Abstract
Introduction: transfusion-associated infections mainly caused by bacteria or virus among blood donors are of concern to public health. Blood transfusion practices around the world emphasize safety and the protection of human life.
Objectives: the aim of this study, is to identify positive serology for syphilis in blood donors.
Methodology: A retrospective descriptive study of prevalence was made. We analyzed the database of records of blood donors, screened from 2011 to 2016, with positive syphilis serologies. The demographic data was recorded and analyzed using SPSS software, version 22.0.
Results: out of a total of 2734 donors, 436 (20%) had positive syphilis serology. The majority (88%) 384 were men and 52 (12%) women. Ages ranged between 18 and 64 years, with an average of 31.95 ± 8.9.
Conclusion: in this study, a seroprevalence rate of 20% was observed for positive syphilis serology, which means the impact of the disease on donors is high, this suggests that screening should be reinforced.
Key words
Blood Donors, Prevalence, Syphilis, Epidemiology.
Introduction
It is well-known that since historic times, [1-2] due to the significant increase in the number of cases diagnosed, syphilis has been an exceedingly important challenge for public health [3]. The World Health Organization (WHO) [3-5] estimates that approximately one million people are infected daily worldwide by one or more sexually transmitted diseases (STD) and for 2010 they estimated 11 million new cases of syphilis. For 2012 they estimated a 10% increase in the regional and global prevalence in new cases of syphilis for men and women. This situation merits careful consideration as it contributed to an increase in high risk populations [6]. Syphilis is a bacterial infection caused by Treponema pallidum, which is endemic in low income countries and which occurs at lower rates in middle and high-income countries [7]. Apart from its direct morbidity it increases the risk of infection by the Human Immunodeficiency Virus (HIV) and may cause lifelong disease in children born to mothers infected. It is a disease which, if not treated, will progress over the years through a series of clinical states, and may lead to irreversible cardiovascular and neurological complications. A study undertaken in the USA among men who have sex with men, which was published in July 2017, revealed that the diagnosis of cases of syphilis increased from 9% in 2008 to 11% in 2014, mainly among men aged between 25 and 29 (6% -10%) and among black Africans (9%-14%) [8]. In another study carried out in Brazil, the prevalence of syphilis was 6,3% greater among males (7,5%) than among females (4,3%, p < 0,001). Syphilis was associated with the age group 25-34 years, with people with a low level of education and the unmarried persons [9].
In neighboring Mozambique (8%), South Africa [10] showed a decrease in the seroprevalence rate for syphilis among fertile women between 12 and 49 years of age. In 2003 the rate was 8,6% and in 2011 it was 3,8% [11]. In a survey carried out in Sierra Leone, the estimated prevalence ranged between 1,5% and 5,2% based on regional studies [12].
Data from the Angolan Health Ministry estimated new cases of STD in Angola, showing 19%, 18,5% and 13,9% of prevalence of syphilis in the provinces of Luanda, Huíla and Benguela respectively among pregnant women at a pre-natal appointment. However, sex workers in the province of Luanda showed a prevalence of 34,1% (Available at www.ilo.org/public/scielo. Accessed on 27/07/2017 at 12h and 47min).
A 2013 study in Angola/Luanda showed a seropositivity rate for syphilis of 4.6% [13].
A study published in 2015 covering 43 countries in sub-Saharan Africa revealed that countries such as the Democratic Republic of Congo, Nigeria, Ethiopia and Tanzania presented an increased rate for syphilis [14] as did Swaziland, [15] and Uganda [16].
The aim of this study was to analyze seropositivity for syphilis in blood donors.
Methods
This study is a retrospective descriptive prevalence study, analyzing blood donations from donor records for the year 2011 to 2016 at Clínica Girassol, Luanda, Angola.
In order to assess the results, a retrospective study of the donor database was undertaken. The demographic data of the donors was registered, between 2011 and 2016 and 2734 adult blood donors were observed between the ages of 18 and 64. The analysis was carried out using the statistical data analysis program SPSS ® v.22.0 (Statistical Package for the Social Sciences).
Blood and plasma of voluntary donors and their families was collected in the province of Luanda, according to the regulations and norms for the collection of blood. Using appropriate collection tubes, five milliliters (5ml) of blood was taken from each donor, which was kept at the ideal temperature.
The laboratory of the Immunohemotherapy Service is certified by IQNet Certified Management Systems.
* Serology for Syphilis
Screening for the antibody (IgG e IgM) for Treponema pallidum (TP) is undertaken using Kits for Enzyme-linked immunosorbent assay test (ELISA) ARCHITECT plus i1000Sr Abbott. All reactive results were tested twice. If both tests were non-reactive, the initial result was considered negative. Syphilis was tested using the automated method for Treponema pallidum Hemagglutination Assay (TPHA) which, if it was reactive twice, was repeated as confirmation using the manual method for the procedure TPHA and VDRL (Veneral Disease Research Laboratory). The latter is considered more specific, giving the final result. Was considered syphilis when the results of TPHA and VDRL were positive.
