Purpose This cross-sectional survey investigated how Ontario private practice physiotherapists (PTs) who participated in the study, make clinical decisions about pregnancy-related pelvic girdle pain (PPGP) and also evaluated differences between pelvic health and orthopaedic PTs in their knowledge of PPGP clinical practice guidelines (CPGs).
Methods: An electronic survey was developed and distributed to private practice PTs recruited via physiotherapy associations and organizations. It included questions about management strategies, best practices, and perspectives on CPGs.
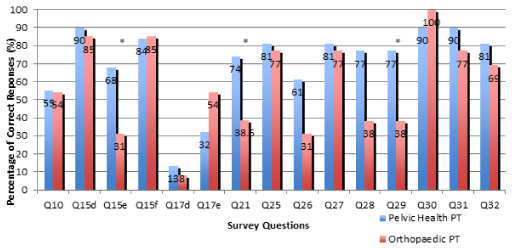
Results: Seventy-eight individuals responded, 44 were included in the study (31 pelvic health, 13 orthopaedic). Pelvic health PTs had increased awareness regarding CPGs compared to orthopaedic PTs (74% vs. 38.5%, p<0.05), selected correct pain terminology (77% vs. 38%, p<0.05), and correctly found age as non-risk for PPGP (68% vs. 31%, p<0.05). This did not translate to clinical practice, as both groups selected management strategies incongruent with PPGP CPGs.
Conclusion: The findings demonstrate that awareness of PPGP CPGs does not transfer into clinical practice, as participants selected treatment strategies that were incongruent with the current PPGP CPGs.
Women’s Health, Pelvic girdle pain, Clinical practice guidelines, Clinical decision Making
Pelvic girdle pain (PGP) denotes pain experienced through the lumbopelvic region that might radiate into the posterior aspect of the thigh [1]. Pregnancy-related pelvic girdle pain (PPGP) is a subcategory of PGP that differs in the etiology as it is related to pregnancy and associated physiological influences [1]. The prevalence of PPGP and back pain has been reported to be as high as 50% [2], with the reported point prevalence of PPGP alone being 20% [1]. Approximately 20-25% of all pregnant women suffer from PPGP such that medical intervention is sought out [2].
Importantly, persistent PPGP in the postpartum period is estimated to occur in 7-25% of women, where 8-10% continue to have PPGP up to two years after delivery [3]. The etiology for PPGP is unclear yet understood to be multifactorial. The most cited contributors to PPGP to date are biomechanical and hormonal [1,4,5]. Recent evidence has shown no correlation between PPGP and pelvic floor muscle weakness [6], yet there is an association
between PPGP and pelvic floor tenderness [7]. Of note, central pain mechanisms are emerging as important drivers of PPGP [3,5,8]. The psychosocial impacts of PPGP are well documented [5]. These issues are closely tied to physical limitations as these women find it difficult to work, sleep, and undertake normal activities [9]. Emotional distress, depression and anxiety, and stress, are considered strong prognostic indicators of ongoing disability in PPGP [5,10]. These psychological health indicators mark a three-fold risk of developing postpartum depression [11] and also demonstrate high correlations with disability and fear of movement [12], including avoidance of future pregnancies [13]. Interpersonal relationships have been found to suffer during the transition to the role of motherhood [14]. These outcomes can also have a socioeconomic impact, as persistent PPGP has a higher prevalence of sick leave and healthcare utilization [8]. As such, in light of emerging pain science psychosocial correlates of PPGP are likely bidirectional in nature. Risk factors associated with PPGP include parity, previous low back pain, work dissatisfaction, and a lack of belief in improvement [3,14]. Increased body mass index and weight gain during pregnancy have also been reported as risk factors [3,14], but these studies included participants with low back pain and PPGP, making it difficult to attribute these risk factors to PPGP alone [1]. Studies involving participants with only PPGP did not show significant correlations between weight gain or increased body mass index [1]. Epidemiologic research has shown that women with PPGP are more likely to have a first degree relative with PPGP, but the role of genetics in PPGP is still unknown [15]. In the United Kingdom, it is common practice for physiotherapists to manage pregnant women with musculoskeletal pain [16]. In Sweden, it was reported that women with PPGP most commonly sought out community PTs after delivery, with a total of 24 visits [8], and these PTs can be both publicly or privately funded without the need for a physician’s referral [8,17]. The majority of women reported that physiotherapy had some effect on their symptoms.8 It is unknown as to how frequently physicians refer women with PPGP to PTs in Ontario.
