Case Report
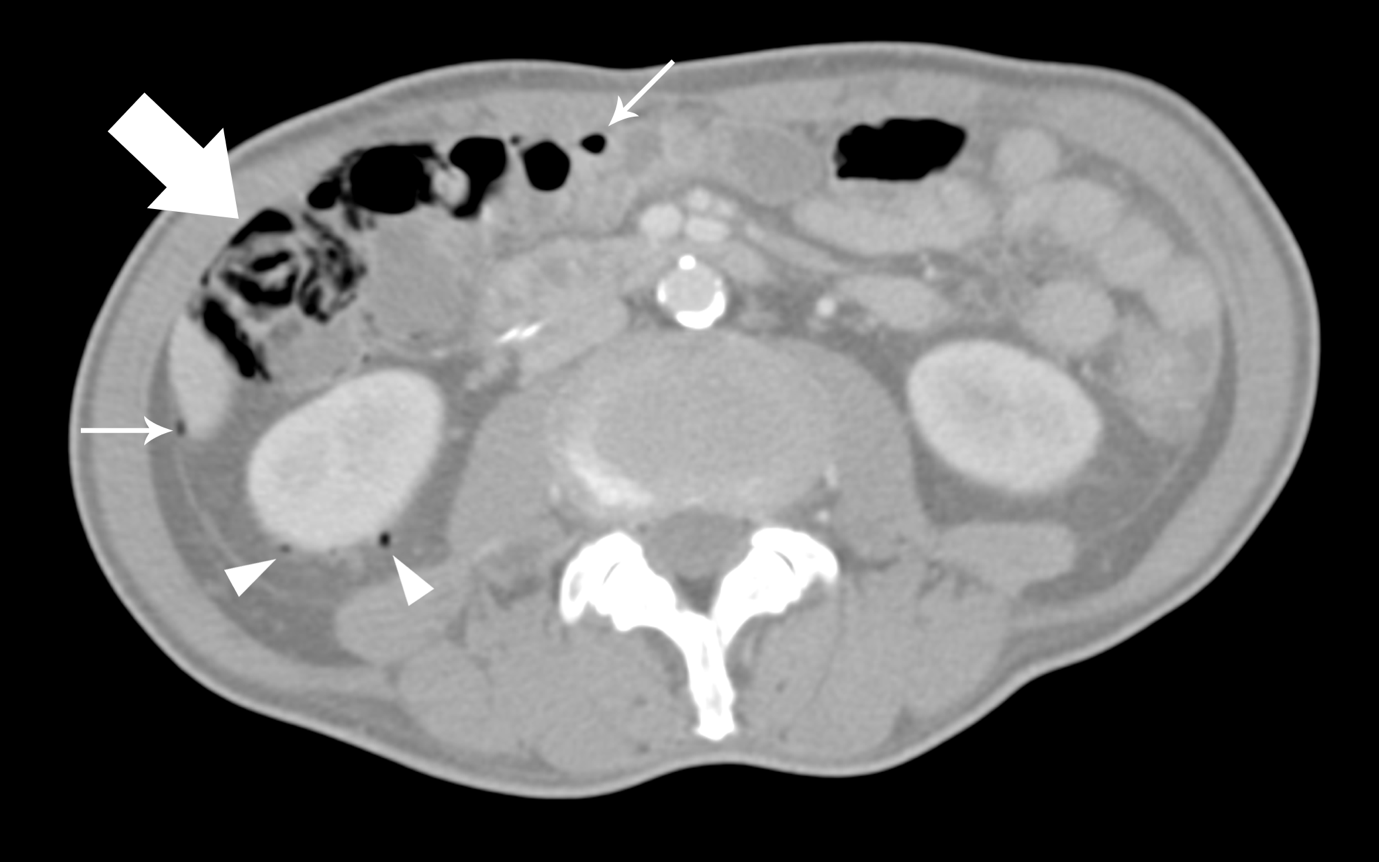
We report a case of a 64-year-old undergoing definitive chemoradiation for stage IVA oesophageal carcinoma. 6 days after his 4th cycle of chemotherapy, he reported 10 episodes of watery stools daily and abdominal discomfort. He was neutropenic with an absolute neutrophil count of 0.58 x 109/L. An abdominal radiograph showed pneumatosis coli in the right hemicolon. This was confirmed on a computed tomography (CT) scan which also showed pockets of intraperitoneal and retroperitoneal gas. In view of worsening neutropenia, non-resolving abdominal pain, distension and fever after 2 days coupled with the presence of extraluminal gas on CT (Figure 1 and 2), he underwent a diagnostic laparoscopy [1,2].

Figure 1: Contrast-enhanced axial (A) and coronal (B) CT images showing pneumatosis coli along the ascending colon and extending to the hepatic flexure (arrow).
