Abstract
Gallbladder volvulus is a rare condition that typically affects elderly patients who present with a presumed diagnosis of acute cholecystitis. Often preoperative imaging is unable to definitively diagnosis volvulus.A 90 year old female presented with a four day history of abdominal pain and was found to have peritoneal signs on examination. CT scan was obtained concerning for necrosis of the gallbladder. She was taken for emergent laparoscopic cholecystectomy, which was converted to an open procedure upon the realization of volvulus.The patient’s postoperative recovery was uneventful and she was discharged to a nursing facility on postoperative day four.Gallbladder volvulus should be considered in the differential diagnosis of the elderly patient with presumed acute cholecystitis.
Key words
Gallbladder volvulus, elderly, acute abdomen
Introduction
Gallbladder volvulus is a known but rare condition that often presents with acute abdomen in the elderly population. Less than 500 cases have been previously reported and the incidence is unknown. Only a few have reported a preoperative diagnosis of gallbladder volvulus, and imaging remains non-diagnostic. Patients are presumed to have acute cholecystitis in the setting of normal liver function testing. Gallbladder volvulus requires immediate operative intervention to avoid potential complications, while acute cholecystitis usually does not require immediate surgical attention. Though this is a rare condition, it is important to includegallbladder volvulus in the differential diagnosis when evaluating an elderly patient with acute onset of right upper quadrant pain.
Case report
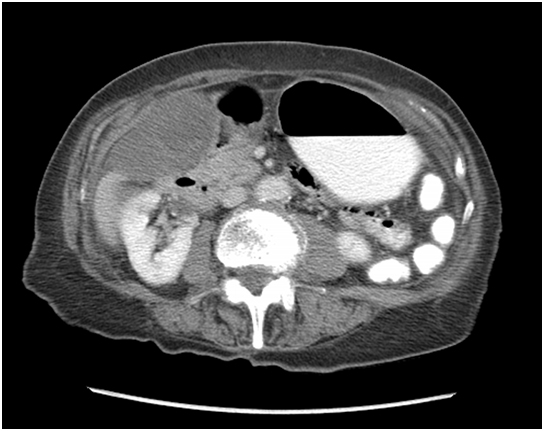
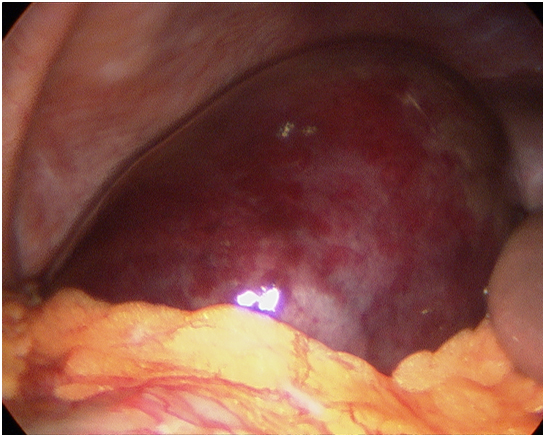
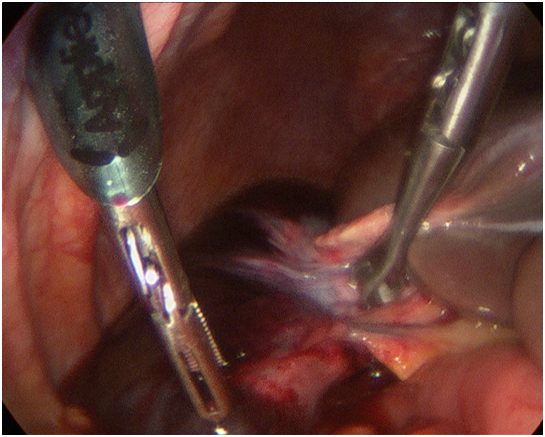
A 90 year old female with no past surgical history presented with four days of abdominal pain, nausea, vomiting and anorexia. She reported no fevers or change in bowel habits. Physical examination revealed an afebrile hemodynamically stable patient. Her abdomen was soft, mildly distended but was extremely tender to palpation at the right upper quadrant region. The tenderness was associated with involuntary guarding. No mass was appreciated. The remainder of her physical exam was within normal limits. Laboratory evaluation revealed a white blood cell count of 14,800 and normal liver function test. CT scan of the abdomen and pelvis revealed a distended and likely necrotic gallbladder without cholelithiasis (Figure 1). This was associated with fat stranding and a significant amount of pericholecystic fluid. The patient was taken to the operating room for laparoscopic cholecystectomy. Upon diagnostic laparoscopy, the patient’s gallbladder was found to be distended, necrotic andvolvulized on its mesentery, along the axis of the cystic duct and cystic artery (Figure 2 & 3). As the anatomy was unclear, the case was converted to an open procedure via a right subcostal incision. The gallbladder was detorsed and the cystic duct and artery were then clearly identified and ligated. The gallbladder was noted to be nonadherent to the liver and was easily resected. The patient’s postoperative course was uneventful and she was discharged to a skilled nursing facility on postoperative day four. Final pathology revealed acute cholecystitis with extensive hemorrhage, focal acute inflammation and loss of surface mucosa. No cholelithiasis was identified.
