin 25% had been used as effective safe topical therapy for basal cell carcinoma [17], solar keratosis [18], so the aim of the present report is to study the effect of 25% podophylline as a topical therapy for KA.
Formal consent was taken before the start of the therapy, after full explanation about the nature of the disease, course, the procedure of treatment, follow up, prognosis and the need for pre and post treatment photographs. Also, ethical approval was performed by the Scientific Council of Dermatology and Venereology- Iraqi Board for Medical Specializations. Digital photographs were taken using SONY Cyber-Shot T300 10.1 MP for each patient in good illumination. The lesions treated with 25% topical podophylline in benzoin co solution once weekly for 6 weeks. And the Follow up was done after clinical cure every 3 months up to 18 months to record recurrence rate of the lesions after clinical recovery.
Podophyllum resin 25% topical solution USP prepared by mixing 25 grams of podophyllum resin in alcohol and then 10 grams of the alcohol-soluble extract of benzoin was added, and finally alcohol was added to make 100 ml. The solution was applied by a wood stick applicator to whole lesion with thin layer. The amounts used in each session depend on the size of lesion but always not exceeding 0.5 ml. The solution was allowed to dry in approximately 3 minutes and patients were instructed to wash off it after 5 hours. The solution was applied once weekly for maximum of 6 weeks and the number of applications depend on rate of response of the lesions [19,20] .
Case No. 1
A 25 years old female patient has xerodermoid disease since early childhood presented with big mass under the left eye of one month duration on 26th Feb, 2013 (Figure 1A).

Figure 1A. A 25 years old female patient with KA before therapy.
On examination, she had well defined classical crateriform KA with 1x1cm in size. She has surgery phobia as she thinks that operation may destroy her eye, accordingly podophylline 25% had been applied once weekly. Partial remission and involution started few weeks later and complete clearance occurred on 8th Sep 2013 that left acceptable cosmetic appearance with little scarring. During initial applications, podophylline can cause reactive erythema, swelling of lesion and crusting. Side effects were not seen during or after therapy. There was no relapse of lesion after 1.5 year follow up (Figures 1B, 1C and 1D).

Figure 1B. The same patient after one month of therapy

Figure 1C. The same patient after three months of therapy.

Figure 1D. Showing complete cure with minimal scar after six months of therapy
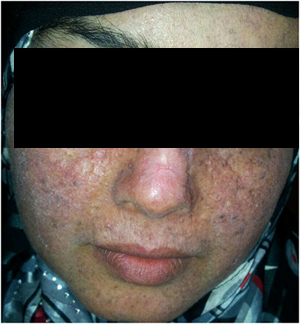
Case No. 2
A 27 years old female with typical history of xerodermoid skin disease since early childhood with positive family history. She was seen on 8th May, 2013 with depressed crateriform KA on the dorsum of the nose of 2 months duration (Figure 2A). She refused surgery as she thinks that operation can cause destruction of nose. After two months of podophylline once weekly application, the lesion completely disappeared but left small scar with very good cosmetic appearance. No side effects or complications were observed during the course of therapy or after. No recurrence of KA after one year of observation (Figures 2B and 2C).

Figure 2A. A 27 years old female patient with KA before therapy.

Figure 2B. The same patient after one month of therapy.
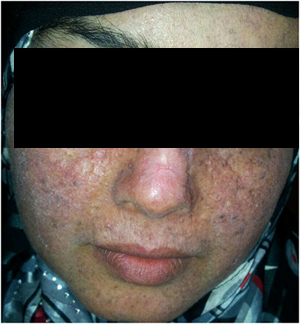
Figure 2C. The same patient after three months.therapy
Case No 3
A 37 years old healthy male patient was seen on 25th June, 2013 with typical KA on the right side of the nose of one month duration that overtime increased in size (Figure 3A).

Figure 3A. A 37 years old male patient with KA before therapy.T
He refused surgery as this procedure might cause damage to his nose. He was treated with podophylline 25 % once weekly and complete resolution was obvious on 9th Dec, 2013 leaving highly accepted cosmetic appearance with minimal scarring (Figures 3B and 3C). No complications or side effects were noted was not observed after 6 months follow up.

Figure 3B. The same patient after one month of therapy.

Figure 3C. The same patient after six months of therapy
Although it has been reported that KA might resolve spontaneous but this clearance might not occur or takes longer time during which, there is great psychological suffering [11,12]. The lesion could be locally destructive especially for vital organs like nose and eyes [12,14], hence its therapy is mandatory and waiting and see principle [2] should not be applied in this kind of tumor. Skin surgery either by curettage and cautery or by radical excision is the most important procedure that should be carried out [2,11,12]. But surgery might leave big damage to organs or surgery might be refused by patient [2,11,12]. In these situations one might look about alternative topical therapy. Podophylline has been effectively used in management of basal cell carcinoma [17] and solar keratosis [18] hence we conducted the present study and podophylline had shown very effective action against KA and without any complications or side effects with good cosmetic results. The safety of podophylline as a topical therapy was confirmed in many clinical situations like in treatment of; genital warts in infants, basal cell carcinoma, solar keratosis and cutaneous leishmaniasis [15-20]. The possible mechanisms of actions are as follow: It is an antimitotic and caustic agent, a lipid-soluble compound with cytotoxic properties that easily crosses cell membranes lead to inhibit cell mitosis and DNA synthesis by reversibly binds to tubulin; the protein subunit of the spindle microtubules, thereby preventing polymerization of tubulin into microtubules, cell division is arrested, and other cellular processes are impaired as it blocks oxidation enzymes in tricaboxylic acid cycle, so it will interfere with nutrition of cells, inhibits axonal transport, protein, RNA, and DNA synthesis and also inhibits mitochondrial activity and reduce cytochrome oxidase activity. It often causes local necrosis and death of tumor cells and erosion of the tissues [21-27].
Other topical therapies like 5 % immiquimod, 5-florouracil, photodynamic therapy with topical 8-aminolaevullinic acid have been used effectively in the treatment of KA [28-35].
In conclusion, podophylline 25 % is an effective safe topical therapy for KA and as alterative treatment to surgery.