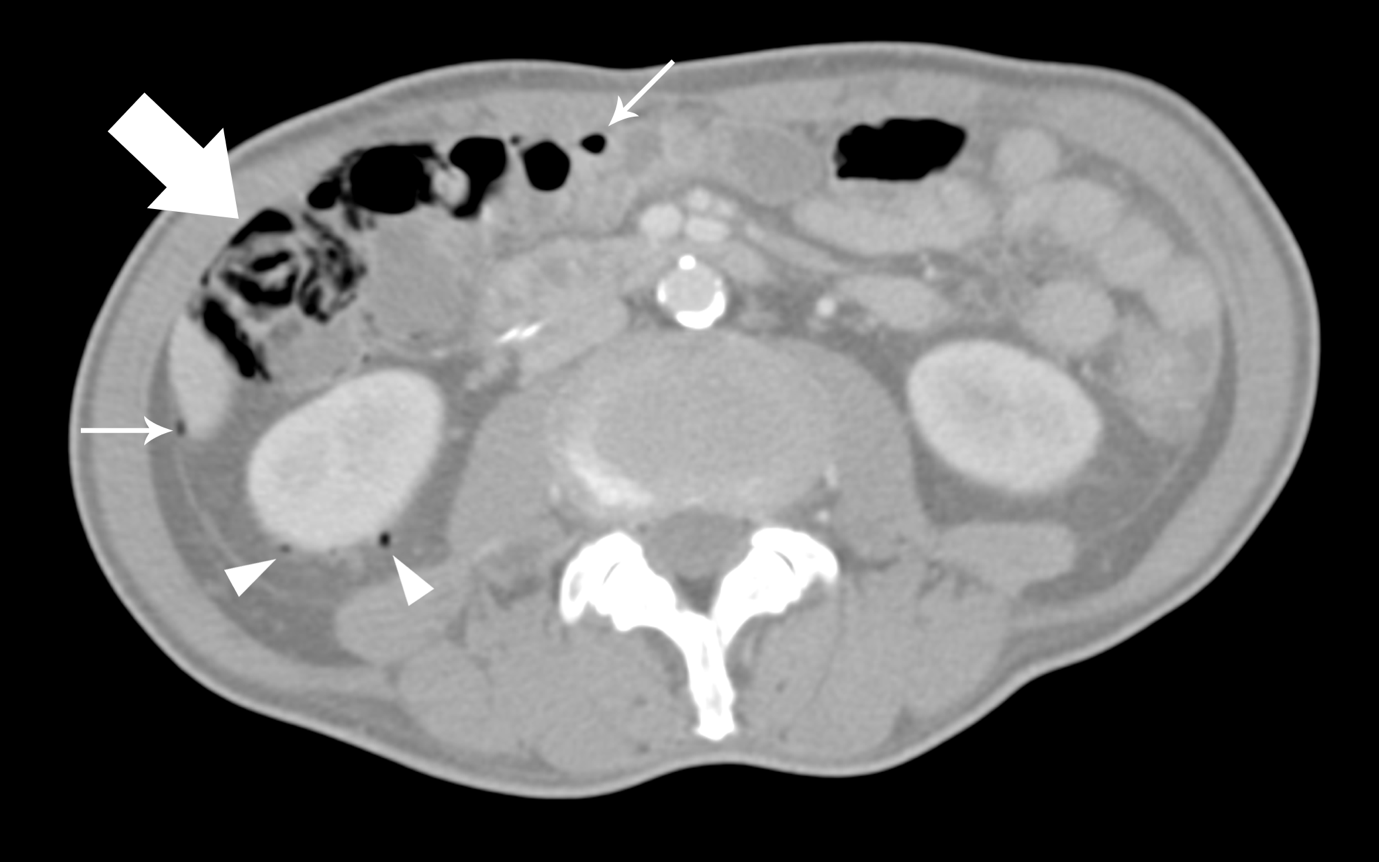
Figure 2: Axial contrast-enhanced CT image showing pneumatosis coli along the ascending colon (thick arrow) along with small pockets of intraperitoneal (thin arrows) and retroperitoneal (arrowheads) gas.