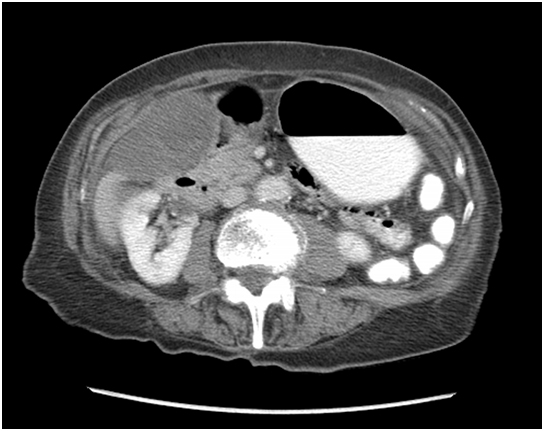
Figure 1: CT scan demonstrating enlarged gall bladder (labelled GB) without stones.
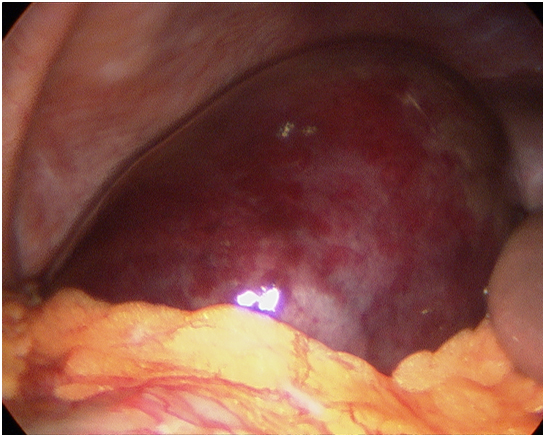
Figure 2: Intraoperative photo of distended and necrotic gall bladder.
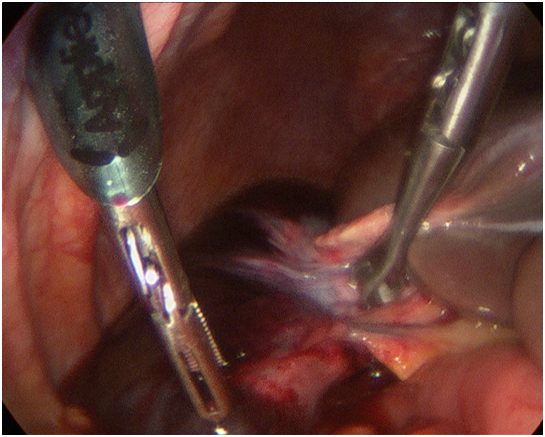
Figure 3: Intraoperative photo of twisted cystic duct pedicle.
Discussion
Acute torsion of the gallbladder is a rare entity in the United States. Initially reported by Wendel in 1898[1], this phenomenon has been described by several authors internationally and seems to have become more common in the past decade.