Statistical analysis
The categorical variables are described as absolute and relative frequencies, the continuous variables are described through median or standard deviations or from the median and percentiles, according to the symmetry of their distribution. The prevalence of infections was estimated and for each variable of interest and presented as relative frequency (%) with the respective confidence interval at 95%. In order to test hypotheses on the independence of categorical variables, the Chi-square test of independence or Fisher’s exact test was applied, as appropriate.
In all the hypothesis testing a significance level of α = 5% was considered. The analysis was undertaken using the statistical analysis program SPSS® v22.0 (Statistical Package for the Social Sciences).
Ethical considerations
This study had the consent of the Research Ethics Committee of the Institute of Public Health of the Republic of Angola. With regard to confidentiality no names were involved in the data analysis process as only codes were used to identify donors.
Results
From 2734 donors include in the study, 546 had not a record of syphilis in the database and 4 were dubious. A total of 2184 donors were analyzed. The profile of these donors was characterized by the
predominance of the masculine sex, with 1969 (90%). They were all adults aged between 18 to 64 years, with a median age of 32 ± 9 and 98% of the donors had Angolan nationality.
The prevalence of syphilis between 2011 and 2016 was 20.0% [18.3-21.7%]. There were differences between prevalence and age and nationality – (table 1).
Table 1. Prevalence of infection by Treponema pallidum among blood donors.
|
Total |
Syphilis positive |
|
|
|
n |
(%) |
|
z%
[CI 95%] |
p-value |
Género |
|
|
0.103 |
Male |
1969 |
90.0 |
384 |
19.5
[17.8-21.3] |
|
Female |
215 |
10.0 |
52 |
24.2
[18.9-30.3] |
|
Age |
|
|
|
|
<25 |
444 |
20.3 |
40 |
9.0
[6.7-12.0] |
<0.001 |
25-29 |
540 |
24.7 |
64 |
11.2
[9.4-14.9] |
30-34 |
440 |
20.1 |
80 |
18.2
[14.9-22.1] |
35-39 |
314 |
14.4
|
85 |
27.1
[22.5-32.2] |
>40 |
446 |
20.4 |
167 |
37.4
[33.1-42.0] |
Year |
|
|
<0.001 |
2011 |
80 |
3.7 |
5 |
6.3
[2.7-13.8] |
|
2012 |
265 |
12.1 |
109 |
41.1
[35.4-47.1] |
2013 |
321 |
14.7 |
110 |
34.3
[29.3-39.6] |
|
2014 |
351 |
16.1 |
88 |
25.1
[20.8-29.9] |
|
2015 |
430 |
19.7 |
83 |
19.3
[15.8-23.3] |
|
2016 |
737 |
33.7 |
41 |
5.6
[4.1-7.5] |
|
Nationality |
|
|
|
|
0.828 |
Non-Angolan |
52 |
2.3 |
11 |
21.2
[12.2-34.0] |
|
Angolan |
2132 |
97.7 |
425 |
19.9
[18.3-21.7] |
|
Luanda |
1131 |
53.1 |
171 |
15.1
[13.2-17.3] |
< 0.001 |
Other Regions |
1001 |
46.9 |
254 |
25.4
[22.8-28.2] |
Shyphilis |
|
|
|
|
|
Negative |
1748 |
80 |
- |
- |
- |
Positive |
436 |
20.0
[18.3-21.7] |
- |
- |
- |
Luanda, 2011-2016.
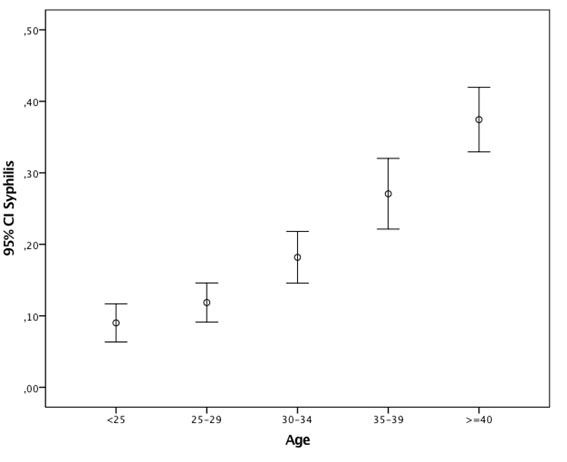
Concerning age, patients with more than 40 years had a higher prevalence than the others 37.4 [33.1 – 42.0] p < 0.001 – (figure 1).