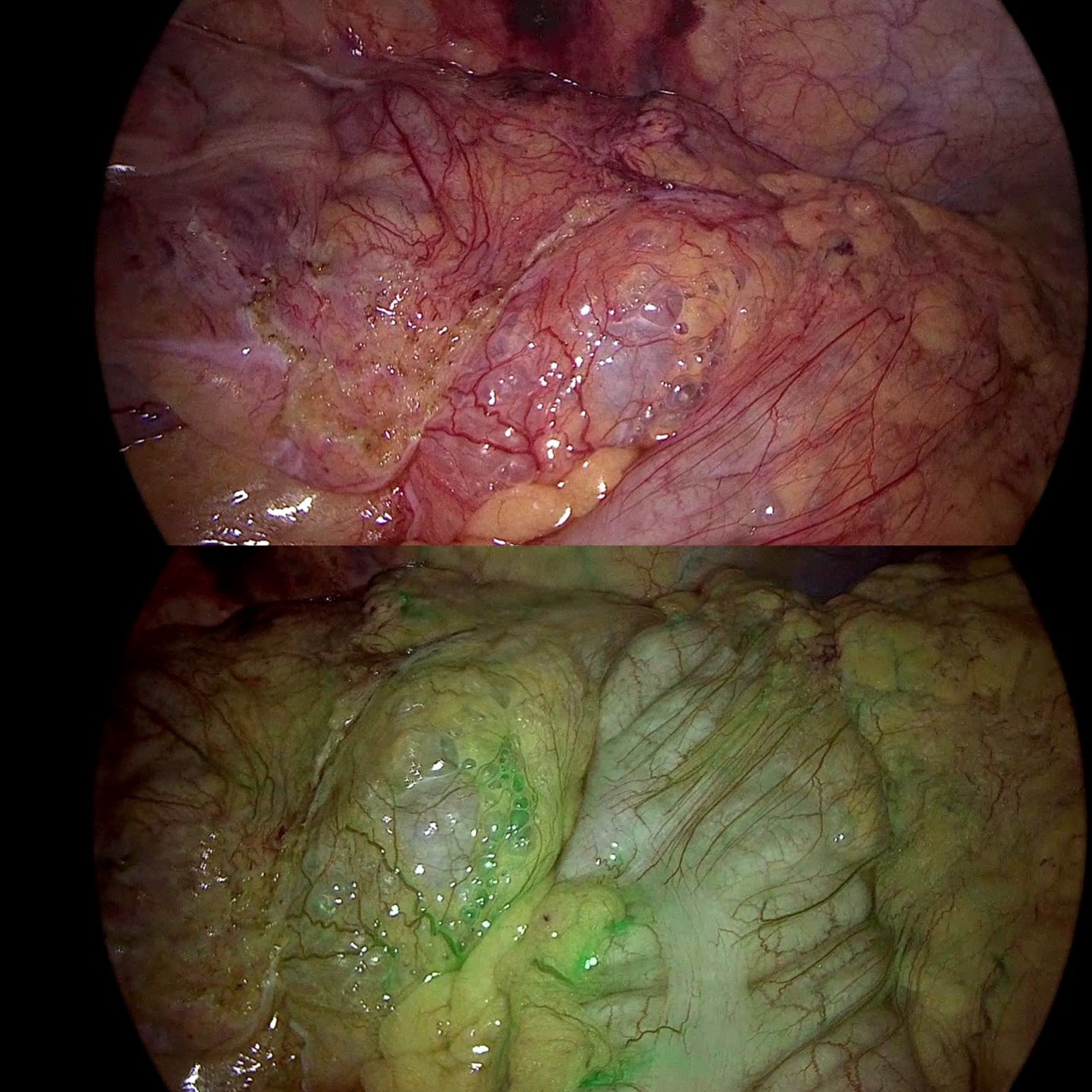
Intra-operatively, apart from pneumatosis seen from mid-ascending to proximal transverse colon, his colon looked healthy and perfusion was checked with indocyanine green (Figure 3). The impression was that of colitis without perforation and his diarrhea resolved with supportive management.