This condition often occurs in elderly, thin females, who present with acute abdomen and signs suggestive of acute cholecystitis, specifically right upper quadrant pain without jaundice. A spectrum of abdominal exam findings has been described. Findings have included mild right upper quadrant pain, palpation of a mass, frank peritonitis[2,3], or suspected acute appendicitis[4,5]. On laboratory evaluation, these patients do not exhibit signs ofbiliary obstruction or elevation of liver function tests. However, leukocytosis may be present, indicating an inflammatory response. Our patient presented with this clinical picture, including peritoneal signs on exam and no signs of biliary obstruction on laboratory evaluation.
Table 1 summarizes all of the reported cases in the English literature since the advent of laparoscopic cholecystectomy by Enrich Muhe[6]. As described above, most of thesepatients are elderly female patients who presented with RUQ pain without a palpable abdominal mass. In most cases, the initial diagnosis was acute or acalculouscholecystitis. However, seven out of 45 cases were diagnosed as gallbladder volvulus preoperatively. Interestingly, a majority of these cases were diagnosed on CT scan, which is not the traditional imaging modality for gallbladder pathology. In hind-sight, our patient’s torsion was visible on CT scan. Unlike our patient, most of the patients who presented with gallbladder volvulus did not have peritonitis or an acute abdomen. They therefore underwent further workup with hepatobiliary iminodiacetic acid (HIDA) scan, magnetic resonance imaging (MRI), or magnetic resonance cholangiopancreatography (MRCP), which revealed findings of a volvulized gallbladder.
| |
Author, year |
N |
Age |
Sex |
Signs & Symptoms |
Peritonitis |
Attempted Methods of Diagnosis |
Suspected preopdiagnosis |
Method of Diagnosis |
Lap
v
Open |
Outcome |
1 |
McHenrey [7] |
2 |
87 |
F |
epigastric pain |
no |
AXR, US |
AC |
exploration |
open |
uncomplicated |
| |
|
|
80 |
F |
generalized abdominal pain |
no |
AXR |
partial large bowel obstruction |
exploration |
open |
uncomplicated |
2 |
Van der Veken[8] |
1 |
83 |
F |
RLQ pain |
no |
AXR |
acute appendicitis |
exploration |
open |
uncomplicated |
| |
|
|
|
|
|
|
|
|
|
|
|
3 |
Alden[9] |
2 |
78 |
F |
RUQ pain |
no |
US |
AC |
exploration |
open |
uncomplicated |
| |
|
1 |
91 |
F |
chest and abdominal pain |
no |
US |
AC |
exploration |
open |
uncomplicated |
4 |
Macdonald [10] |
1 |
74 |
M |
RUQ pain and abdominal mass |
no |
none |
AC |
exploration |
open |
uncomplicated |
5 |
Gonzalez-Fisher [11] |
1 |
56 |
F |
RUQ pain |
no |
US |
AC |
exploration |
open |
uncomplicated |
6 |
Nguyen [12] |
1 |
91 |
F |
crampy abdominal pain |
no |
AXR, US, CT, |
AC |
exploration |
laparoscopy |
uncomplicated |
7 |
Schroder [13] |
1 |
18 |
F |
|
|
|
|
exploration |
laparoscopy |
|
8 |
Hamdi [14] |
1 |
90 |
F |
RUQ pain |
no |
AXR, US |
AC |
exploration |
open |
uncomplicated |
9 |
McAleese [15] |
1 |
85 |
F |
RUQ pain |
no |
US |
AC |
exploration |
laparoscopy |