This study sought to examine how Ontario PTs working with pregnant women within a private practice setting make clinical decisions regarding PPGP. One objective was to assess the level of awareness and knowledge regarding PPGP Clinical Practice Guidelines (CPGs). A secondary objective was to determine if there were differences between clinical decision-making approaches between pelvic health and orthopaedic PTs. It was hypothesized that pelvic health PTs would practice in a manner more highly congruent with CPGs based on the specificity of their post-graduate training.
Participants
This study included Registered orthopaedic and pelvic health PTs employed in a private practice setting in Ontario. Pelvic health PTs were those rostered for “assessment and treatment of internal pelvic musculature” [18]. Orthopaedic PTs were those that self identified as such and had completed at least one of the orthopaedic course levels. Informed consent was obtained from all participants in the study (Appendix A). This study was approved by the ethics committee of the XXXX Research Ethics Board (Project 1625).
Survey Development
Creation of electronic survey
The survey was based on a previous study that examined this topic in the public sector. The tool was adapted for private practice and incorporated the 2008 European and 2012 Irish Guidelines and cross referenced the answers of the survey with the 2016 Clinton Guidelines and was developed using SurveyMonkey®. It assessed knowledge of risk factors, objective assessment and treatment strategies for PPGP, and opinions of CPGs.
Pilot testing
The survey was sent December 2016 to a volunteer group of five Master educated private practice Ontario PTs (2 pelvic health and 3 orthopaedic PTs) to ensure its validity, readability, and clarity. The majority (60%) of this group had between 1-5 years of overall clinical experience, were rostered in spinal manipulation (50% pelvic health and 33% orthopaedic and/or for internal pelvic examination (100% pelvic health and 33% orthopaedic PTs) and all had completed at least one orthopaedic level. It was not indicated if any of these PT had survey development experience. These participants were prompted to report any wording or technical issues. The term “perinatal” was identified as an unfamiliar term and was removed from the survey. Incomplete submissions were considered withdrawals from the study.
Recruitment and data collection
Recruitment emails occurred through professional web-based platforms from January-May 2017 sent by the Ontario and Canadian Physiotherapy Associations (Women’s Health, Orthopaedic, and Private Practice) and Pelvic Health Solutions. The research team attempted to apply principles of the Dillman method for recruitment [19] but were not in control as to when the associations distributed the emails. Response rate could not be determined as PTs could hold multiple memberships to the divisions. The research team followed up with incomplete responses. All data were collected via SurveyMonkey® and exported into an excel file on a password protected computer.
Data Analysis
Only complete submissions were analyzed on a separate Excel sheet. Participant’s names were changed to initials and all identifiers were removed. Multiple-choice answers were coded accordingly. Descriptive statistics and statistical analysis were completed. Due to the sample size, the Fisher’s exact method was used to assess significance between the two groups. Only topics that were addressed in congruence with current CPGs were statistically analyzed.
Seventy-eight participants responded to the survey and 44 completed the survey. Refer to Figure 1 for a summary of all results inclusive of associated statistical analysis.
Study sample
For full demographic characteristics refer to Table 1.
Table 1: Demographic Information.
