Abstract
The Spigelian hernia was first coined by Joseph Klinkosch in the 18th century and takes its name from anatomist Adrian van der Spigel who first described the linea semilunaris in the 17th century. It is generally uncommon and often non-specific in presentation, requiring abdominal imaging for confirmation of diagnosis. We present a rare case of bilateral Spigelian hernias with unilateral incarceration causing intestinal obstruction, which was chiefly diagnosed via computed tomography imaging. The patient underwent successful exploratory laparotomy and onlay mesh repair of bilateral Spigelian hernias. While laparoscopic repair of Spigelian hernia continues to grow in popularity, open repair remains safe, feasible and even preferrable in cases presenting with incarceration and intestinal obstruction, as well as those with large hernial defects requiring concomitant abdominal wall repair.
Keywords
Hernia, Abdominal wall repair, Anaesthesia.
Introduction
The Spigelian hernia was first coined by Joseph Klinkosch in the 18th century and takes its name from anatomist Adrian van der Spigel who first described the linea semilunaris in the 17th century [1]. It describes a hernia occurring through the Spigelian fascia, which is comprised of the internal oblique and transversus abdominis aponeuroses, located at the linea semilunaris just lateral to the rectus abdominis muscle. It often occurs at or just inferior to the arcuate line, where the posterior rectus sheath ends. Accounting for only 2% of all abdominal hernias, it is often non-specific in presentation and continues to represent a diagnostic and operative challenge [2- 4]. This is often compounded in the presence of bilateral defects, which are exceedingly uncommon and only represent 3% of patients with Spigelian hernia. We present a rare case of bilateral Spigelian hernias with unilateral incarceration causing intestinal obstruction, which was diagnosed on abdominal imaging and managed surgically.
Case Presentation
An elderly lady in her 80s presented to the Emergency Department with intermittent abdominal pain of a few months’ duration, which had worsened over the preceding few days. This was associated with intermittent nausea, vomiting, diarrhoea and fever. She had significant medical co-morbidities including hypertension, beta-thalassaemia trait, osteoporosis, chronic subdural haemorrhage, and possible cognitive impairment. She required assistance with her activities of daily living, and had to rely on a rollator frame for ambulation. She did not have a history of previous abdominal surgeries. Her BMI was 16.7.
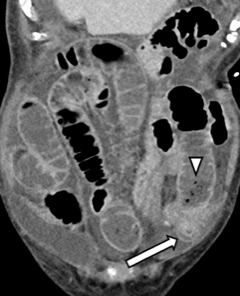
On review, the patient was noted to have stable vital signs. Initial physical examination revealed a soft and non-tender abdomen without any obvious masses or abnormalities, while bedside ultrasound examination showed the presence of intra-abdominal free fluid. Her preliminary blood results including inflammatory markers and arterial blood gas were unremarkable. Computed tomography (CT) scan of her abdomen and pelvis then revealed significant ascites along with bilateral Spigelian hernias – while the right-sided hernia sac was fluid-filled, the left-sided hernia sac contained an incarcerated loop of oedematous small bowel with collapsed bowels distal to it (Figures 1 and 2).

Figure 1: Axial contrast-enhanced CT image shows bilateral Spigelian hernias. The right-sided hernia contains ascites (arrowhead), while the left-sided hernia contains a knuckle of small bowel (arrow).
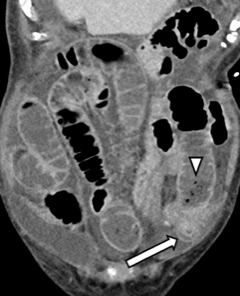
Figure 2: Coronal contrast-enhanced CT image shows submucosal oedema involving the herniated small bowel segment (arrow), together with diffuse upstream dilatation. Note is made of “small bowel faeces” sign (arrowhead). The contralateral Spigelian hernia is also appreciated.
Treatment
An exploratory laparotomy via a lower midline incision was promptly performed under general anaesthesia. Intra-operatively, the incarcerated left-sided Spigelian hernia sac was reduced and found to contain healthy small bowel loops, thus no bowel resection was necessary. The left-sided Spigelian fascial defect was noted to be 2cm in diameter, while the right-sided fascial defect measured 3cm and did not contain any trapped bowels. The bilateral Spigelian hernial defects were repaired from the peritoneal side using simple interrupted polydioxanone (PDS) sutures, ensuring full thickness closure of all layers including the internal oblique and transversus abdominis aponeurosis. Separate transverse left and right iliac fossa incisions were then made to place Prolene onlay meshes to reinforce the anterior abdominal fascia. Being mindful of the patient’s frailty and significant medical co-morbidities, this open approach was selected to achieve a durable hernia repair while minimising any unnecessary prolongation in operative duration. Almost 2L of clear ascitic fluid was also drained.
Post-operatively, the patient endured an initial period of post-operative ileus along with hospital-acquired pneumonia and hypoactive delirium. She gradually recovered with supportive management and tolerated slow escalation of feeding. Her ascites was attributed to hypoalbuminaemia for which she later required drainage by interventional radiologists and intravenous albumin replacement. The patient was eventually discharged after 3 weeks of hospitalisation.
The patient was last reviewed 3 months post-op in the outpatient clinic. It was noted that she had returned to her pre-morbid functional status without any signs of wound complications, recurrent abdominal wall hernia or intestinal obstruction. She was given an open date follow-up thereafter.
