Aim: Wrong level surgery continues to be a major cause for litigation in spine surgery. We aim to demonstrate a method to minimise the incidence of wrong level surgery in the more challenging thoracic spine cases.
Methods: We use the case of a patient undergoing a T9/T10 discectomy in which we placed pre-operative radio-opaque tantalum beads within the pedicle of the T9 vertebrae under CT guidance to allow for intra-operative level identification.
Results: The method allowed for clear intra-operative identification of the level and cross-referencing with pre-operative CT without complication.
Conclusion: The use of CT guidance provides excellent accuracy for pre-operative marker placement & the specific use of tantalum beads allows for clear marker identification intra-operatively. We have found this method to be safe, and in our experience it more reproducible and accurate than other techniques that we have previously used.
Pre-operative, Tantalum beads, spinal surgery, CT scan, fluoroscopy
Wrong level spinal surgery continues to be a major source of litigation for orthopaedic and neurosurgeons worldwide with wrong level exposure ranging between 0.32% - 15% of all cases [1]. Some reports state that as many as one in two spinal surgeons will perform a wrong site surgery at some point in their careers [2]. The impact of these errors on the health and wellbeing of the patient cannot be understated, and the emotional and professional cost on the surgeon, as well as the financial cost of litigation are also considerable.
The most important factors impacting the assessment of spinal level intraoperatively using the conventional method of palpation of bony anatomy with fluoroscopy confirmation include body habitus of the patient and variation in the vertebral anatomy [3]. Atypical numbers of vertebrae are surprisingly common in the population, with some studies stating rates as high as 10% in clinically asymptomatic patients [4]. Presence of acquired or congenital spinal deformity also reduces the accuracy of palpation as a localisation method [5]. The lack of uniquely identifiable radiological landmarks in the thoracic spine makes localisation more difficult. Finally, human error in the form of inaccurate counting, cannot be discounted as a factor. Other novel methods of localisation include placement of sterile needles as markers, placement of percutaneous fiducial markers preoperatively, and computer-based algorithms amongst others, though none of these methods are currently widely used [6-8].
We present a method that the authors feel provides an accurate and reproducible technique that can assist surgeons in the intra-operative identification of correct and intended spine level, with the pre-operative placement of radio-opaque beads.
A 79-year-old female who was listed for a T9/10 Discectomy (Figure 1), to be performed through an anterior approach. Due to the Thoracic location of the disc, there was an increased risk of wrong level surgery and so we utilised a previously undescribed technique where we executed CT guided pre-operative placement of radio-opaque beads within the pedicle of a specific and pre-determined spinal vertebrae. These radio-opaque beads then act as a reference for the operating surgeon when using intra-operative fluoroscopy.
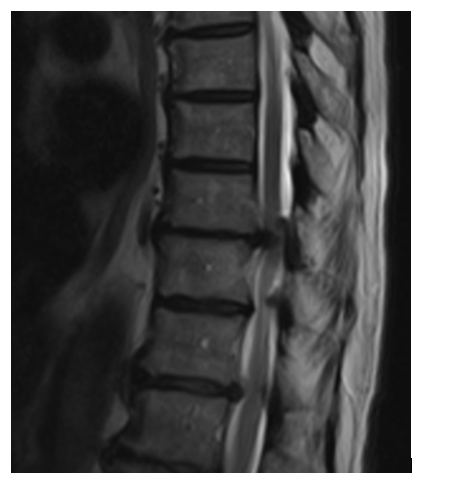
Figure 1: T2 Weighted Sagittal MRI Images illustrating the patient’s pre-operative pathology.
