Abstract
Introduction: Autologous fat grafting is currently a common adjunct procedure in various reconstructive cases. Muscle tissue, as a recipient site, most of the times ensures optimal fat graft survival rates, due to increased vascular supply.
Materials and Methods: A review was conducted in the US National Library of Medicine by two independent reviewers using the keywords ‘fat graft survival’ OR ‘fat transplantation’ OR ‘lipotransfer’ AND ‘muscle’. All articles published within the last four decades were included. Relevant articles were also found through the reference list of the searched articles.
Results: A total of eleven articles were included in our review. Data that were included in our review were the survival rate of fat cells that were transplanted into muscles, factors that interfered with fat graft survival, as well as the safety of the procedure and the complication rate. The majority of studies confirmed the superiority of muscle tissue in the survival of transplanted fat. However, recent data report a high incidence of fatal complications during fat injections intramuscularly in specific sites, namely the gluteal area.
Conclusion: Fat graft low integration rates can be associated with the recipient site as well as with the total volume injected and the technique used. Intramuscular fat injections favour fat integration but relates to high incidence of major complications.
Keywords
fat graft survival, muscle
Introduction
Autologous fat is widely used in reconstructive and aesthetic surgery as a natural filler in replacing and filling volume deficits [1]. It is a metabolically active tissue consisting of a heterogeneous cell population secreting cytokines, hormones, and growth factors, which promotes healing and tissue regeneration [2].
The type of tissue into which the fat is implanted plays an important role in the overall survival of the fat grafts [3]. Muscle tissue, which is one of the most vascular tissues in the body, was considered from the beginning as one of the most ideal tissues for receiving fat.
Fat grafting in muscle tissue has fallen into disfavor during the last decades. Multiple reports on mortality from gluteal fat grafting suggest that intramuscular fat injection may cause a direct hit to vessels or interfere with the creation of a passive emboli, which could lead to fat embolization [4].
Interestingly there are no published studies describing complications from fat grafting to non-gluteal muscles. Moreover, numerous published articles favour fat graft survival in muscles compared to other tissues [5,6].
The aim of the present review was to give an overview of autologous fat grafting to muscle with emphasis on the efficacy, safety, and complications.
Methods
A review was conducted in the US National Library of Medicine (MEDLINE/Pubmed) by two independent reviewers using the keywords ‘fat graft survival’ OR ‘fat transplantation’ OR ‘lipotransfer’ AND ‘muscle’. All articles published within the last four decades were included. Relevant articles were also found through the reference list of the searched articles.
The inclusion criteria consisted of randomized controlled studies, clinical and experimental case series and case reports that describe fat grafting in muscles. Citations found through the literature search and reference screening were title and/or abstract reviewed for eligibility.
Data that were included in our review were the survival rate of fat cells that were transplanted into muscles, factors that interfered with fat graft survival, safety and complications.