Characteristics |
No. of
Participants (%) |
No. of Pelvic Health
PT (%) |
No. of Orthopaedic
PT (%) |
N = 44 |
44 (100%) |
31 (70%) |
14 (30%) |
Years of Practice |
|
|
|
1-5 years |
14 (32%) |
11 (35%) |
3 (23%) |
6-10 years |
12 (27%) |
7 (23%) |
5 (38%) |
11+ years |
18 (41%) |
13 (42%) |
5 (38%) |
Highest Level of Physiotherapy Education |
|
|
|
Bachelors |
16 (37%) |
11 (36%) |
5 (38%) |
Masters |
27 (61%) |
19 (61%) |
8 (62%) |
Doctorate |
1 (2%) |
1 (3%) |
0 (0%) |
Rostered to perform Spinal Manipulation |
|
|
|
Yes |
17 (39%) |
10 (32%) |
7 (54%) |
No |
27 (61%) |
21 (68%) |
6 (46%) |
Rostered to perform Internal Pelvic Exams |
|
|
|
Yes |
31 (70%) |
31 (100%) |
0 (0%) |
No |
13 (30%) |
0 (0%) |
13 (100%) |
Orthopaedic Levels |
|
|
|
Yes |
32 (73%) |
22 (71%) |
10 (77%) |
No |
12 (27%) |
9 (29%) |
3 (23%) |
FCAMPT Certification |
8 (18%) |
3 (10%) |
5 (38%) |
Knowledge of risk factors
A clinical vignette was used to assess knowledge related to PPGP risk factors. Fifty-five percent of participants correctly ranked the scenarios, with 55% of pelvic health and 54% of orthopaedic PTs ranking them correctly. When prompted about risk factors for PPGP, 89% of participants identified history of low back pain as a risk factor (90% of pelvic health and 85% of orthopaedic). Fifty-seven percent of PTs correctly identified age as not a risk factor, with a statistically significant difference (p=0.04) between pelvic health (68%) and orthopaedic PTs
(31%). Use of contraceptives was not a risk factor and 84% of participants answered that correctly of which 84% were pelvic health and 85% were orthopaedic PTs. This difference was not statistically significant.
Knowledge of assessment strategies
To assess the sacroiliac joint, the majority of PTs chose assessment of the dorsal ligament (pelvic health 74%, orthopaedic 92%) and the Posterior Pelvic Pain Provocation Test (pelvic health 94% and orthopaedic 100%) and also chose the Patrick’s Faber test at a similar rate (87% and 85%). While 52% of pelvic health and 31% orthopaedic PTs chose to use Gaeslsen’s test. The majority of PTs chose the Active Straight Leg Raise (100% pelvic health and 92% of orthopaedic PTs) and Stork Test (pelvic health 61% and orthopaedic 92%) to assess pelvic girdle function. Forty-eight percent of pelvic health and 85% of orthopaedic PTs stated they would use the Standing ASIS Asymmetry Test. Ninety-four percent of pelvic health and 100% of orthopaedic PTs stated they would palpate the pubic symphysis for assessment. The Modified Trendelenburg’s Test was chosen by 26% of pelvic health and 31% of orthopaedic PTs. A similar rate of pelvic health and orthopaedic PTs selected Resisted Hip Abduction (65% and 69%) respectively.
Specific outcome measures were selected based on their prevalence in the literature. The Quebec Back Pain Disability Scale was rarely chosen by both groups (pelvic health 3% and orthopaedic PTs 0%) while 35% of pelvic health and 38% of orthopaedic PTs would use the Oswestry Low Back Pain Questionnaire. Sixteen percent of pelvic health and 23% of orthopaedic PTs selected the Disability Rating Index as an outcome measure. A similar rate of pelvic health and orthopaedic PTs (10% and 8%) stated using no outcome measures. The majority of clinicians (95%) did not believe any imaging techniques would assist with the diagnosis of pelvic girdle pain.
Knowledge of evidence-based treatment strategies
Only 11% of participants identified acupuncture as a possible treatment for PPGP and 39% chose manipulations and joint mobilizations. There was no statistically significant difference between pelvic health and orthopaedic PTs for either acupuncture or manipulations and joint mobilizations.