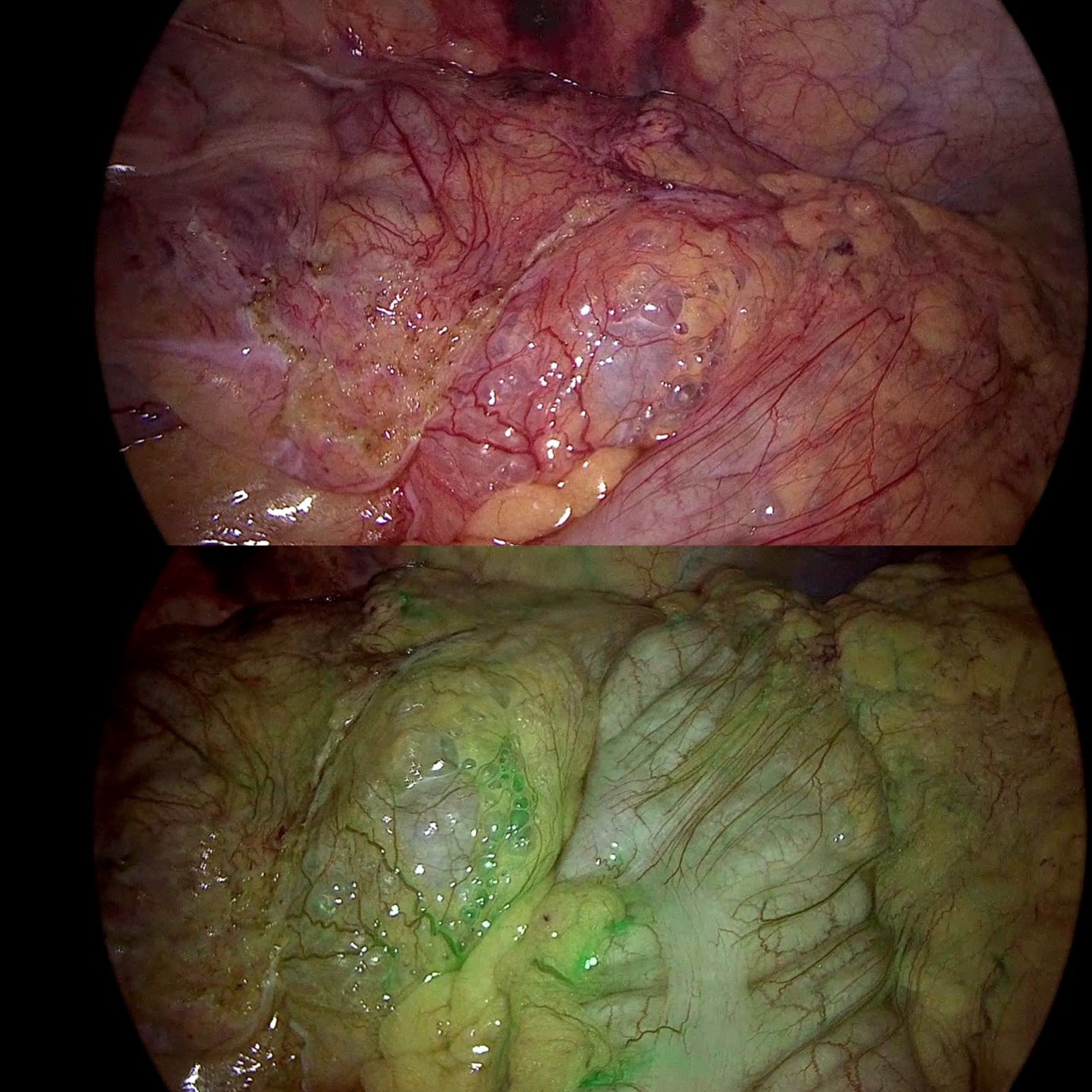
Figure 3: Pneumatosis coli on laparoscopy without (above) and with (below) indocyanine green fluorescence imaging demonstrating good bowel perfusion.
Discussion
Cancer treatments are associated with adverse events of which pneumatosis intestinalis (PI) is rare, occurring in about 0.03%i of patients but potentially life-threatening. A systematic review found that the median time of onset was 6 weeks and most commonly occurred in the large bowel. Though symptoms were frequently mild if at all present and most cases resolve with conservative management, there have been reports of delayed bowel perforation leading to rapid deterioration [3,4].
Some authors have proposed two main mechanisms in the development of PI. The bacterial theory hypothesizes that gas producing bacteria such as Escheria coli and Clostridia can invade the intestinal wall, which is supported by the decrease in gas after antibiotics and proximity of the gas cysts near blood vessels. Alternatively, the mechanical theory proposes mucosal disruption from increased luminal pressure or due to inflammation/chemotherapy.
Conclusion
It has been postulated that PI can be considered benign in the absence of worrisome features such as portovenous gas, decreased bowel wall enhancement and bowel dilatation. Although these features were not present for our case, we were compelled to intervene in view of persistent symptoms despite antibiotics. Patients with PI can be conservatively managed in the absence of worrisome features, but close observation is required with a low threshold for intervention.
References
- Gazzaniga G, Villa F, Tosi F, Pizzutilo E, Colla S, et al. (2022) Pneumatosis Intestinalis Induced by Anticancer Treatment: A Systematic Review. Cancers 14: 1666. [Crossref]
- Kim J, Lee S, Do B (2022) Pneumatosis intestinalis with delayed onset small bowel perforation: a case report. J EMS Med 1: 31-35.
- Torres US, Fortes CDFM, Salvadori PS, Tiferes DA, Ippolito GD (2018) Pneumatosis From Esophagus to Rectum: A Comprehensive Review Focusing on Clinico-Radiological Differentiation Between Benign and Life-Threatening Causes. Semin Ultrasound CT MR 39: 167-182. [Crossref]
- Ko S, Hong SS, Hwang J, Kim H, Chang Y, et al. (2018) Benign versus life-threatening causes of pneumatosis intestinalis: differentiating CT features. Rev Assoc Med Bras 64: 543-548. [Crossref]