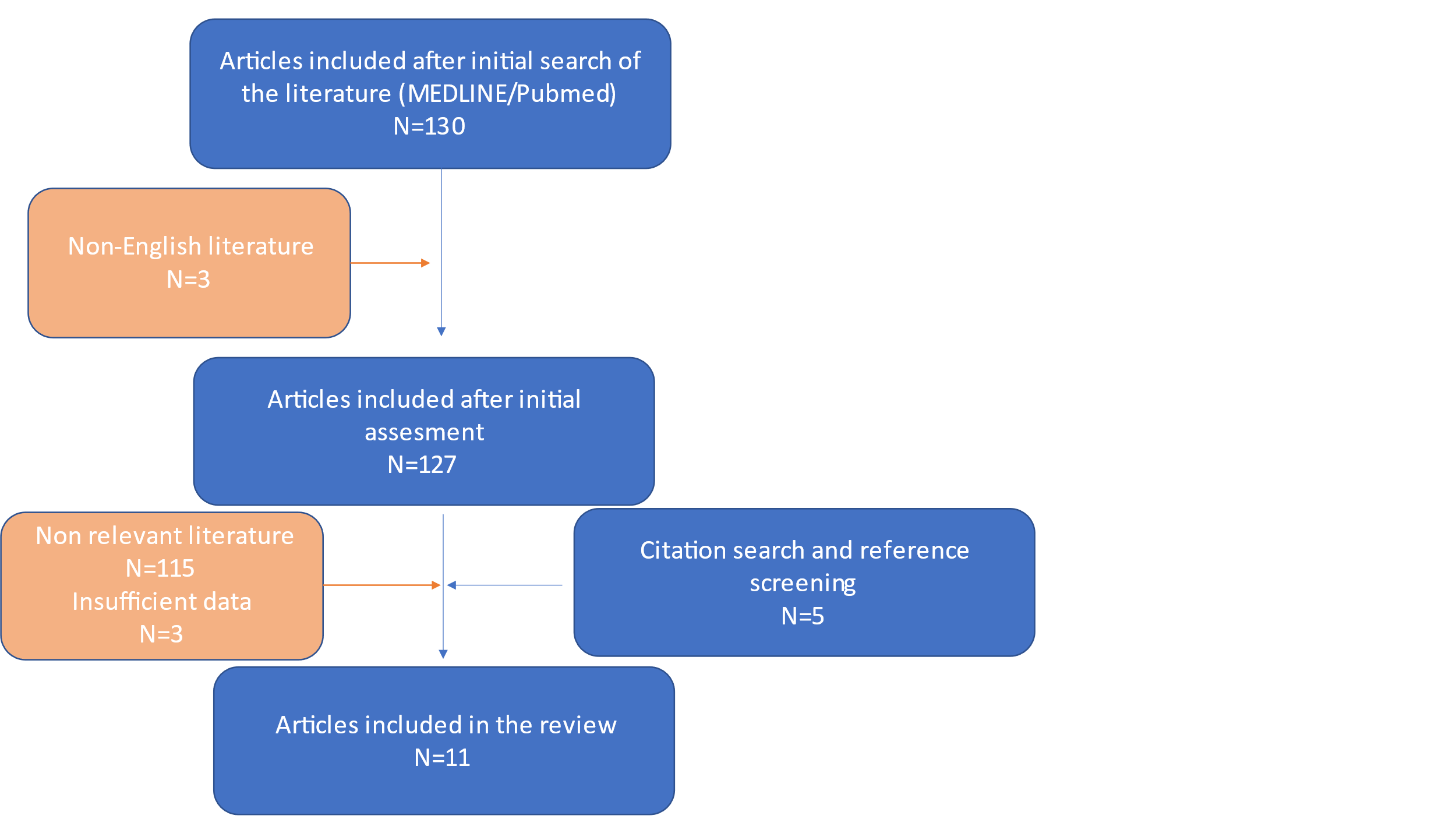
Extracted data were summarized descriptively. A flow chart of our analysis is depicted below. Meta-analysis was not performed due to the heterogeneous methodology among the articles.
Results
Literature search using the keywords mentioned above revealed 130 articles. All articles that were published using a non-English language were excluded from our review (N=3). Studies originating from the reference list that were added were 127. 115 articles were excluded after review of their abstracts, resulting in a total of 12 articles eligible for full-text reading. Out of these articles, 3 articles were excluded for insufficient data. Citation search and reference screening added 5 articles on our review. Ultimately, 11 articles were included into the systematic review. Seven articles were evaluated with a level of evidence III, three with level IV, and one with level V.
Fat graft survival rate
Guerrerosantos et al, were among the first to study the survival of fat autografts in experimental animals [5]. In a comparative experimental study in rats, they reported increased viability of autologous fat grafts after intramuscular injection, compared to subcutaneous injection of an equivalent amount of fat, and after 12 months of follow-up. The favourable results of this experimental study led the authors to a clinical application of intramuscular injection of autologous fat in the gluteal muscles with similar results [5].
The same conclusion was reached by Peren et al, who clinically transferred free fat grafts in 10mm strips at different levels within the gluteal muscle and found that after 5 years of follow-up the survival rates exceeded 60-70% [7].