Knowledge of best practice guidelines
There was a statistically significant difference (p=0.04) in the familiarity of PPGP CPGs between pelvic health (74%) and orthopaedic PTs (38.5%). The majority of pelvic health (81%) and orthopaedic PTs (77%) correctly identified PPGP as an abnormal effect of pregnancy and 61% of pelvic health PTs correctly identified that PPGP differs from low back pain in its history; while 69% of orthopaedic PTs felt they were similar. The majority of PTs (pelvic health 81% and orthopaedic 62%) correctly disagreed with pubic symphysis injury as a cause of PPGP, while 80% of participants identified that PPGP is a complex disorder (81% of pelvic health and 77% orthopaedic PTs). In respect to the use of the terms stability and instability with PPGP, 77% of pelvic health and 38% of orthopaedic PTs correctly disagreed with the use of these teams.
There was no significant difference between groups for the following items: central pain mechanisms, SIJ provocation tests (Q31), and role of connective tissue. Most participants (93%) correctly identified that central pain mechanisms can be a feature of PPGP. Eighty-six percent of participants correctly agreed that >3 positive provocation tests indicates SIJ pain (90% pelvic health and 77% orthopaedic PTs). Seventy-seven percent of participants correctly identified the role connective tissue plays in PPGP.
Current level of knowledge
Participants demonstrated to have moderate knowledge of management strategies of PPGP and limited awareness and utilization of CPGs in clinical practice. The lack of awareness of risk factors for PPGP, as demonstrated by the results for Q10, could be due to the common misconception of increased body mass index as a risk factor [1], as research tends to include participants with both low back pain and PPGP [3,14]. Studies assessing risk factors for PPGP alone have not found BMI to be a risk factor [1]. Mounting literature supports the notion that clinicians should avoid language that can perpetuate fear of movement when caring for individuals experiencing persistent pain [5]. In our study, a higher proportion of pelvic health PTs identified avoiding terms such as ‘instability’ and
‘stability’(Q29) terms when describing PPGP. O’Sullivan and Beales (2007) proposed a biopsychosocial framework specific to PGP and highlighted the need to move away from the term stability [5]. These terms have been noted to potentially further amplify central pain mechanisms [5], contribute to pain persistence, lead to a decreased quality of life and increased healthcare utilization [5,8].
Commented [A1]: This was a significant difference (p=0.018)
Commented [A2R1]: yes
Use of clinical practice guidelines and evidence-based practice
Although the Essential Competency Profile for Canadian Physiotherapists indicates Scholarly Practitioner as one of (how many?) competencies (need reference), we found that only 1/3 of participants reported that their workplace encourages use of CPGs (Q34), and expect them to engage in evidence-based practice (EBP) [20]. Research suggests PTs use EBP more frequently than other health professionals, but PTs do not consistently implement it [21]. Scurlock-Evans et al. found only 69% of PTs reported they read relevant research, and only 26% of these PTs critically appraised it [21].
Our findings are corroborated by the literature highlighting the fact that participants’ lack of awareness of CPGs related to PPGP may affect clinical decision making and EBP [22]. As hypothesized, pelvic health PTs demonstrated greater level of awareness of these CPGs that was statistically significant. This may be due to the postgraduate training pelvic health PTs receive that may include CPGs education. However, this knowledge did not translate into their clinical decision making in this study. Lack of awareness and/or implementation of CPGs could lead to PTs providing treatment not consistent with CPGs [22]. Over half of the participants reported providing manipulations and joint mobilizations, even though evidence is low for the PPGP population and is recommended it be used for testing or only a few treatments. It is unknown if PTs are following this recommendation fully [3]. Acupuncture was least selected despite multiple CPGs reporting strong levels of evidence supporting it being effective for PPGP relief [1,3].
