Abstract
The ambulance transferred patients have a set of physiological parameters i.e., temperature, heart rate, blood pressure (systolic & diastolic), respiratory rate and oxygen saturations (vitals), done on route to the emergency department (ED). The ED triage nurse has to repeat them on arrival, which can delay the initiation of clinical encounter with the physician. It can also impact on the ambulance turnaround time.
We did a retrospective comparative analysis of the two sets of vitals recorded by paramedics and ED triage nurses for 332 patients over a period of 5 months.
There was no significant median difference between the two set of vitals. The mean (SD) difference and P <0.05 were not statistically significant for 4 out the six parameters compared.
The traige and door to doctor time can be significantly decreased, if duplication can be avoided at triage for ambulance transferred patients.
key words
emergency department, triage, blood pressure, heart rate, respiratory rate, oxygen saturations
Introduction
King Faisal Specialist Hospital & Research Center (KFSH & RC) is one the largest tertiary care center in the Saudi Arabia. Its Emergency department (ED) receives a significant number of sick patients transferred via ambulance.
Our paramedics do a series of “vitals” in the pre-hospital phase for patients transferred to ED. These include temperature, heart rate (HR), blood pressure (BP), respiratory rate (RR), pulse oximetry (SpO2). Glasgow coma scale (GCS), blood glucose (BGL), pupil size measurement and twelve lead ECG. End tidal carbon dioxide (EtCO2) monitoring is also carried out.
Vital are repeated in the ED Triage area by the nursing staff. An appropriate clinical examining space is then allocated to the patient. The quicker this process is completed at triage, the faster is the initiation of clinical encounter by the ED physician (“Door to Doctor” time).
The duplication of vital signs by the Triage nurse can add extra time on the patient’s journey within the ED and increase “Door to Doctor time”. This can also have an impact on the ambulance turnaround time.
We intend to compare the two set of patients’ vitals recorded by two differently skilled health care providers to measure any significant difference.
Methods
A convenient sample of all patients transferred to the ED by ambulance over a continuous 5-month period (from July to November 2019) was selected as the study period. We chose vitals like temperature, HR, BP (systolic & diastolic), RR and SpO2 to be compared, as these make a significant component of the Canadian triage system (CTAS), which is used in our ED to allocate a triage category. All patients who had these vitals recorded by paramedics and triage nurses were eligible for the study.
The data gathering process involved collection of manually completed patient care reports (PCR) by the paramedics, which don’t get recorded in the hospital electronic system. The triage vitals carried out by the ED nurses which are electronically recorded were gathered thorough health information technology system (HITA) of the institution.
Medical record numbers (unique patient identifiers) of patients were obtained through HITA, whose mode of transport to ED was ambulance. PCRs of the respective patients were then retrieved.
The data collection was carried out by two authors. One was responsible for gathering information from HITA, whilst the second gathered PCRs. They cross checked the gathered data to avoid any errors. If the PCR showed multiple sets of recorded vitals, the final set was taken for comparison.
An excel sheet was generated where patient’s vitals (Temperature, HR, BP systolic, BP diastolic, RR, SpO2) from both sources were laid side by side for comparative analysis.
We used the hospital statistician to analyze our study data. Descriptive statistics for the continuous variables were reported as mean ± standard deviation and categorical variables summarized as frequencies and percentages. The categorical variables were compared by the Chi-square test and the continuous variables by Student’s independent t-test. The level of statistical significance was set at p < 0.05.
Results
A total 332 patient’s data was gathered within the study period. Only HR and BP (systolic) readings were recorded for all the patients. The BP (diastolic) was recorded in 331(99.6), RR rate in 330 (99.3), SpO2 in 274 (83%) and temperature recorded in 136 (41%) patients. There was missing vitals data in both the triage and ambulance PCR.