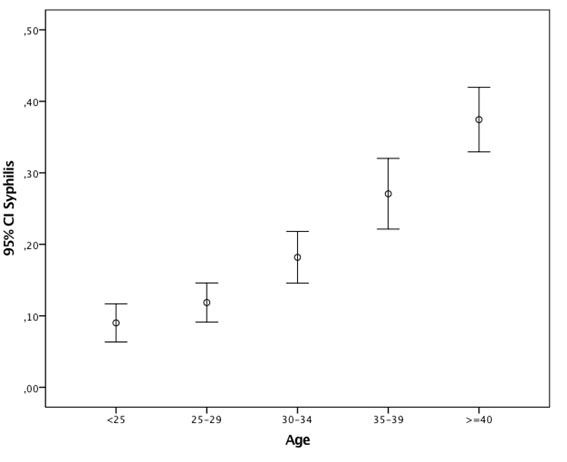
Figure 1. Prevalence of infection by Treponema pallidum among blood donors Age. Luanda, 2011-2016.
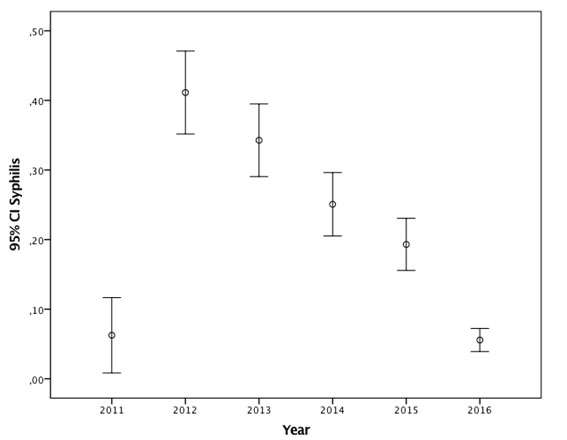
Between 2011 and 2016 the highest prevalence observed was 41.1% [35.4-47.1] in 2012 and the lowest in 2016 with 5.6% [4.1-7.5%]- (figure 2).
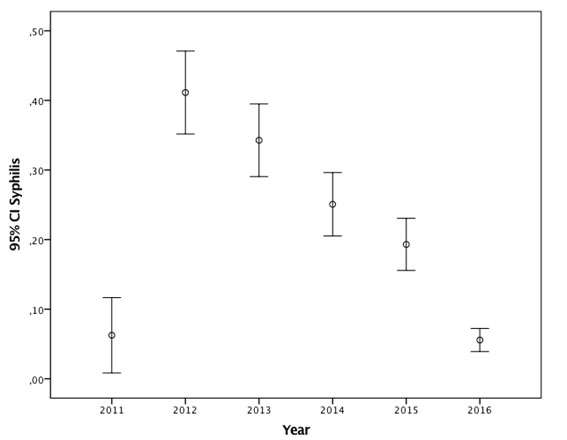
Figure 2. Prevalence of infection by Treponema pallidum among years blood donors. Luanda, 2011-2016.
Discussion
Togo, officially known as The Republic of Togo, an African country bordered to the north by Burkina Faso, to the east by Benin, to the south by the Atlantic Ocean and to the west by Ghana, presents a rate of 2,2% of syphilis among female sex workers, compared to 2,3% for other clients [5]. Countries which border on Angola present a high rate of seroprevalence for syphilis. A study undertaken in 2011 and published in 2014 among women attending pre-natal clinics showed that the Democratic Republic of Congo presented a rate of seroprevalence of 4,2% [17] and among demobilized soldiers it was 3, 4%, with an equal distribution in relation to sex and location [18]. The prevalence of syphilis observed in Zambia was 9,3% [19], 0,4% in Botswana [14].
In a study published in 2014 [20], in comparison with other findings for other countries mentioned above, Namibia presented a low rate of seropositivity for syphilis, with 0,3% of donations positive for the infection. Other study in Ghana who compare laboratory practices for screening blood donors for syphilis estimated that syphilis seroprevalence in voluntary donations was 2.9%, compared to 4.0% in family donations (p = 0.001) [2], [21] when compared to these countries, Angola still maintains high levels of seropositivity for syphilis.
This present study showed that 20% of donations were positive for syphilis, a high rate when compared to neighboring African countries. This decrease in prevalence of Syphilis markers in donors of 2011 to 2016, due to the fact that the Clínica Girassol, makes exclusively service in private patients, which somehow restricts access to most of the population.
Conclusion
In this study it was observed that the prevalence of syphilis continues high in Angola (20%), and that these results do not differ greatly from the estimates suggested by the Angolan Health Ministry from 2003-2008. It is urgent to increase awareness campaigns and to encourage the use of condoms among this key population group and underprivileged classes, to intensify campaigns for the prevention and control of syphilis particularly among populations considered the most vulnerable.