In their experimental study, Aygit et al [8], published autologous fat survival rates after intramuscular transplantation greater than 50%. All animals were evaluated by scintigraphic imaging and histopathological examination.
Karacaoglu et al [6], in their study compared the survival of autologous fat volume transplanted at different levels, i.e., subcutaneous, above muscle and submuscular in the facial region in rabbits. The results of the study showed statistically significant survival rates of fat cells (p<0.01), in the epimuscular injection (81.95% ± 4.40%) compared to the subcutaneous injection (41.62% ± 3.2%) and submuscular (37.31% ± 5.77%), which was related to the increased perfusion of the recipient area.
Experimental study by Shi et al [9], who compared the survival rates of subcutaneously and intramuscularly injected fat in rats, showed that the fat survived favourably in the subcutaneous layer, although the initial survival rate was higher in the intramuscular area. One of the possible causes of this observation, as interpreted by the authors, is the site of fat injection, involving the locomotor muscles of the lower limbs, which probably negatively affects the overall survival of adipocytes.
Similarly, Nguyen et al [10], in their study, showed excellent survival rates of autologous fat in the muscle tissue for the first month, which however progressively decreased within the first 4 months.
Factors interfering with fat graft survival
One parameter that appears to have a negative effect on the ultimate survival of fat when injected into muscle tissue is muscle contractility, as described in several studies [11-13]. The theory behind this observation is based on the immaturity of the vascular connections that have been developed between the fat graft and the substrate. The shear forces that develop during muscle contraction on the newly formed vascular pedicles may harm the vascular connections and cause devascularization of the fat with the result being a dramatic decrease in fat survival. In addition, these same mechanical forces may negatively affect the degree of differentiation and proliferation of stem cells derived from adipose tissue, and therefore their final conversion into adipocytes. Comparative studies on the effect of immobilization or chemical paralysis of muscles with toxins on the overall survival of the fat yield encouraging results [12,13].
Insufficient vascularization, inflammatory response to the grafted fat, and cellular damage due to mechanical stresses has been associated with fat resorption [14]. Another factor is the intra-tissular pressure. Much as in the phenomenon of compartment syndrome, it can be speculated that the increase in tissue pressure by the injected volume may lead to an obstruction of venous outflow and decrease of capillary perfusion [15]. Patient related factors, including the metabolic and hormonal status, might play a more important role than considered to date [16].
Safety and Complications
Intramuscular fat cell transplantation has recently been implicated as being associated with serious and often fatal complications (eg, thromboembolic events), mainly related to the lipotransfer technique used. In 2015, a retrospective study by Cardenas and Camarena [17] enrolled 22 patients diagnosed with fat embolism after liposuction for buttock augmentation. For this complication, a special group of experts (Research Foundation Task Force) [18] was organized and found that in a total of 198,857 patients who underwent fat transfer surgery in the gluteal area, 135 patients were diagnosed with varying degrees of pulmonary embolism from fat and of these 32 ended up. The panel of experts concluded that fat emboli are directly related to intramuscular fat injections. A more thorough study of the pathophysiological mechanism of fat embolism suggested two aetiological mechanisms: the first was the mechanical obstruction of the pulmonary vessels by macroscopic fat particles and the second was the systemic inflammation of the lungs by the produced fatty acids, derived from the hydrolysis of micro -emboli from lipase, which leads to reactive airway obstruction from hemorrhage and edema. Fatty clots enter the circulation either by direct injection into the gluteal vein, or after traumatic rupture of the vein. Based on all the above, it is concluded that the increased possibility of fat embolism in this particular area of the body is due to the proximity of the muscle groups with large diameter venous stems, but also to the special space formed between the deep muscle groups, where the gradient of negative pressure can drive the microemboli into the systemic circulation.
A study from Conde-Green et al [19], showed that complications occur most frequently following intramuscular injection (28,7%) compared to subcutaneous fat grafting (4%). Similar results were reported from observations following fat injections into cadavers in the buttock area, which suggested a migration into the deep muscle plane [20]. Complication rates also increase with increasing volumes of injected fat, with a complication rate of 19% with fat injection of more than 1,000mL intramuscularly and subcutaneously per buttocks [21].