Generally, physiotherapists’ adherence to CPGs ranges from 68%-89% depending on the topic [23,24] and PTs use their colleagues as resources more consistently than research [21]. Bridging the gap between PTs’ attitudes towards EBP and its implementation leads to higher adherence rates to CPGs and more effective care with improved physical functioning scores [24]. Evidence has shown that PTs who participate in studies about a specific population/topic have higher levels of adherence to CPGs about that topic [23]. As such a potential outcome that might transpire from this study relates to participants better engaging in care decisions that align with CPGs and current best practices.
Barriers at the practice level have been found to hinder the implementation of EBP by PTs [21]. Some researchers have identified barriers are: lack of time to dedicate to researching current literature, lack of computer access to databases, and lack of knowledge in application of recommendations [21,25]. These practice level barriers may explain some of the varience related to the discrepancy in awareness of PPGP CPGs and implementation of CPGs by pelvic health PTs, found in this study. Working towards eliminating these barriers, it could increase PTs’
confidence in applying CPGs and promote consistent engagement in CPGs in the future [26].
Clinical decision making
The aim of CPGs are to support clinical decision-making by streamlining and grading the evidence such to facilitate integration into practice [27]. Despite the emerging understanding of the multifactorial nature of pregnancy-related PGP and the need to consider this clinical issue from a biopsychosocial perspective, all described assessment strategies in this study were biomedical and biomechanical in nature. In the most recent published CPGs for pregnancy related PGP, Clinton and colleagues (2016) indicate patient reported outcomes as an important way to capture the various assessment domains relevant to pregnancy-related PGP [3]. Specifically, the Oswestry Disability Index (ODI), the Pelvic Girdle Questionnaire (PGQ) and the Pain Catastrophizing Scale (PCS) are recommended. None of our participants described using these measures. Physiotherapists’ potential lack of awareness and/or translation of current best practices may lead to the use of treatment that is not evidence based and thus not effective. Often decision makers in healthcare fail to consistently use research to inform their decisions [28,29]. This provides further incentive to promote continued postgraduate education and learning to translate knowledge into clinical practice.
The completion rate was 71% however due to the inclusion criteria, only 55% of responses were included. The authors chose to restrict participation to Ontario PTs as the College of Physiotherapists of Ontario’s public registry indicated that there were 759 PTs rostered to perform internal examinations and 1613 orthopaedic PTs rostered for spinal manipulations thus this would be a sufficient pool of PTs for recruitment. The authors were able to ensure that no participants were from outside Ontario by asking for their postal codes upon initialling the survey. The Dillman method could not be fully followed due to Canadian Physiotherapy Association Division’s distribution email restrictions. The hypothesis could not be confirmed due to the small sample size and the uneven distribution of pelvic health and orthopaedic PTs. It was difficult to determine in the participants’ years of clinical practice, how many of these were in the area of PPGP as this could be factor in their knowledge base and use of CPGs in this area. It is also unknown if the two groups were significantly different, pelvic health PT range dramatically in education from the postgraduate courses to University certifications which increases the challenge to compare group as a whole.
There is a discrepancy between the current best practice recommendations related to and the clinical decisions made by Ontario PTs that participated in this study. Most PTs were not familiar with the guidelines, but even those who were, tended to use management strategies that were biomechanically focused and minimally congruent with current best practice. Importantly, both groups of participants (orthopaedic PTs and pelvic PTs) agreed that CPGs use is associated with enhanced patient care. As such, an opportunity exists to address this gap in knowledge
translation in physiotherapy management of PPGP.
Pain science is evolving such that many of the traditional therapeutic biomechanical approaches are being challenged and being addressed by a “much simpler, congruent with the cognitive, neuroscience approach and best evidenced based practice” [30,31]. Future PPGPs CPGs will need to consider and incorporate this into their recommendations. Implementation of PPGP CPGs is quite a conundrum as it is dependent on clinicians being aware, and then they may need to change their practice. They may not if it supports the CPGs, but they will be basing their clinical treatment plan on sound evidence based practice. Making clinicians aware of the CPGs can occur in several ways including both at the entry-level physiotherapy programs and post-graduate physiotherapy courses level. The professional associations also have key role in disseminating the new evidence based information to their members.