Limitations
Be accomplished only in a private clinic, where not all individuals are able to resort to Financial Institution for screening.
Competing interests
The authors declare that they have no competing interests.
Authors contributions
All the authors participated, read and approved the final manuscript.
Acknowledgements
The authors wish to thank all employees of the Immunohemoterapy Service the Clínica Girassol, that one way or another contributed to the collection of data for statistical analysis.
Websites
- Angolan Health Ministry. Sexual Transmitted Diseases. (Available at www.ilo.org/public/scielo. Accessed on 27/07/2017 at 12h and 47min).
References
- Rovesti M (2017) Between history and gossip: the state of women relative to syphilis, a traditionally male disease. J Biol Regul Homeost Agents. 31: 187-191 [Crossref]
- Sarkodie F (2016) Syphilis screening practices in blood transfusion facilities in Ghana. Int J Infect Dis. 43: 90-94. [Crossref]
- Hook EWR (2017) Syphilis. Lancet 389: 1550-1557.
- Nenoff, P (2017) Non-viral sexually transmitted infections - Epidemiology, clinical manifestations, diagnostics and therapy: Part 1: Gonococci. Hautarzt 68: 43-49.
- Halatoko WA (2017) Prevalence of syphilis among female sex workers and their clients in Togo in 2011. BMC Public Health 17: 219. [Crossref]
- Newman L (2015) Global Estimates of the Prevalence and Incidence of Four Curable Sexually Transmitted Infections in 2012 Based on Systematic Review and Global Reporting. PLoS One 10: 143-304. [Crossref]
- Rimoin AW (2015) HIV infection and risk factors among the armed forces personnel stationed in Kinshasa, Democratic Republic of Congo. Int J STD AIDS 26: 187-195. [Crossref]
- An Q (2017) Syphilis Screening and Diagnosis Among Men Who Have Sex with Men, 2008-2014, 20 U.S. Cities. J Acquir Immune Defic Syndr 75: 63-69. [Crossref]
- Gomes NC (2017) Prevalence and factors associated with syphilis in a Reference Center. Rev Soc Bras Med Trop 50: 27-34. [Crossref]
- Mocumbi S (2017) High HIV prevalence and incidence among women in Southern Mozambique: Evidence from the MDP microbicide feasibility study. PLoS One 12: 173-243. [Crossref]
- Ballah NJ (2017) Decline in syphilis seroprevalence among females of reproductive age in Northern Cape Province, South Africa, 2003-2012: utility of laboratory-based information. Int J STD AIDS 28: 564-572. [Crossref]
- Djibo DA (2017) Prevalence and Risk Factors for Human Immunodeficiency Virus (HIV) and Syphilis Infections Among Military Personnel in Sierra Leone. Curr HIV Res 15: 128-136. [Crossref]
- Guimaraes Nebenzahl H (2013) Prevalence of human immunodeficiency virus, hepatitis C virus, hepatitis B virus and syphilis among individuals attending anonymous testing for HIV in Luanda, Angola. S Afr Med J 103: 186-198. [Crossref]
- Kuznik A (2015) Estimating the Public Health Burden Associated with Adverse Pregnancy Outcomes Resulting from Syphilis Infection Across 43 Countries in Sub-Saharan Africa. Sex Transm Dis 42: 369-375. [Crossref]
- Ginindza TG (2017) Prevalence and risk factors associated with sexually transmitted infections (STIs) among women of reproductive age in Swaziland. Infect Agent Cancer 12: 29. [Crossref]
- Rassjo EB (2006) Prevalence of sexually transmitted infections among adolescents in Kampala, Uganda, and theoretical models for improving syndromic management. J Adolesc Health 38: 213-221. [Crossref]
- Taylor MM (2014) Correlates of syphilis seropositivity and risk for syphilis-associated adverse pregnancy outcomes among women attending antenatal care clinics in the Democratic Republic of Congo. Int J STD AIDS 25: 716-725. [Crossref]
- Senga RK, PM Lutala (2011) High prevalence of syphilis among demobilized child soldiers in Eastern Congo: a cross-sectional study. Confl Health 5: 16. [Crossref]
- Sakala J, N Chizuni, and S Nzala (2016) A study on usefulness of a set of known risk factors in predicting maternal syphilis infections in three districts of Western Province, Zambia. Pan Afr Med J 24: 75. [Crossref]
- Mavenyengwa RT (2014) Prevalence of human immunodeficiency virus, syphilis, hepatitis B and C in blood donations in Namibia. BMC Public Health 14: 424. [Crossref]
- Sarkodie F (2016) A novel strategy for screening blood donors for syphilis at Komfo Anokye Teaching Hospital, Ghana. Transfus Med 26: 63-66. [Crossref]