postoperative bleeding diverticuli requiring redadmission |
10 |
Christoudias [16] |
1 |
82 |
F |
left chest pain |
no |
US |
AC |
exploration |
laparoscopy |
uncomplicated |
11 |
Losken [17] |
1 |
80 |
F |
epigastric pain |
no |
AXR |
bowel obstruction |
AC |
open |
uncomplicated |
12 |
Ikematsu [18] |
6 |
77-91 |
F |
|
|
|
|
|
|
|
13 |
Khosraviani [19] |
1 |
86 |
F |
RUQ pain and abdominal mass |
no |
US |
AC |
exploration |
not commented |
uncomplicated |
14 |
Usui [20] |
1 |
78 |
F |
epigastric pain |
no |
CT, US, MRI, MRCP, |
GBV |
MRCP |
open |
uncomplicated |
15 |
Rajagopal [21] |
1 |
70 |
F |
RUQ pain and abdominal mass |
no |
US, CT |
AC |
exploration |
open |
uncomplicated |
16 |
Kim [22] |
1 |
73 |
F |
n/a |
n/a |
n/a |
n/a |
n/a |
n/a |
n/a |
17 |
Ortiz-Gonzalez [23] |
1 |
90 |
F |
RUQ pain |
yes |
AXR |
acute appendicitis |
exploration |
open |
uncomplicated |
18 |
Cho [24] |
1 |
94 |
F |
RLQ pain and abdominal mass |
no |
CT |
GBV |
CT |
laparoscopy |
uncomplicated |
19 |
Shaikh [25] |
2 |
79 |
M |
RUQ pain |
no |
US, CT |
hydrops of GB |
exploration |
open |
uncomplicated |
| |
|
|
84 |
M |
RUQ pain |
no |
US |
AC |
exploration |
laparoscopy |
uncomplicated |
20 |
Matsuhashi [26] |
1 |
54 |
F |
RUQ pain |
no |
US, CT, MRI, MRCP |
necrotic gall bladder |
exploration |
open |
uncomplicated |
21 |
Tarhan [27] |
1 |
70 |
M |
RUQ pain |
no |
AXR, US |
AC |
exploration |
open |
wound infection |
22 |
Faure [28] |
1 |
84 |
F |
RUQ pain and abdominal mass |
no |
US, CT |
GBV |
CT |
laparosocpy |
uncomplicated |
23 |
Kimura [29] |
1 |
11 |
M |
RUQ pain |
no |
US, CT, MRI |
GBV |
MRI |
laparoscopy |
uncomplicated |
24 |
Malherbe [30] |
2 |
86 |
F |
RUQ pain |
no |
US, CT, EUS |
AC |
exploration |
open |
uncomplicated |
| |
|
|
80 |
F |
diffuse abdominal pain w palpable mass |
no |
CT |
AC |
exploration |
laparoscopy |
postoperative pleural effusions |
25 |
Caliskan [31] |
1 |
79 |
F |
RUQ pain and abdominal mass |
no |
US |
acalculouscholecystitis |
exploration |
open |
uncomplicated |
26 |
Lavy [32] |
1 |
85 |
F |
RUQ pain |
yes |
CT |
GBV |
CT |
not commented |
uncomplicated |
27 |
Bagnato [33] |
1 |
85 |
M |
RUQ pain |
yes |
AXR, US |
acalculouscholecystitic |
exploration |
open |
uncomplicated |
28 |
Chen [34] |
1 |
84 |
F |
RUQ pain |
no |
AXR, CT, |
AC |
exploration |
open |
uncomplicated |
29 |
Chittal [35] |
1 |
71 |
F |
cecal volvulus |
|
|
|
exploration |
|
|
30 |
Inoue [36] |
1 |
95 |
M |
abdominal pain |
no |
CT, US, MRI, MRCP, |
GBV |
CT, MR |
laparoscopy |
uncomplicated |
31 |
Mouawad [37] |
1 |
99 |
F |
RUQ pain |
no |
CT, HIDA, ERCP |
AC |
exploration |
open |
uncomplicated |
32 |
Alevizos [38] |
1 |
95 |
F |
RUQ pain and abdominal mass |
no |
CT |
n/a |
exploration |
laparoscopy |
uncomplicated |
33 |
Arslan [39] |
1 |
47 |
M |
RUQ pain |
yes |
US |
AC |
exploration |
open |
uncomplicated |
34 |
Miyakura [40] |
1 |
61 |
F |
RUQ pain |
no |
US, CT |
GBV |
CT |
laparoscopy |
uncomplicated |
Table 1: Gall bladder volvulus case reports since advent of laparoscopic cholecystectomy in 1986.
