Abstract
This article discusses and describes the interconnectedness (connecting the dots) of systems thinking as the overarching concept integrating the principle concepts of TeamSTEPPS®, interprofessional education (IPE) and interprofessional practice (IPP). Each in turn have different approaches of nomenclature and terminology, depending on the audience; yet have essentially the same overall principles and objectives. The strength and necessity of how systems thinking works is critical to all practitioners and educators; regardless of specialty; highlighting the necessity to integrate the common these principles to improve patient safety. The interconnectedness of TeamSTEPPS® and IPE/IPP are clearly applicable in such specialties as palliative care, emergency settings, general settings and many more. Literature is reviewed indicating support for these concepts, difficulties with variances in nomenclature and terminology, and recommendations.
Key words
IPE, IPP, Interprofessional education, interprofessional practice, TeamSTEPPS® language, nomenclature, terminology, communication, education, informatics, digital age
Introduction
Can we truly work by connecting all of the dots? What about the meaning and use of Teamstepps®, Interprofessional Education, and Interprofessional Practice? Are they directed at different user groups? In many respects they are. TeamSTEPPS® [1] is directed more for the active practitioner; whether nurse, physician, pharmacist, respiratory therapist (as examples) and for all areas of practice from both ends of the spectrum of life; in utero to end of life; such as practicing in the world of hospice and palliative care or the intensive care unit, as examples.
Interprofessional Education denotes, in many instances, educating students; whether pre-licensure or earning further degrees. Interprofessional practice is more in line with actively engaging in teams after initial licensure as health care providers. An example can be the functioning of teams in intensive care units or as with hospice and palliative care. Palliative care typically works with interprofessional teams; which has been the case since its inception [2]. Creating the connection between concepts of terms seems simple yet challenging. Even more so, is communication between professions in which technology is a dramatic driver in today’s healthcare [3].
Transparency of communication is critical to outcomes. We are working with electronic records which present challenges for providers and successes. Therefore, how we engage with the team, the language we use, what we document, can make the difference. And, connecting all (as we work toward a holistic approach) is the world of systems thinking.
There are many ‘dots’ we work with; such as engaging in transparent communication, using science and art, skills to work with electronic systems, working in interprofessional teams and respecting and valuing all members of the team. What we lack is consistent incorporation of this delivery modality when educating in the academic settings our pre-licensure students. To prepare those entering our workforce embedding the concepts of teams is critical and is within the world of systems thinking.
The purpose of the article is to discuss and describe connecting these concepts (dots) as they appear to be different depending on the audience. However, the strength and necessity of how systems thinking works is critical to recognize for all practitioners and educators; regardless of specialty.
Brief Literature Review
Systems thinking broad brush
We tend to handle issues linearly. Many variables that are out of our control can be critically important to include. Gehlert, Ressler, and Baylon [4] wrote: “The complexity of challenges cannot be successfully engaged using linear, reductionist thinking. Today’s complex challenges with globalization, global warming, economic instability, right to life issues, terrorism, scientific/technological breakthroughs, healthcare, religious and political differences and more have converged, creating gridlock and polarization in our society” (pp. 79-80). One might wonder what that has to do with healthcare, yet so many providers view and make decisions on linear thinking. Current curriculums continue to teach in a methodology, in many ways using reductionist thinking versus systems thinking.
Providers care for individuals that are a reflection of the society as a whole. Our educators speak to systems thinking however; do not fully integrate systems thinking in curriculums. In instances where system theory is prominent the connection with systems thinking is not adequately covered and applied. To successfully engage in systems thinking we must include all that impacts the whole. The question then is; are we missing out by viewing healthcare problems independently of the whole?