Prior to the date of intended spine surgery, the patient attended a CT list by a Consultant Radiologist. A CT scanogram of the whole spine is performed to assess for any vertebral abnormalities and to allow for accurate counting of the vertebrae. Under CT guidance the pedicle of the chosen vertebra is identified. Using aseptic technique and following administration of local anaesthetic, a 11gx15cm Jamshidi needle was then inserted into the left pedicle of the T9 vertebra. Once position is confirmed on imaging (Figure 2), the central core of the Jamshidi was removed and 4 sterile 1mm Tantalum beads were inserted into the needle. The central core introducer was then re-inserted to push the beads down the needle and into the pedicle. The bead position is then confirmed following removal of the Jamshidi needle. Finally, a lateral scout of the whole spine is obtained also to confirm level (Figure 3). On the day of surgery, intra-operative fluoroscopy is used to identify the vertebra containing the radio-opaque Tantalum beads (Figure 4), thereby allowing surgery to proceed at the correct level.
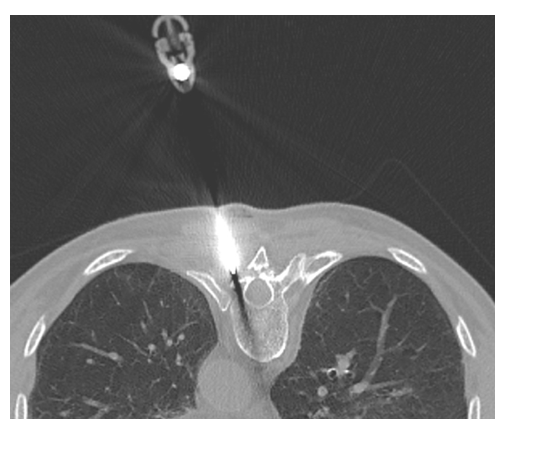
Figure 2: CT Guided insertion of Tantallum beads into the Left T9 Vertebra.

Figure 3: Pre-and post-insertion Scanograms to confirm level and bead placement.
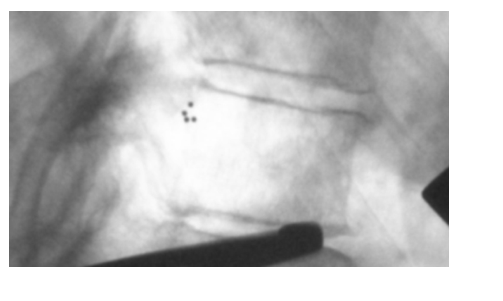
Figure 4: Intra-operative fluoroscopic image of the T9 Vertebra, with the Radio-opaque beads confirming level.
The use of anatomical landmarks and fluoroscopic counting continues to be the most widely utilised technique for level identification, despite being prone to error. Although many other techniques have been described each has their own disadvantages that we feel have prevented widespread utilisation. Intra-operative sterile needle insertion or K wire insertion can augment fluoroscopic counting by providing a visual and radio-opaque reference but can be time consuming and these techniques are still susceptible to miscounting. Pre-operative skin markers, although non-invasive, can undergo significant movement with skin shifting, particularly in obese patients. Likewise, placement of methylene blue is only suitable for posterior surgery after skin incision and the potential spread of dye within the tissue can compromise its accuracy. Pre-operative percutaneous vertebroplasty offers a more accurate alternative however, there it is more prone to complication such as infection, cement extravasation, pulmonary embolism. Additionally, it can be difficult to differentiate intra-operatively from sclerotic bone. Finally, CT algorithms and Image Guided (IG) with Robotics are likely to have an increased role in spine surgery and level identification in the future, but currently most units are not resourced to utilise such technology and further developments are required [8,9].
To date we have utilised this technique in four cases with accurate intra-operative identification of the desired spine level and no associated complications. From what has previously been described we feel that the use of tantalum beads offers an excellent development in the use of radio-opaque markers that are safe and simple to insert. Furthermore, using CT to guide their pre-operative insertion provides an incredibly accurate method of spine level localisation. Together with its accuracy the senior authors feel the technique significantly reduces intra-operative fluoroscopy time by removing the need for sequential pre- and post-incision fluoroscopic level counting.