Key: AC = acute cholecystitis; AXR = abdominal x-ray; CT = computed tomography; ERCP = endoscopic retrograde cholangiopancreatography; GBV = gall bladder volvulus; HIDA = hepatobiliary iminodiacetic acid scan; MRCP = magnetic resonance cholangiopancreatography; MRI = magnetic resonance imaging; US = ultrasound
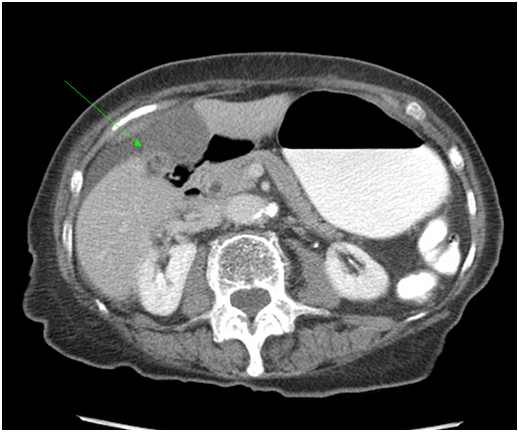
From a clinical standpoint, gallbladder volvulus can show up on imaging as a distended, hydropic gallbladder with thickened wall and pericholecystic fluid. It has been previously suggested that ultrasound may be the instrumental for the diagnosis, with a triad of radiologic findings including: anterior localization of the gallbladder; increased volume of the gallbladder; and a severely thickened, multilayered gallbladder wall[14]. Our patient’s physical exam prompted evaluation in the emergency department with a CT scan. Chen et al. suggested that gallbladder volvulus can be identified on the CT scan using the “U to 9 to O” sign[34]; however, this sign was not evident on our patient’s imaging. Upon retrospective review of our patient’s CT scan, one can appreciate a twist of the gallbladder along the axis of the cystic duct (Figure 4). The use of MRCP to diagnose gallbladder volvulus has been reported [20,26]. However, the majority of these patients present with an acute abdomen, requiring prompt surgical intervention, thus negating any additional studies;a result, only 1% of reported cases of gallbladder volvulus werediagnosed preoperatively[41].
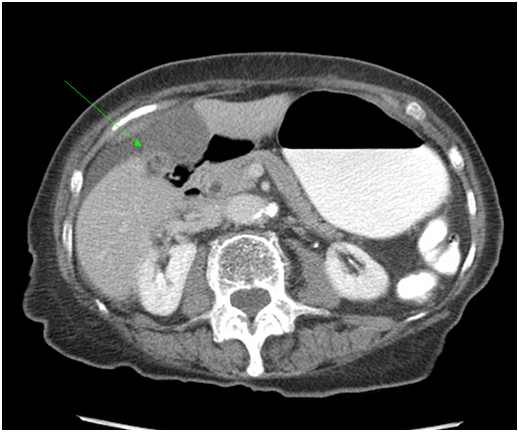
Figure 4: Twisted cystic duct pedicle on CT scan.
Conclusion
The exact cause of gallbladder volvulus remains unknown. Suggested mechanisms for torsion include: congenital deformities, a long peritoneal mesentery, generalized visceroptosis, forceful peristalsis of nearby organs, cholelithiasis, or atherosclerosis of the cystic artery[10,18]. The acute torsion initially results in venous congestion of the gallbladder, leading to engorgement of the organ, followed by acute internal hemorrhage as the mucosa becomes necrotic. This clinical entity has been described sporadically in the literature and remains a rare or under-reported phenomenon. While this diagnosis has been made radiographically, the use of imaging is difficult in cases where patients present with peritonitis requiring emergent operation.
The gallbladder in a gallbladder volvulus case can be resected laparoscopically; however, the triangle of Calot may be difficult to be identified due to torsion of the gallbladder along the cystic duct axis. Therefore, laparotomy may be necessary in order to safely evaluate the anatomy prior to its resection. To summarize, although rare, it is important to consider gallbladder volvulus as a differential diagnosis in the elderly patient with right upper quadrant pain and peritonitis, especially if the clinical situation does not permit time for additional radiographic studies.
Conflict of interest
Anuradha R. Bhama, MD and other co-authors have no conflict of interest.