Discussion
Fat grafts have been widely used for more than a century in medicine. Despite a variety of other methods of soft tissue augmentation becoming available over the years, none have the “ideal” properties of autologous fat, namely, abundance, easy availability, and biocompatibility [22]. The greatest drawback at the current time is the unpredictable stability and longevity of the graft. While some authors claim impressive outcomes, others report disappointing long-term results, with up to 80% of the graft reportedly being reabsorbed [22].
The amount of fat graft resorption is highly dependent on the recipient tissue. The rich blood supply that characterizes muscle tissue led to the investigation of the survival of autologous fat after its intramuscular transplantation, and the comparison of the results with the corresponding results of fat grafting into subcutaneous tissue, which showed in most cases favourable results for the intramuscular plane [14].
Despite the favourable and comparatively superior survival outcomes of autologous adipose tissue grafts after its intramuscular injection, intramuscular fat transfer has recently been implicated as being associated with serious, and sometimes fatal, complications due to thromboembolic events, particularly in buttock augmentation surgery via intramuscular transplantation of large amounts of autologous fat [17,18]. The above data led to a revision of the surgical techniques in order to limit the risks and possible complications related to the above operations.
In contrast to intramuscular lipotransfer procedures in the gluteal muscles, intramuscular injection of autologous adipose tissue in other areas of the body, e.g., in the pectoral muscles in the context of breast reconstruction operations, has never been associated with similar serious complications. After all, autologous fat transplantation in the breast, both subcutaneously and intramuscularly, is a safe and fully established surgical methodology, as shown by many published studies [23-25].
Conclusion
Fat grafting is widely used as an approved method of volume reconstruction the last decades. Fat graft low integration rates can be associated with the recipient site as well as with the total volume injected and the technique used. Even though most experimental and clinical cases show an increased survival rate when fat grafts are injected intramuscularly, major complications can be associated with this application in specific sites i.e., the buttock area. Additional studies are needed to clarify the behavior of fat grafts in the muscles of different areas.
Disclosure Statement
The authors report there are no competing interests to declare.
References
- Gamboa GM, Ross WA (2013) Autologous fat transfer in aesthetic facial recontouring. Ann Plast Surg 70: 513-516. [Crossref]
- Wong T, McGrath JA, Navsaria H (2007) The role of fibroblasts in tissue engineering and regeneration. Br J Dermatol 156: 1149-1155. [Crossref]
- Bellini E, Grieco MP, Raposio E (2017) The science behind autologous fat grafting. Ann Med Surg (Lond) 24: 65-73. [Crossref]
- O'Neill RC, Abu-Ghname A, Davis MJ, Chamata E, Rammos CK, et al. (2020) The role of fat grafting in buttock augmentation. Semin Plast Surg 34: 38-46. [Crossref]
- Guerrerosantos J, Gonzalez-Mendoza A, Masmela Y, Gonzalez MA, Deos M, et al. (1996) Long-term survival of free fat grafts in muscle: an experimental study in rats. Aesthetic Plast Surg 20: 403-408. [Crossref]
- Karacaoglu E, Kizilkaya E, Cermik H, Zienowicz R (2005) The role of recipient sites in fat-graft survival: experimental study. Ann Plast Surg 55: 63-68. [Crossref]
- Perén PA, Gómez JB, Guerrerosantos J, Salazar CA (2000) Gluteus augmentation with fat grafting. Aesthetic Plast Surg 24: 412-417. [Crossref]
- Aygit AC, Sarikaya A, Doganay L, Top H, Cakir B, et al. (2004) The fate of intramuscularly injected fat autografts: An experimental study in rabbits. Aesthetic Plast Surg 28: 334-339. [Crossref]
- Shi Y, Yuan Y, Dong Z, Gao J, Lu F (2016) The fate of fat grafts in different recipient areas: subcutaneous plane, fat pad, and muscle. Dermatol Surg 42: 535-542. [Crossref]
- Nguyen PSA, Desouches C, Gay AM, Hautier A, Magalon G (2012) Development of micro-injection as an innovative autologous fat graft technique: the use of adipose tissue as dermal filler. J Plast Reconstr Aesthet Surg 65: 1692-1699. [Crossref]
- Baek RM, Park SO, Jeong EC, Sik Oh H, Kim SW, et al. (2012) The effect of botulinum toxin A on fat graft survival. Aesthetic Plast Surg 36: 680-686. [Crossref]
- Shi N, Su Y, Guo S, Zhang Z, Qiu L, et al. (2019) Improving the retention rate of fat grafts in recipient areas via botulinum toxin A treatment. Aesthet Surg J 39: 1436-1444. [Crossref].