We understand there may be concern with the long-term implantation of the tantalum beads but for over 40 years Radiostereometric Analysis (RSA) has been safely performed almost exclusively with the safe implantation of tantalum beads [10]. The tantalum beads inserted are manufactured sterile and supplied by Halifax Biomedical Inc. with American (FDA) and European (CE) approval for implantation in bone and soft tissue. We have been inserting them into bone as part of RSA trials within our unit for over 10 years without complication or concern. The small size of the beads is also advantageous as they are unlikely to cause issue should instrumentation of the vertebrae be required in the future.
With the use of CT, the patient’s overall radiation exposure should also be considered with this technique. For a thoracic discectomy like the one in the case illustrated, we would routinely perform a pre-operative CT scan to assess for calcification of the intervertebral disc. Therefore, these patients are not exposed to any increased radiation than they would with current practice. We do appreciate however, that pre-operative CT scans are not routine for all spinal surgery and in those cases the radiation exposure must be considered with a patient specific risk versus benefit analysis, reserving the technique for thoracic level surgery of case in which level identification is expected to be challenging. It should also be discussed with the patient during their consenting process. In our experience, this was less than 500 mGy cm2 and we aim to do further work in the future to assess to what degree intra-operative fluoroscopy time is reduced with our technique.
In summary, we illustrate a method for the intra-operative determination of the correct spinal level and thereby reducing the risk of wrong level surgery. We feel the technique is simple, safe and reproducible. Furthermore, in our experience, it allows a more accurate and reliable method than others described within the literature. We are accepting that the implications mentioned previously are not justified for all operations of the spine and the technique should instead be reserved for those cases where correct level identification is expected to be difficult.
- Mayer JE, Dang RP, Duarte Prieto GF, Cho SK, Qureshi SA, et al. (2014) Analysis of the techniques for thoracic- and lumbar-level localization during posterior spine surgery and the occurrence of wrong-level surgery: results from a national survey. Spine J 14: 741-748. [Crossref]
- Groff MW, Heller JE, Potts EA, Mummaneni PV, Shaffrey CI, et al. (2013) A Survey-Based Study of Wrong-Level Lumbar Spine Surgery: The Scope of the Problem and Current Practices in Place to Help Avoid These Errors. World Neurosurg 79: 585-592. [Crossref]
- Epstein NE (2017) More risks and complications for elective spine surgery in morbidly obese patients. Surg Neurol Int 8:66.
- Hu Z, Zhang Z, Zhao Z, Zhu Z, Liu Z, et al. (2016) A neglected point in surgical treatment of adolescent idiopathic scoliosis: Variations in the number of vertebrae. Medicine (Baltimore) 95: e4682. [Crossref]
- Tee JW, Rutges J, Marion T, Street J, Paquette S, et al. (2017) Factors predictive of topographical accuracy in spine level localization. J spine Surg (Hong Kong) 3: 23-30.
- Chin KR, Pencle FJR, Kubik J, Coombs AV, Seale JA, et al. (2015) Avoidance of Wrong Level Surgery in the Lumbar Spine: A Technical Report. J Spine 4: 1-3.
- Madaelil TP, Long JR, Wallace AN, Baker JC, Ray WZ, et al. (2017) Preoperative Fiducial Marker Placement in the Thoracic Spine. Spine (Phila Pa 1976) 42: E624-E628. [Crossref]
- Lo SL, Otake Y, Puvanesarajah V, Wang AS, Uneri A, et al. (2015) Automatic Localization of Target Vertebrae in Spine Surgery. Spine (Phila Pa 1976) 40: E476- E483. [Crossref]
- Kochanski RB, Lombardi JM, Laratta JL, Lehman RA, O'Toole JE (2019) Image-Guided Navigation and Robotics in Spine Surgery. Neurosurgery 84:1179–1189. [Crossref]
- Valstar ER, Gill R, Ryd L, Flivik G, Börlin N, et al. (2005) Guidelines for standardization of radiostereometry (RSA) of implants. Acta Orthop 76: 563–572. [Crossref]