As an example of the many parts impacting the whole, Clark and Normile [5] examined patients admitted from the emergency department (ED) to the intensive care units (ICU). Many factors were noted to influence the timeliness to leaving the ED for the ICU. System issues attributed to longer stays in the ED for admitted ICU patients including lack of available ICU beds. One of the reasons for the lack of the ICU beds was waiting on floor beds to transfer patients out of the ICU; among many other system wide issues. Findings in this study indicated “the higher the ICU occupancy (fewer available beds) at the time of decision to admit was associated and suggested increased mortality” (p. 315). Additionally, “the higher mortality for the uninsured could be attributed partially to the greater number of co-morbidities” (p. 316).
Nomenclature/Terminology
Terminology and nomenclature are essentially the same; though in many ways different. Terminology is described as vocabulary we use [6] whereas, in the sciences nomenclature is a system of names that define and describe ‘things’ [7].
Many questions can be generated when we discuss healthcare language, whether of a discipline different than another, or when educating our patients with words they do not understand; as well as cultural differences and perspectives. As anatomic structures are described and discussed essentially the same between healthcare disciplines, why are there differences in the use of nomenclature and terminology between healthcare disciplines? Is this a behavioral science issue? Is it embedded in our discipline specific educational processes defining what words we use and how we communicate? What creates the barriers to communication between disciplines such as nursing and medicine? If we are polarized at opposite ends like protons and electrons pushing each other apart is there any way we can come back to the center and connect again?
In addressing these challenges a funded AHRQ study identified that a lack of nursing terminology leads to miscommunication potentially resulting in medical errors creating negative patient outcomes [8]. What makes up this lack of nursing terminology? Is it that nursing is so different than other healthcare providers in the language used when communicating? The problems we encounter with differences in terminology creates communication concerns between disciplines; leading to conflict, misunderstandings, misinterpretations, and even medical errors.
In a study by Clark et al. [9] a given word can be similar yet have a different meaning. An example is discussing clinicals for nursing students and pharmacy students. Pharmacy students do not readily use the term clinicals. The term used is experiential activities [9]. Teaching healthcare students’ phrases or terms used that have different meanings (even slightly) can lead to communication breakdowns. In a class composed of several different healthcare discipline students’ terms and abbreviations can be very different and or understood to have a slightly different meaning for each discipline. This can also occur for new practitioners just entering the workforce as well. As was noted with the AHRQ study [8] miscommunication creates the environment where there can be increased errors. This miscommunication can be for many reasons, one of which can be the language used.
Education/Practice
Dolensky and Moore [10], nursing educators, discuss the necessity of including systems thinking more in depth in our curriculums’. They discuss how nursing has focused very closely on the use of Quality and Safety for Education of Nurses (QSEN) for nearly a decade with its positive impact on quality of care. However, this narrow focus has a downside leaving out the crucial interactions impacting the system. Therefore, one might venture to say it is linier and reductionist thinking rather than systems thinking.
Scopes of practice
In today's healthcare delivery environment scopes of practice are not as discrete as they once were. Changes are taking place by legislative actions, governed by both national and state regulations.
The discipline of nursing tends to see scope of practice holistically. With this perspective nursing sees itself solely responsible to coordinate all care, education, interventions, and advocacy for the patient. This can and does result in a more tunneled vision or ‘linear’ approach to the delivery of care. Respiratory therapy has a narrow perspective as well with in-depth knowledge and skill sets focused on pulmonary and related conditions. Pharmacy too has a more narrowed specialized focus and knowledge base. However, medicine and many other disciplines profess a more holistic approach.
Academic training continues to be mainly discipline specific. By so doing the importance of systems thinking from a non-linear approach is lacking and diminishes the readiness for our new graduates entering the workforce to work in collaborative teams.
What about IPE in academic education?
Defining IPE has been challenging and many professions have stipulated definitions to guide curriculums. Several indicate interprofessional education should be completely infused in curriculums; yet without definitive steps and requirements. An example of more specific requirements can be found regarding pharmaceutical education. According to Buring et al. [11] the definition of IPE includes “both ‘students and educators’ should jointly work together in an interprofessional collaborative learning environment” (p.2). One can postulate from this definition if two professions of students are present then both professions should be represented by the respective faculty. This is one of the stumbling blocks many academic institutions face; not availing faculty representing the student professions to be present and active consistently throughout a course.