References
- Wendel AV (1898) VI. A Case of Floating Gall-Bladder and Kidney complicated by Cholelithiasis, with Perforation of the Gall-Bladder. Ann Surg 27: 199-202. [Crossref]
- Ortiz-Gonzälez J1, Reyes-Segura MP, Gutierrez-Carrillo F, Vega-Chavaje RG (2003) Volvulus of the gallbladder. Dig Dis Sci 48: 1116-1117. [Crossref]
- Bagnato C, Lippolis P, Zocco G, Galatioto C, Seccia M (2011) Uncommon cause of acute abdomen: volvulus of gallbladder with necrosis. Case report and review of literature. Ann Ital Chir82: 137-140. [Crossref]
- Alevizos L, Stamou KM, Tsamis D, Pattas M, Menenakos E, et al. (2012) Gallbladder volvulus as a cause of an acute abdomen in a 95-year-old patient. Am Surg 78: E47-48. [Crossref]
- Rueda-Martínez JL C-SP, Vázquez-Aragón P, Valero-Liñán AS, Prat-Calero A (2012) Gallbladder volvulus: clinical presentation mimicking acute appendicitis of the elderly. Rev EspEnferm Dig 103:656-657. [Crossref]
- Mühe E (1991) [Laparoscopic cholecystectomy]. Z GastroenterolVerh 26: 204-206. [Crossref]
- McHenry CR, Byrne MP (1986) Gallbladder volvulus in the elderly. An emergent surgical disease. J Am GeriatrSoc 34: 137-139. [Crossref]
- Van der Veken E, Azagra JS, de Prez C (1986) Gallbladder volvulus: a case report. ActaChirBelg 86: 267-269. [Crossref]
- Alden PB, Miller JB, Gamble WG (1989) Volvulus of the gallbladder. Report of two cases and review of the literature. Minn Med 72: 653-656. [Crossref]
- Macdonald PH1, Pace RF (1990) Volvulus of the gallbladder: a case report. Can J Surg 33: 282-283. [Crossref]
- Gonzalez-Fisher RF1, Vargas-Ramirez L, Rescala-Baca E, Dergal-Badue E (1993) Gallbladder volvulus. HPB Surg 7: 147-148. [Crossref]
- Nguyen T1, Geraci A, Bauer JJ (1995) Laparoscopic cholecystectomy for gallbladder volvulus. SurgEndosc 9: 519-521. [Crossref]
- Schroder DM1, Cusumano DA 3rd (1995) Laparoscopic cholecystectomy for gallbladder torsion. SurgLaparoscEndosc 5: 330-334. [Crossref]
- Hamdi M1, Blondiau JV, Algaba R, Van Gysel JP (1996) Gallbladder volvulus: a case report. Could the ultrasound be the key of the early diagnosis? ActaChirBelg 96: 41-43. [Crossref]
- McAleese P1, Kolachalam R, Zoghlin G (1996) Saint's triade presenting as volvulus of the gallbladder. J LaparoendoscSurg 6: 421-425. [Crossref]
- Christoudias GC (1997) Gallbladder volvulus with gangrene. Case report and review of the literature. JSLS 1: 167-170. [Crossref]
- Losken A1, Wilson BW, Sherman R (1997) Torsion of the gallbladder: a case report and review of the literature. Am Surg 63: 975-978. [Crossref]
- Ikematsu Y1, Yamanouchi K, Nishiwaki Y, Kida H, Waki S, et al. (2000) Gallbladder volvulus: experience of six consecutive cases at an institute. J Hepatobiliary PancreatSurg 7: 606-609.[Crossref]
- Khosraviani K1, Tho2021 Copyright OAT. All rights reservf the gallbladder. Ulster Med J 69: 163-164. [Crossref]
- Usui M, Matsuda S, Suzuki H, Ogura Y (2000) Preoperative diagnosis of gallbladder torsion by magnetic resonance cholangiopancreatography. Scand J Gastroenterol 35:218-222. [Crossref]
- Rajagopal R1, Rajagopal A (2001) Acute torsion of the gall bladder. Am J Surg 182: 534-535. [Crossref]
- Kim SY1, Moore JT (2003) Volvulus of the gallbladder: laparoscopic detorsion and removal. SurgEndosc 17: 1849. [Crossref]