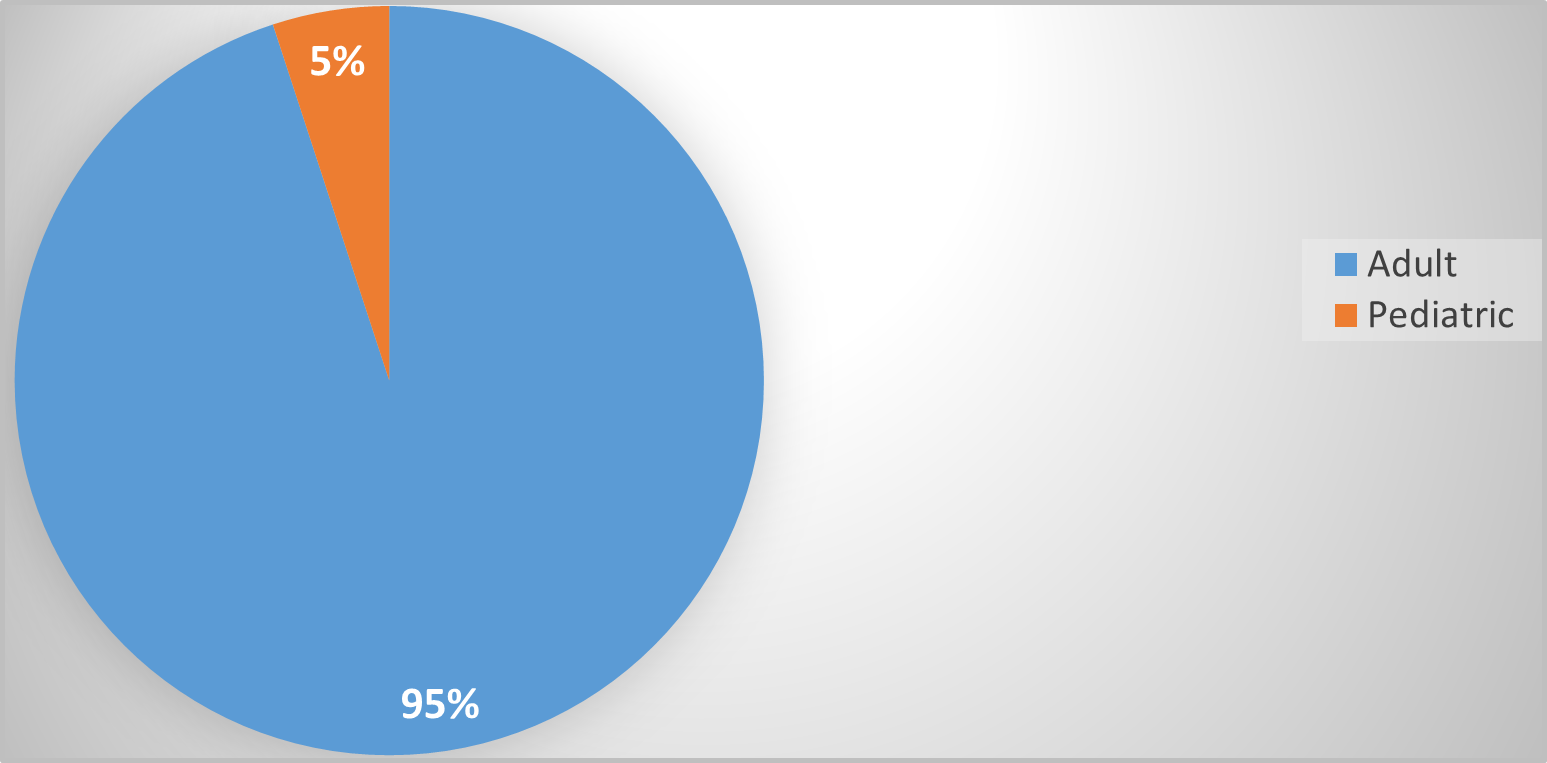
176 (53%) of the study population was male. Adult patients number was 315 (95%). The age range was from 3-97yrs (Figure 1).