An example of where all faculties were consistently engaged in a course is a forensics course [5]. Three University programs and the three representative faculties collaborated engaging students with interprofessional concepts. The three disciplines of faculty included Nursing, Psychology, and Criminal Justice. Students worked in groups engaging with case studies recognizing that criminal justice and law are very much associated with interactions and communications with healthcare situations. This format of original training can and does impact how practitioners work within teams, collaborate, and value others expertise in many settings.
Interprofessional practice/communication
According to Clark et al. [9] an IPE class which also engaged in IPP included several disciplines in the care of the critically ill. The disciplines included Social Work, Pharmacy, Nursing, and Respiratory Therapy. Terminology was different depending on the discipline. Not all of the disciplines were familiar or had ever heard of the abbreviation SOAP or subjective, objective, assessment, and plan; a method of organizing information about a patient and documenting that information. A term or abbreviation used in Pharmacy education was ‘terminal performance outcomes’. Pharmacy uses the phrase Objective, Structured Clinical Examinations or OSCEs to describe practice in patient interviewing skills with actors. In nursing the term or phrase with the same meaning is Standardized Patient Interview or SPI. Though they are essentially the same skill to practice and learn neither discipline recognizes the similarities unless they are exposed to the other. Faculty that were unfamiliar with SOAP included Pharmacy, Respiratory Therapy and Social Work.
When we think in terms of educating our profession students we can see differences and overlaps. In this class the four disciplines working together in case studies and simulations, the nursing students approached interventions with the rationale they were responsible for all patient care; regardless of whether it was teaching about the use of inhalers or medications, as examples. What was most apparent was the lack of understanding and knowledge of the scopes of practice of each of the disciplines in this class and how to engage, collaborate, and use the expertise of each discipline to address patient care from a systems perspective.
Is TeamSTEPPS® different than IPE/IPP/patient centered care?
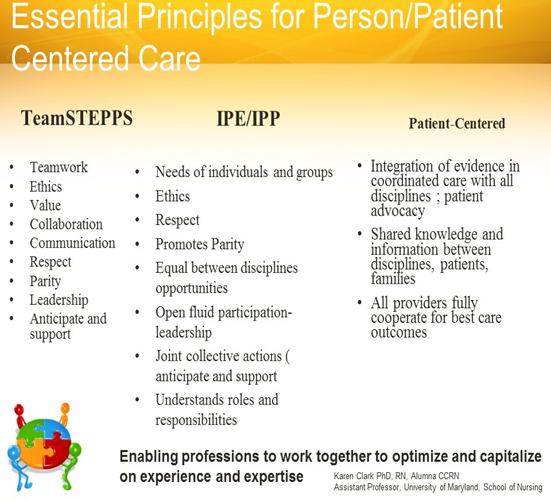
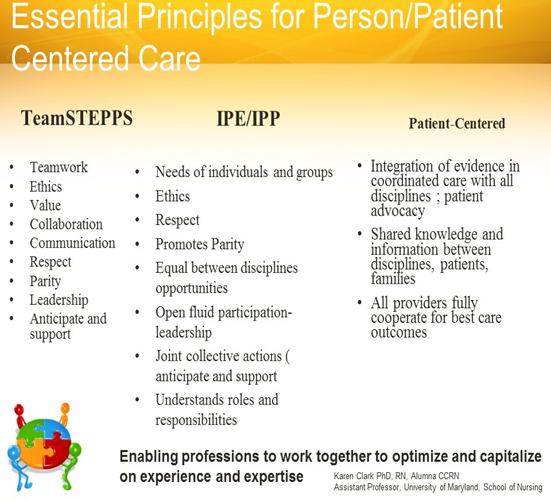
The concept of TeamSTEPPS® [1] highlights systems thinking as integral to collaboration, value, respect and effective communication within the interprofessional teams; which captures the full scope of ‘systems thinking’. TeamSTEPPS® nomenclature/terminology is similar to IPE/IPP and the principles/concepts are essentially the same. The minor differences are geared more to the practice environment versus the educational environment. However, in a presentation by Clark [12] the commonalities are interconnected even though IPE focuses more on educational endeavors and TeamSTEPPS® is geared to the practicing provider audience. Essential principles for Person/Patient Centered Care [12] engage same or similar vocabulary, concepts, and are patient centered (Appendix). Each of the categories noted with TeamSTEPPS®, IPE/IPP, and Patient Centered Care are essentially the same. Each focuses on somewhat different audiences to communicate and educate the importance of the principles for safe practice.