- Ortiz-Gonzälez J1, Reyes-Segura MP, Gutierrez-Carrillo F, Vega-Chavaje RG (2003) Volvulus of the gallbladder. Dig Dis Sci 48: 1116-1117. [Crossref]
- Cho YP1, Kim HJ, Jung SM, Kang GH, Han MS, et al. (2005) Torsion of the gallbladder: report of a case. Yonsei Med J 46: 862-865. [Crossref]
- Shaikh AA1, Charles A, Domingo S, Schaub G (2005) Gallbladder volvulus: report of two original cases and review of the literature. Am Surg 71: 87-89. [Crossref]
- Matsuhashi N, Satake S, Yawata K, Asakawa E, Mizoguchi T, Kanematsu M, et al. (2006) Volvulus of the gall bladder diagnosed by ultrasonography, computed tomography, coronal magnetic resonance imaging and magnetic resonance cholangio-pancreatography. World J Gastroenterol 12:4599-4601. [Crossref]
- Tarhan OR1, Barut I, Dinelek H (2006) Gallbladder volvulus: review of the literature and report of a case. Turk J Gastroenterol 17: 209-211. [Crossref]
- Faure JP1, Doucet C, Scepi M, Rigoard P, Carretier M, et al. (2008) Abnormalities of the gallbladder, clinical effects. SurgRadiolAnat 30: 285-290. [Crossref]
- Kimura T1, Yonekura T, Yamauchi K, Kosumi T, Sasaki T, et al. (2008) Laparoscopic treatment of gallbladder volvulus: a pediatric case report and literature review. J LaparoendoscAdvSurg Tech A 18: 330-334. [Crossref]
- Malherbe V1, Dandrifosse AC, Detrembleur N, Denoel A (2008) Torsion of the gallbladder: two case reports. ActaChirBelg 108: 130-132. [Crossref]
- Caliskan K1, Parlakgumus A, Koc Z, Nursal TZ (2009) Acute torsion of the gallbladder: a case report. Cases J 2: 6641. [Crossref]
- Lavy M, Lubrano J, Morati P, Delabrousse E, Idelcadi O, et al. (2010) Gallbladder volvulus diagnosed at computed tomography. Am Surg 76: 1302-1303. [Crossref]
- Bagnato C1, Lippolis P, Zocco G, Galatioto C, Seccia M (2011) Uncommon cause of acute abdomen: volvulus of gallbladder with necrosis. Case report and review of literature. Ann Ital Chir 82: 137-140. [Crossref]
- Chen Y1, Rosati C (2011) Necrotizing volvulus of the gallbladder with a distinct pattern on computed tomography scan. Am Surg77: E298-300. [Crossref]
- Chittal R1, Harris D, Patel A, Goodyear S, Parkianathan V (2011) An interesting rare case of double volvulus. BMJ Case Rep 2011. [Crossref]
- Inoue S1, Odaka A, Hashimoto D, Tamura M, Osada H (2011) Gallbladder volvulus in a child with mild clinical presentation. PediatrRadiol41: 113-116. [Crossref]
- Mouawad NJ1, Crofts B, Streu R, Desrochers R, Kimball BC (2011) Acute gallbladder torsion - a continued pre-operative diagnostic dilemma. World J EmergSurg6: 13. [Crossref]
- Alevizos L1, Stamou KM, Tsamis D, Pattas M, Menenakos E, et al. (2012) Gallbladder volvulus as a cause of an acute abdomen in a 95-year-old patient. Am Surg 78: E47-48. [Crossref]
- Arslan ED1, Hakbilir O, Uyanik B, Oztürk B, Kaya E, et al. (2012) Gallbladder volvulus. J Pak Med Assoc62: 965-966. [Crossref]
- Miyakura Y1, Sadatomo A, Ohta M, Lefor AT, Sata N, et al. (2012) Floating gallbladder strangulation caused by the lesser omentum: report of a case. Surg Today 42: 693-696. [Crossref]
- Katz DS, Yam B, Hines JJ, Mazzie JP, Lane MJ, et al. (2008) Uncommon and unusual gastrointestinal causes of the acute abdomen: computed tomographic diagnosis. Semin Ultrasound CT MR29:386-398. [Crossref]