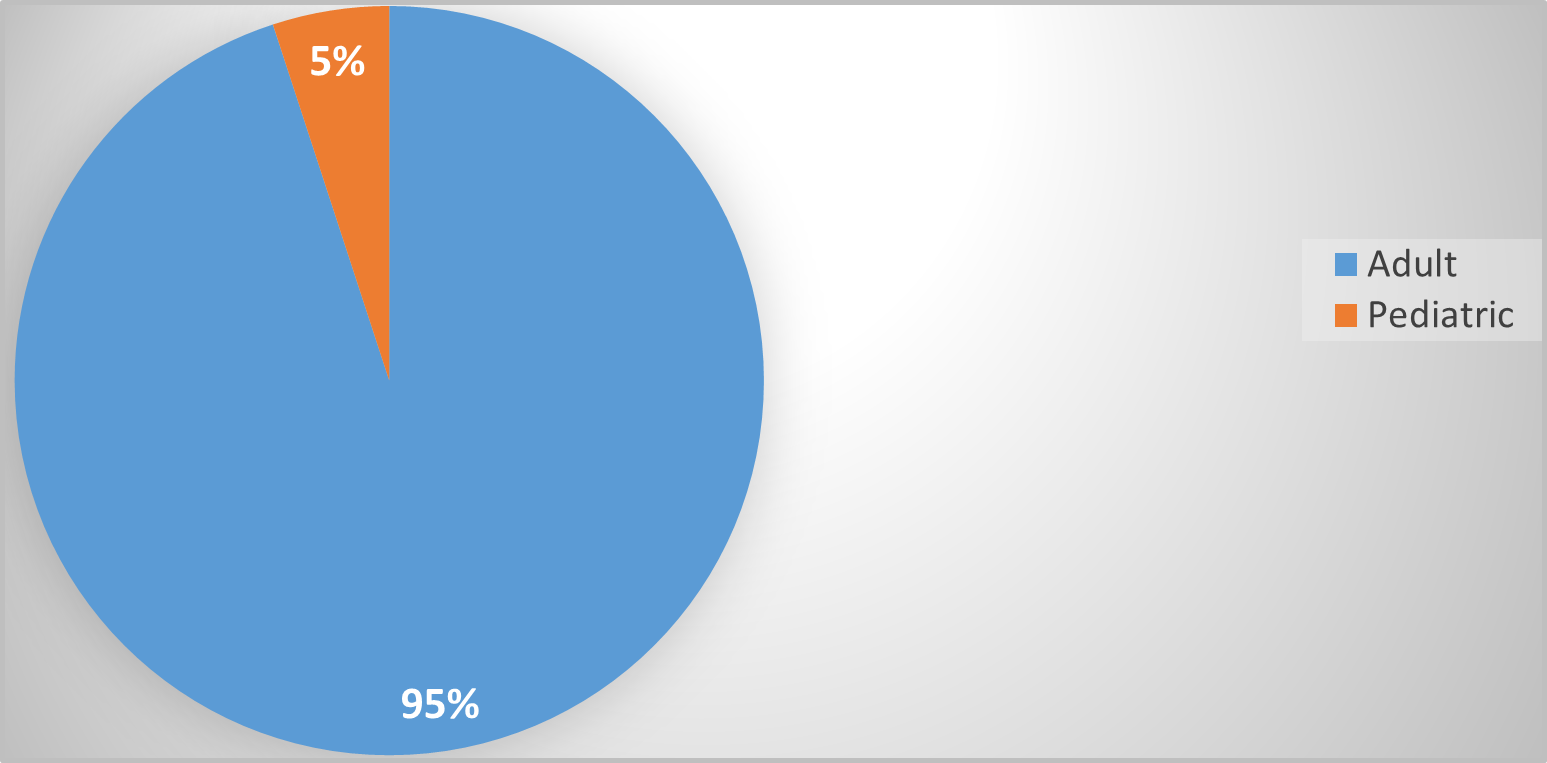
Figure 1. Adult and pediatric patient ratio
209 (63%) were allocated CAT 3, 93 (28%) were triage category CAT 2, 24 (8%) were CAT 4 and 3(1%) were classed as CAT 5&1(2&1). 176(53%) patient came between the morning hours of 0700-1500h, 123 (37%) came between 1500h-2300h and 33 (10%) from 2300h-0700h (Figure 2, Figure 3 and Figure 4).
Figure 2. Gender category
Figure 3. Triage (CTAS) categories
Figure 4. Time segregation
The vital data set included temperature, heart rate, blood pressure (systolic & diastolic), respiratory rate and oxygen saturations.
The median values of the compared data showed no significant statistical difference (Graph 1) but the mean difference was statistically significant for respiratory rates and oxygen saturations only. (Table1 and Graph 2).