Appendix: Essential principles for Person/Patient Centered Care
Communication
One wonders how informatics, or information technology, fits when discussing teamwork, collaboration, communication, values and respect. All are critical to caring for any patient whether in hospital, clinic, at home, or at end of life (palliative care or hospice). We know the use of electronic healthcare records are used in many settings and can provide direct access to patient’s conditions and providers. Communication with this documentation format can increase the speed and accuracy of patient needs between care givers and providers. In 2009 the Health Information Technology (HITECH) Act was passed as part of the American Recovery and Reinvestment Act [13]. With this new law, providers were pushed to move toward the digital age. Many practitioners were reluctant to even consider digitalizing their medical records. Blogs and short articles on medical websites for various specialties explained the problems with going digital. Many also explained they did not have time nor valued the information contained in the electronic health records (EHR). Reese [14] expressed that doctors want to put together constellations of signs from complaints and do not value the numeric information contained in the EHR; whether check marks for choices or even posted lab results. One point Reese shared was the perspective of an Ophthalmologist that indicated he ignores EHR summaries as the summary does not tell the story of the patient, only the patient can explain the story (para. 9). Shortly after this article was published on the web in a healthcare blog another physician [15] wrote about the advantages of the EHR. He described the technology more in line with using a utility; that it is reliable, easy to access, and using the Cloud is cheaper than continually upgrading individual servers with hardware and software; much less concerns with crashes and downtime of the system. However, a disadvantage can be if the Cloud based vender is not dependable the entire network is in jeopardy. The two opposing viewpoints continue to be present however, EHRs and even embracing Cloud computing is here to stay. So, why is this important along with how we communicate?
As providers in the digital age, we are influenced by many outside forces and we do not necessarily recognize how critical this is from a systems thinking perspective. A key challenge is for all involved (in the system) to recognize patient experiences within an interconnected system. From a different point of view, the extrapolation of communication between providers, when using the EHR, is a more holistic approach when communicating with all providers synchronously and asynchronously.
Discussion
The more experience a provider gains in practice the more (depending on the provider or practitioner) they will engage in the team. This is a point that can be debated depending on the realm of the provider’s discipline; which leads to and encourages a continued fragmentation to the delivery of care.
At the center of the debate regarding practice and even entry into practice is few healthcare curriculums fully engage IPE in required coursework. Others may have, or not, limited integration of interprofessional course work with multiple disciplines. Dolesnky and Moore, [10] two nursing educators discuss Quality and Safety for Education of Nurses (QSEN); which is nearly a decade old. They indicate the focus is now too narrow and can leave out crucial interactions impacting the system. Therefore, one might venture to say it is linier and reductionist thinking rather than systems thinking.
Interconnected systems thinking?
It is clear how much variability there is in situations. We generally think as a provider we are addressing and handling every issue pertinent to our patient. Yet, when we see what we do from a systems vantage we realize how many variables impact our patients. A systems perspective is connections between the critical concepts for IPE/IPP, TeamSTEPPS®, and broadly communication; which include the digital age. All merge to clarify, communicate, and collaborate as we utilize interoperability with healthcare information. When so doing we can easily see the interconnectedness of the principles of IPE, IPP, Patient Centered Care (Appendix) and the critical nature of systems thinking.
