Intraosseous schwannomas are benign neoplasms that originate from the neural sheath. Most common occurrence sites being soft tissues of head and neck, intraosseous schwannomas are rare. This case report presents an unusual location of an intraosseous schwannoma of the mandible and its management.
intraosseous schwannoma, mandible
Schwannomas or neurilemmomas are benign non-odontogenic tumours derived from schwann cells, which are responsible for the production of myelin sheath covering peripheral nerves [1,2]. The most common cause of proliferation of the schwann cells in the perineurium are displacement and compression of the nerve sheath. Schwannomas are mainly slow growing, well defined, unilocular and encapsulated lesions presenting variable symptoms [3]. Intraoral schwannomas account for 1% of all head and neck region tumours, commonly reported on the base region of the tongue. Intraosseous schwannomas are rare and mandible, particularly in the posterior segment of the body and ramus, is the most common site of occurrence due to the bony intraosseous path of the inferior alveolar nerve [1]. Radiologically differential diagnosis should be made based on the presence of mandibular canal dilation, which includes angiofibroma, neurofibroma, leimyoma or vascular malformations. In the absence of canal dilation, it is difficult to differentiate from unilocular, well defined border radiolucent images of keratocytes, periodontal cysts, ameloblastomas or periapical inflammatory lesions. In these situations intraoperative direct attachment of the tumour to the neurovascular bundle gives an idea on differential diagnosis [4]. Treatment of choice is conservative surgical enucleation in cases where the integrity of mandible is not compromised. Recurrences are rare after total removal of the tumour [5]. This case report presents a rare location of an intraosseous schwannoma of the mandible on an edentulous area and its surgical management.
A 58 years old female patient was referred to the clinic with a complaint of slight localized swelling on right mandibular molar region stating the swelling was smooth and little in size for the last 12 months but moderately increased lately. On intraoral examination, swelling was observed on the edentulous vestibular area of the right posterior mandible located between the second premolar to retromolar area (Figure 1). The mucosa over the swelling was intact, normal in colour whereas on palpation, it was well-demarcated, tender and firm. There was no sign of any trauma or inflammation even after the removal of partial prosthesis for a long time. On neurosensory examination two-point discrimination and light touching tests showed normal sensation on lower lip and buccal mucosa.

Figure 1. Intraoral appearance of the lesion on the right mandible.
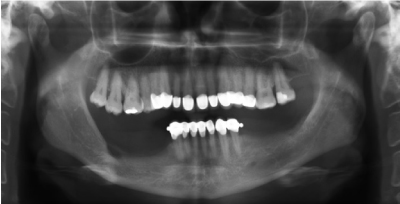
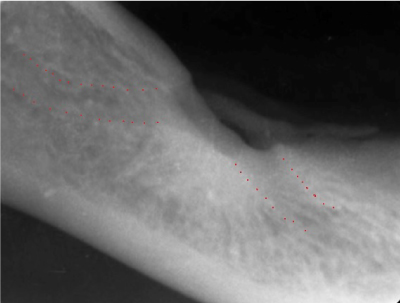
On orthopantomography, well-circumscribed, unilocular, radiolucent lesion with a sclerotic border which kept track with the intraosseous path of mandibular canal was observed (Figure 2). Cortical erosion on the superior border with focal radiopacity inferior to the lesion were seen on periapical radiography (Figure 3).
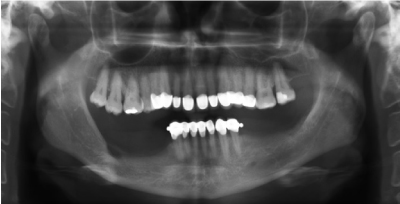
Figure 2. Orthopantomography showing a well-circumscribed, unilocular radiolucent lesion on the posterior mandible.