A method that may assist with the PPGP CPGs becoming a part of clinical practice is to develop a toolkit that outlines the purpose of the CPGs, its stakeholders, how to implement it, how to overcome any barriers, and how to evaluate its implementation on an ongoing basis [30].
The authors would like to thank the Orthopaedic, Private Practice, and Women’s Health Divisions of the Canadian Physiotherapy Association, as well as Pelvic Health Solutions, and the Ontario Physiotherapy Association for the recruitment of participants. The authors sincerely thank the PTs who participated in the study. The authors declare no conflict of interest.
View supplementary data
- Vleeming A, Albert HB, Ostgaard HC, Sturesson B, Stuge B (2008) European guidelines for the diagnosis and treatment of pelvic girdle pain. Eur Spine J 17: 794-819. [Crossref]
- Wu WH, Meijer OG, Uegaki K, Mens JM, Van Dieen JH, et al. (2004) Pregnancy-related pelvic girdle pain (PPP), I: Terminology, clinical presentation, and prevalence. Eur Spine J 13: 575-589. [Crossref]
- Clinton S, Newell A, Downey P, Ferreira K (2016) Pelvic Girdle Pain in the Antepartum Population: Physical Therapy Clinical Practice Guidelines Linked to the International Classification of Functioning, Disability, and Health from the Section on Women’s Health and the Orthopaedic Section of the American Physical Therapy Association.
- Stuge B (2012) Pelvic girdle pain: examination, treatment, and the development and implementation of the European guidelines. Journal of the Association of Chartered Physiotherapists in Women’s Health. Autumn 111: 5-12.
- O’Sullivan PB, Beales DJ (2007) Diagnosis and classification of pelvic girdle pain disorders—Part 1: A mechanism based approach within a biopsychosocial framework. Man Ther 12: 86-97. [Crossref]
- Fitzgerald CM, Santos LR, Mallinson T (2012) The association between pelvic girdle pain and urinary incontinence among pregnant women in the second trimester. Int J Gynaecol Obstet 117: 248-250. [Crossref]
- Fitzgerald CM, Mallinson T (2012) The association between pelvic girdle pain and pelvic floor muscle function in pregnancy. Int Urogynecol J 23: 893-898. [Crossref]
- 8 Bergström C, Persson M, Mogren I (2016) Sick leave and healthcare utilisation in women reporting pregnancy related low back pain and/or pelvic girdle pain at 14 months postpartum. Chiropr Man Therap 24: 7-18.
- Brown A, Johnston R (2013) Maternal experience of musculoskeletal pain during pregnancy and birth outcomes: significance of lower back and pelvic pain. Midwifery 29: 1346-1351. [Crossref]
- Bjelland EK, Stuge B, Engdahl B, Eberhard-Gran M (2013) The effect of emotional distress on persistent pelvic girdle pain after delivery: a longitudinal population study. BJOG 120: 32-40. [Crossref]
- Gutke A, Josefsson A, Oberg B (2007) Pelvic girdle pain and lumbar pain in relation to postpartum depressive symptoms. Spine (Phila Pa 1976) 32: 1430-1436. [Crossref]
- Wu WH, Meijer OG, Bruijn SM, Hu H, van Dieën JH, et al. (2008) Gait in pregnancy-related pelvic girdle pain: amplitudes, timing, and coordination of horizontal trunk rotations. Eur Spine J 17: 1160-1169. [Crossref]
- Brynhildsen J, Hansson Å, Persson A, Hammar M (1998) Follow-up of patients with low back pain during pregnancy. Obstet Gynecol 91: 182-186. [Pubmed]
- Institute of Obstetricians and Gynaecologists Royal College of Physicians of Ireland (2012) Clinical Practice Guideline Management of Pelvic Girdle Pain in Pregnancy and Post- Partum. Chartered Physiotherapists Women’s Health and Continence and Directorate of Strategy and Clinical Programmes Health Service Executive.