Recommendations
Moving forward curriculums must revise requirements to incorporate the concepts of IPE/IPP, and Team STEPPS to prepare new providers in our healthcare environment. Merging entry level required course work discussing professionalism, history, and background of disciplines, can be accomplished while reducing redundancy of early course work using IPE/TeamSTEPPS® principles. Engaging faculty and students in, as an example, history and professionalism of nursing, pharmacy, and medicine can accomplish socialization to what it means as a profession and in practicing in an interprofessional environment. This methodology can engage students in differences/similarities of scopes of practice and historical similarities with the overarching common goals. To address different schedules between schools and programs virtual reality coursework with interprofessional disciplines should become the norm. This could be used to supplement when several disciplines of students and faculty have conflicting schedules or limited space available to meet face to face. The use of technology can accomplish this readily.
To communicate within 2021 Copyright OAT. All rights reservcritical for all disciplines in the team. Learning and engaging electronically students will understand more readily the necessity of informatics concepts and skills. Board certifications, state licensing, and legislative changes should require informatics scenarios to be infused with exams because of continued increase of digital records and move to digital formats.
Summary
It is clear how much variability there is in many situations. We generally think as a provider we are addressing and handling every issue pertinent to our patient. Yet, when we see what we do from a systems vantage point we realize how much we are missing that can make a tremendous difference in the care we provide to our patients. All of the system, and the unknowns in the system, impact every provider regardless of specialty.
References
- AHRQ (2016) TeamSTEPPS®: Strategies and tools to enhance performance and patient safety. PSNet.
- Whittenberg E, Handzo G, Malloy P, Smith T, Glajchen M (2016) Enhancing palliative care communication through interprofessional education. [Abstract]. Journal of Pain and Symptom Management 52: 336.
- King S, Gredidanus E, Carbonaro M, Drummond J, Boechler P, et al. (2010) Synchronous problem-based e-learning (ePBL) in interprofessional health science education. Journal of Interactive Online Learning 9: 133-150.
- Gehlert KM, Ressler T, Baylon D (2013) Global challenges demand global education of systems thinking. Human Systems Management 32: 79-94.
- Clark K, and Normile L (2012) Nursing informatics and data collection from the electronic medical record: Study of characteristics, factors and occupancy impacting outcomes of critical care admissions from the Emergency Department. Health Informatics Journal 18: 309-319.
- The Free Dictionary by Farlax (n.d.) Terminology. Available from http://medical-dictionary.thefreedictionary.com/terminology
- The Free Dictionary by Farlax (n.d.) Nomenclature. Available from http://medical-dictionary.thefreedictionary.com/nomenclature
- Evanoff B, Potter P, Wolf L, Grayson D, Dunagan C, et al. (2005) Can We Talk? Priorities for Patient Care Differed Among Health Care Providers. Advances in Patient Safety 1. [Crossref]
- Clark K, Brennon-Congdon H, Macmillan K, Gonzales JP, Guerra A (2015) Changes in perceptions and attitudes of healthcare profession student’s pre and post academic course experience of team-based ‘care for the critically ill. Journal of Professional Nursing 31: 330-339.
- Dolansky MA, Moore SM (2013) Quality and Safety Education for Nurses (QSEN): The Key is Systems Thinking. Online J Issues Nurs 18: 1. [Crossref]
- Buring SM, Bhushan A, Broeseker A, Conway S, Duncan-Hewitt W, et al. (2009) Interprofessional education supplement. Interprofessional education: Definitions, student competencies, and guidelines for implementation. American Journal of Pharmaceutical Education 73: 59.
- Clark K (2016) Essential principles for person/patient centered care. PowerPoint Presentation Washington, D. C. USA
- Medicare and Medicaid Health Information Technology (2009) Title IV of the American Recovery and Reinvestment Act Fact Sheet. CMS.com.
- Reese R (2011) Why doctors don’t like electronic health records [Blog]. The Health Care Blog.
- Lusk R (2012) Cloud computing may be a simple solution to your EHR needs. ENT Today.