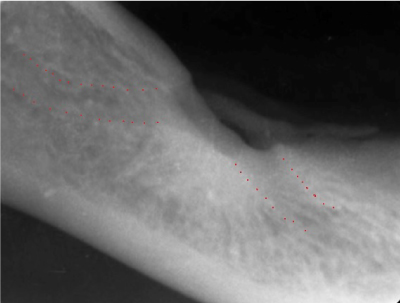
Figure 3. Periapical radiography showing cortical erosion and focal radiopacity.
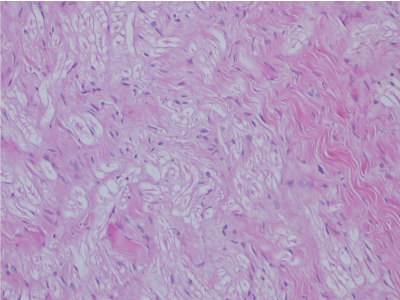
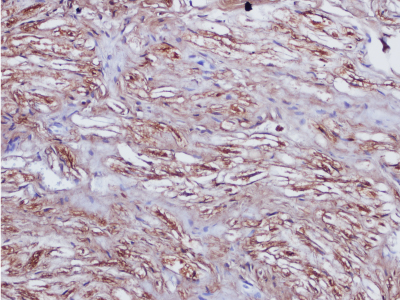
Before the surgery fine-needle aspiration was performed and aspiration was negative. Complete surgical enucleation was performed under intravenous sedation. Direct attachment of the encapsulated lesion to inferior alveolar neuro-vascular bundle was observed and careful blunt dissection was performed preserving the integrity of the nerve. Histopathologically schwannoma was diagnosed. It was typically characterized by encapsulation with Antoni A and Antoni B areas usually coexisting in the lesion with possible presence of nuclear palisading, spindle shaped cells and verocay bodies. Antoni type A areas were relatively cellular, in contrast Antoni type B tissue was composed of less cellular and less organized nonorganoid areas. Diffuse immunoreactivity for S-100 protein was observed, however, the staining was diminished in Antoni type B areas (Figure 4,5). A post-operative neurosensory disturbance was observed for 4 weeks with full recovery and no recurrences at 12-month follow-up.
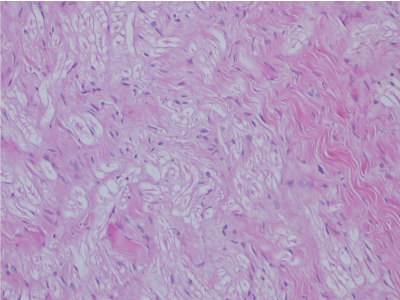
Figure 4. Hematocylin and eosin section of an intraosseous schwannoma (original magnification × 200).
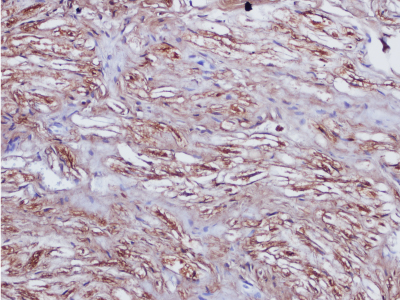
Figure 5. A high power photomicrograph of an intraosseous schwannoma depicts Antoni A tissue with spindle shaped cells, nuclear palisading and verocay bodies (original magnification × 200).
Nowadays, in the point of pathologist’s view, schwannoma, neurilemmoma, neurinoma and perineural fibroblastoma are considered be synonymous terms and must be distinguished from neurofibroma [6]. While schwannomas are encapsulated lesions, due to lack of encapsulation neurofibromas tend to recur frequently and have the increased potential for malignant transformation [6]. Schwannomas are slow growing tumours therefore before becoming symptomatic they could be present for years [3]. Swelling is the most common symptom whereas paresthesia or pain could be present in half of the cases.
There are three mechanisms by which schwannomas may involve bone:
- A tumour may arise centrally with in a bone,
- A tumour may arise within a nutrient canal,
- A soft tissue or periosteal tumour may cause secondary erosion and penetration into bone [7].