Discussion
Spigelian hernias make up just 2% of all abdominal wall hernias, while bilateral disease is even more uncommon. Among 624 patients included in a systematic review by Mayank et al, only 19 (3.1%) of them had bilateral Spigelian hernias [3]. Females have been described to develop Spigelian hernias more frequently, while other risk factors include obesity, multiple pregnancies, chronic cough and straining [2,4,5]. Presentation is often non-specific with intermittent abdominal pain, with or without a palpable abdominal wall lump at the linea semilunaris. While some cases may be noted as incidental Spigelian fascial defects during general laparoscopic procedures [6], almost 20% may present with hernia incarceration requiring emergency surgery. Abdominal imaging including ultrasonography and CT scans are usually obtained in cases of uncertain diagnosis [4].
In the systematic review by Mayank et al., the authors noted a growing trend towards laparoscopic repair compared to the traditional open onlay mesh repair over the last few decades [3]. The most popular laparoscopic approaches were the intraperitoneal onlay mesh (IPOM), transabdominal preperitoneal (TAPP) and totally extraperitoneal (TEP) repair techniques, and they have been associated with reduced post-operative morbidity and length of hospitalisation compared to open surgery [7]. However, open surgery enables concurrent abdominal wall repair for patients with large Spigelian hernias and can be performed under locoregional anaesthesia for patients at high risk of general anaesthetic complications [4]. Open surgery may also be the only option in cases presenting emergently with incarceration and intestinal obstruction, where the presence of dilated bowel loops could make laparoscopic surgery challenging and unfeasible.
There have been a few cases of bilateral Spigelian hernias reported in the literature. Safioleas et al. described a case of successful bilateral open hernioplasty for bilateral Spigelian hernias [8], while Vannahme et al. presented a case of laparoscopic converted to open mesh repair of an incarcerated right-sided Spigelian hernia in a patient with bilateral Spigelian hernias [9]. Matsui et al. also described a rare case of concurrent TEP repair for bilateral Spigelian and right-sided inguinal hernias [10]. No immediate post-operative complications were encountered in these case reports, indicating that both open and laparoscopic repair remain feasible in the setting of bilateral Spigelian hernias.
In our case, the patient had multiple medical co-morbidities and displayed radiological features of left-sided small bowel incarceration and obstruction. Open surgery was the logical option as it was a priority to avoid unnecessary prolongation of operative time given the patient’s frailty and co-morbidities, and the presence of dilated small bowel loops and significant ascites would have increased the complexity of a laparoscopic approach. The bilateral hernia defects were reasonably small at 2-3cm in size, which made open onlay mesh repair a convenient and feasible option. The patient did not suffer any immediate post-operative complications such as hernia recurrence, wound infection, post-operative haematoma or collection.
Conclusion
Spigelian hernias continue to pose a surgical conundrum owing it its rarity, non-specific presentation, and difficulty with clinical detection on physical examination, thus often requiring abdominal imaging for accurate diagnosis. Despite bilateral Spigelian hernias being even more uncommon, there is emerging evidence in the literature demonstrating that both open and laparoscopic repair techniques are feasible surgical approaches. Open onlay mesh repair of bilateral Spigelian hernias is certainly a viable and safe option for selected patients.
References
- Ghosh SK, Sharma S, Biswas S, Chakraborty S (2014) Adriaan van den Spiegel (1578-1625): Anatomist, physician, and botanist. Clin Anat 27: 952-957.
- Skandalakis PN, Zoras O, Skandalakis JE, Mirilas P (2006) Spigelian Hernia: Surgical Anatomy, Embryology, and Technique of Repair. Am Surg 72: 42-48. [Crossref]
- Roy M, Balarajah V, Mudan SA (2021) Systematic Review of the Evolution of Surgical Technique for Spigelian Hernia. Indian J Surg 83: 850-858.
- Hanzalova I, Schäfer M, Demartines N, Clerc D (2021) Spigelian hernia: current approaches to surgical treatment – a review. Hernia 26: 1427-1433. [Crossref]
- Webber V, Low C, Skipworth RJE, Kumar S, de Beaux AC, et al. (2017) Contemporary thoughts on the management of Spigelian hernia. Hernia 21: 355-361 [Crossref]
- Paajanen H, Ojala S, Virkkunen A (2006) Incidence of occult inguinal and spigelian hernias during laparoscopy of other reasons. Surgery 140: 9-12. [Crossref]
- Moreno-Egea A, Carrasco L, Girela E, Martín J, Aguayo JL, et al. (2002)Open vs Laparoscopic Repair of Spigelian Hernia: A Prospective Randomized Trial. Arch Surg 137: 1266-1268. [Crossref]
- Safioleas M, Stamatakos M, Moulakakis K, Safioleas P, Skandalakis P (2007) Spigelian hernia. A rare case of bilateral hernia and presentation of our experience. Chirurgia (Bucur) 102: 429-432. [Crossref]
- Vannahme M, Monkhouse SJW (2013) Acute management of a unilateral incarcerated Spigelian hernia in a patient with bilateral Spigelian hernias. Ann R Coll Surg Engl 95: 89-91. [Crossref]
- Matsui S, Nitori N, Kato A, Ikeda Y, Kiatagwa Y, et al. (2016) Laparoscopic totally extra-peritoneal hernia repair for bilateral Spigelian hernias and coincident inguinal hernia: A case report. Int J Surg Case Rep 28: 169-172. [Crossref]