- Wu M, Li Y, Wang Z, Feng J, Wang J, et al. (2020) Botulinum toxin a improves supramuscular fat graft retention by enhancing angiogenesis and adipogenesis. Dermatol Surg 46: 646-652. [Crossref]
- Yi Y, Hu W, Zhao C, Wu M, Zeng H, et al. (2021) Deciphering the emerging roles of adipocytes and adipose-derived stem cells in fat transplantation. Cell Transplant 30: 963689721997799. [Crossref]
- Largo RD, Tchang LA, Mele V, Scherberich A, Harder Y, et al. (2014) Efficacy, safety and complications of autologous fat grafting to healthy breast tissue: a systematic review. J Plast Reconstr Aesthet Surg 67: 437-448. [Crossref]
- Bills JD, Derderian C, Barker J, Lowe A, Lavery LA, et al. (2015) The role of estrogen in the modulation of autologous fat graft outcomes. Plast Reconstr Surg 135: 103e-113e. [Crossref]
- Cárdenas-Camarena L, Bayter JE, Aguirre-Serrano H, Cuenca-Pardo J (2015) Deaths caused by gluteal lipoinjection: what are we doing wrong? Plast Reconstr Surg 136: 58-66. [Crossref]
- Mofid MM, Teitelbaum S, Suissa D, Ramirez-Montañana A, Astarita DC, et al. (2017). Report on mortality from gluteal fat grafting: recommendations from the ASERF task force. Aesthet Surg J 37: 796-806. [Crossref]
- Condé-Green A, Kotamarti V, Nini KT, Wey PD, Ahuja NK, et al. (2016) Fat grafting for gluteal augmentation: a systematic review of the literature and meta-analysis. Plast Reconstr Surg 138: 437e-446e. [Crossref]
- Del Vecchio DA, Villanueva NL, Mohan R, Johnson B, Wan D, et al. (2018) Clinical implications of gluteal fat graft migration: a dynamic anatomical study. Plast Reconstr Surg 142: 1180-1192. [Crossref]
- O'Neill RC, Abu-Ghname A, Davis MJ, Chamata E, Rammos CK, et al. (2020) The role of fat grafting in buttock augmentation. Semin Plast Surg 34: 38-46. [Crossref]
- Locke MB, de Chalain TM (2008) Current practice in autologous fat transplantation: suggested clinical guidelines based on a review of recent literature. Ann Plast Surg 60: 98-102. [Crossref]
- Delay E, Sinna R, Ho Quoc C (2013) Tuberous breast correction by fat grafting. Aesthet Surg J 33: 522-528. [Crossref]
- Sinna R, Delay E, Garson S, Delaporte T, Toussoun G (2010) Breast fat grafting (lipomodelling) after extended latissimus dorsi flap breast reconstruction: a preliminary report of 200 consecutive cases. J Plast Reconstr Aesthet Surg 63: 1769-1777. [Crossref]
- Demiri EC, Dionyssiou DD, Tsimponis A, Goula CO, Pavlidis LC, et al. (2018) Outcomes of fat-augmented latissimus dorsi (FALD) flap versus implant-based latissimus dorsi flap for delayed post-radiation breast reconstruction. Aesthetic Plast Surg 42: 692-701. [Crossref]