In literature, a female predilection, with a 1.6:1 female to male ratio and a peak prevalence of diagnosis in second and third decades of life were reported [8]. In a review of 60 intraosseous schwannoma cases in the jaws, 40 lesions were localized on the posterior body/ramus region of mandible, of 15 on the anterior body including symphysis region and of 5 on the maxilla [9]. In the presented case lesion was localized in edentulous retromolar area of mandible. This localization is consistent with a marked tendency to be located in the lower posterior jaw.
The typical radiographic presentation of mandibular schwannomas has been reported as being well demarcated, unilocular radiolucency with a thin sclerotic border. Cortical thining/erosion, external root resorption, cortical expansion, focal radiopacity and peripheral scalloping have also been occasionally evident [10]. In present case since the lesion was located in the edentulous area, the radiographic findings were similar with the reported cases.
Vascular malformations should be considered in differential diagnosis in the presence of enlargement of mandibular canal which was ruled out in this case report due to negative aspiration. Histopathological examination is necessary for a definite diagnosis [8]. Microscopically, the tumour is classified into two basic types of tissue Antoni A and Antoni B. Diffuse immunoreactivity for S-100 protein is routinely observed in schwannomas; however, staining is diminished in Antoni B areas [9,11].
The treatment of choice is conservative surgical enucleation with periodic follow-up examinations. Recurrence was reported only in five cases in mandible, which was attributed to malignant cases or incomplete removal [9]. Nerve injury is the major complication in the surgical management of these lesions, therefore careful dissection from the surrounding tissues is important to prevent neurologic disturbance. Long-term follow up is necessary for evaluation of recurrences. In conclusion, schwannoma should be considered in differential diagnosis in the presence of unilocular and well-defined border lesions located in edentulous mandibles.
- Murphy J, Giunta JL (1985) Atypical central neurilemmoma of the mandible. Oral Surg Oral Med Oral Pathol 59: 275-278. [Crossref]
- Villanueva J, Gigoux C, Solé F (1995) Central neurilemmoma of maxilla. A case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 79: 41-43. [Crossref]
- Martins MD, Anunciato de Jesus L, Fernandes KPS, Bussadori SK, Taghloubi SA, et al. (2009) Intra-oral schwannoma: case report and literature review. Indian J Dent Res 20: 121–125. [Crossref]
- Sciubba JJ, Sachs SA (1980) Schwannoma of the inferior alveolar nerve in association with the organ of Chievitz. J Oral Pathol 9: 16-28. [Crossref]
- Buric N, Jovanovic G, Pesic Z, Krasic D, Radovanovic Z, et al. (2009) Mandible schwannoma (neurilemmoma) presenting as periapical lesion. Dentomaxillofac Radiol 38: 178–181. [Crossref]
- Belli E, Becelli R, Matteini C, Iannetti G (1997) Schwannoma of the mandible. J Craniofac Surg 8: 413-416. [Crossref]
- Buranovic M, Macan D, Begovic EA, Luksic I, Brajdic D, et al. (2006) Schwannoma with secondary erosion of mandible: Case report with review of the literature. Dentomaxillofac Radiol 35: 456-460. [Crossref]
- Simsek HO, Aksoy MC, Can C, Baykul T (2012) Intraosseous Schwannoma of the Mandible. Saini R, editor. International Journal of Experimental Dental Science 1: 48–50.
- Chi AC, Carey J, Muller S (2003) Intraosseous schwannoma of the mandible: a case report and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 96: 54–65. [Crossref]
- Zhang F, Lu F, Jiang J, Wang H (2015) Two Case Reports and an Updated Review of Spinal Intraosseous Schwannoma. J Korean Neurosurg Soc 57: 478–83. [Crossref]
- Goldblum JR, Folpe AL, Weiss SW, Enzinger FM, Weiss SW (2001) Enzinger and Weiss’s soft tissue tumors. 4th ed. St Louis: Mosby-Year Book, Inc; 1111-1200.