- Kanakaris NK, Roberts CS, Giannoudis PV (2011) Pregnancy-related pelvic girdle pain: an update. BMC Med 9: 15. [Crossref]
- Chartered Society of Physiotherapists: Pelvic Obstetric and Gynaecological Physiotherapy (2015) Guidance for Health Professionals: Pregnancy-related Pelvic Girdle Pain.
- Bury TJ, Stokes EK (2013) A global view of direct access and patient self-referral to physical therapy: implications for the profession. Phys Ther 93: 449-459. [Crossref]
- College of Physiotherapists of Ontario (2017) Controlled Acts and Other Restricted Activities. http://www.collegept.org/standards/controlled_Acts
- Meade D, Patel A, Rogovsky V, Dufour S, Daniel S (2016) Pregnancy-Related Pelvic Girdle Pain: Understanding Clinical Decision-Making [homepage on the internet] School of Rehabilitation Science MSc(PT) Program Research & Evidence Based Practice. https://srs-mcmaster.ca/wpcontent/uploads/2016/09/REBP-Abstract-Booklet-2016.pdf
- Millar MM, Dillman DA (2011) Improving response to web and mixed-mode surveys. Public Opin Q 75: 249-269.
- Essential Competency Profile for Physiotherapists in Canada, October 2009.
- Scurlock-Evans L, Upton P, Upton D (2014) Evidence-based practice in physiotherapy: a systematic review of barriers, enablers and interventions. Physiotherapy 100: 208-219.
- Beales D, Hope JB, Hoff TS, Sandvik H, Wergeland O, et al. (2015) Current practice in management of pelvic girdle pain amongst physiotherapists in Norway and Australia. Man Ther 20: 109-116. [Crossref]
- Armantrout EA, Hummel-Berry K, Underwood F, Nelson C (2008) Physical therapist compliance with electromyography guidelines. J Neurol Phys Ther 32: 177-185. [Crossref]
- Rutten GM, Degen S, Hendriks EJ, Braspenning JC, Harting J, et al. (2010) Adherence to clinical practice guidelines for low back pain in physical therapy: do patients benefit? Phys Ther 90: 1111-1122. [Crossref]
- Côté AM, Durand MJ, Tousignant M, Poitras S (2009) Physiotherapists and use of low back pain guidelines: a qualitative study of the barriers and facilitators. J Occup Rehabil 19: 94-105. [Crossref]
- Smart K, Doody C (2007) The clinical reasoning of pain by experienced musculoskeletal physiotherapists. Man Ther 12: 40-49. [Crossref]
- Alonso-Coello P, Oxman AD, Moberg J, Brignardello-Petersen R, Akl EA, et al. (2016) GRADE Evidence to Decision (EtD) frameworks: a systematic and transparent approach to making well informed healthcare choices. 2: Clinical practice guidelines. BMJ 353: 1-9. [Crossref]
- Straus SE, Tetroe JM, Graham ID (2011) Knowledge translation is the use of knowledge in health care decision making. J Clin Epidemiol 64: 6-10. [Crossref]
- Greg Lehman- Reconciling Biomechanics with Pain Science. 2017[cited 23 August 2017]. Available from: http://www.greglehman.ca/
- RNAO-Toolkit of Implementation of Best Practice Guidelines. 2012[cited 23 August 2017]. Available from: http://rnao.ca/sites/rnaoca/files/RNAO_ToolKit_2012_rev4_FA.pdf
Article Type
Research Article
Publication history
Received date: February 05, 2018
Accepted date: February 28, 2018
Published date: March 05, 2018
Copyright
© 2018 Dufour S. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Citation
Dufour S (2018) Pregnancy-related pelvic girdle pain: understanding practice patterns and clinical decision making. Front Womens Health 3: DOI: 10.15761/FWH.1000137