Graph 1. Ambulance and triage measures
Graph 2. Mean values.
|
Mean |
SD |
Temperature |
0.03 |
1.09 |
BP (systolic) |
0.95 |
14.96 |
BP (diastolic) |
1.25 |
13.82 |
RR |
1.58 |
5.84 |
HR |
0.07 |
14.88 |
SpO2 |
-0.51 |
2.26 |
The mean (SD) and P levels of the compared vitals are as follows:
Temperature 0.03 (1.09) P>0.47
BP (systolic) 0.95 (14.96) P>0.39
BP (diastolic) 1.25 (13.82) P>0.84
RR 1.58 (5.84) P<0.00
HR 0.07 (14.88) P>0.90
SpO2 -0.51 (2.26) P<0.00
Discussion
Our study was carried out in a big tertiary hospital setting and compared 332 patients, which has never been reported before. Our ED patients are generally sicker with increased clinical complexity as compared to a standard ED setting. Despite this complex cohort, the vitals recorded in the prehospital setting and ED triage were statistically comparable.
ED attendances have consistently increased worldwide and strategies are being adopted to expedite patients’ disposition [1-3]. Our results clearly show that duplication of vitals can be avoided in triage, which can save precious time. This can lead to rapid assessment by the physicians and help streamline patient flow. Triage time usually averages 15 minutes, which can be reduced significantly by avoiding this duplication. Other factors like patient volume and number of triage personnel can also affect the triage time [4-7]. The delay at triage can have a significant impact on ambulance turnaround times, allocation of an appropriate examining space for the patient and overcrowding at triage [8,9].
The average ambulance journey time can be variable but one set of parameters is definitely carried out by the ambulance personnel [10]. In case of multiple recordings, the final set should be more reflective of the patient’s clinical status prior to triage assessment [11].
The last set of vitals done by the paramedics can be used by triage nurse and electronically recorded on arrival, provided the patients’ clinical condition corroborates with it. In the scenario of patient deterioration during transfer from the ambulance to ED triage, it will be safe to repeat the vitals at triage [12,13].
The training and skill mix of the paramedics does impact on recording of these parameters. Skills rehearsal and joint training of ED nursing & paramedic staff can help enhance skills and bring more confidence in using parameters done by other care providers [14].
The devices used for recording these vitals can be standardized to help maintain consistency. The hospital management can play a role in equipment standardization.
ED triage is a very important step in patient’s journey presenting to the ED. This involves a structured review of patient clinical complaint and allocating a triage category based on their presenting complaints and physiological parameters (vitals). The triage category can expedite patient care based on acuity (lower the CTAS category, quicker the intervention by clinicians) [14,15]. The patient acuity also demands the patient be made ready for clinician’s assessment (door to doctor) as quickly as possible to start important clinical interventions [15].
Our study results are informative and highlights that physiological parameters done by the ambulance team can help reduce the triage time and help expedite patients’ clinical encounter with physicians.
Limitations
Our study is single centered and conducted in a highly specialized tertiary care center. It does not reflect the workflow of a standard ER and the results are not generalizable.
Recommendations
The results can use to modify the handover process between paramedics and triage nurses. It can reduce the clinical encounter time (Door to doctor time) with ED physician. The overall patient’s experience can be improved by decreasing the waiting time for assessment.
References
- Sanjuan-Quiles, Ángela, Hernández-Ramón MDP, Juliá-Sanchis R, García-Aracil N, et al (2019) Handover of patients from prehospital emergency services to emergency departments: A qualitative analysis based on experiences of nurses. Journal of Nursing Care Quality 34:169. [Crossref]
- Báez, Alejandro A, Lane PL, Sorondo B (2003) System compliance with out-of-hospital trauma triage criteria. Journal of Trauma and Acute Care Surgery 54:344-351. [Crossref]
- Bernstein, Steven L, Aronsky D, Duseja R, Epstein S, et al (2009) The effect of emergency department crowding on clinically oriented outcomes. Academic Emergency Medicine 16:1-10. [Crossref]
- Bruijns, Stevan R, Guly HR, Bouamra O, Lecky F, et al (2014) The value of the difference between ED and prehospital vital signs in predicting outcome in trauma. Emergency Medicine Journal 31:579-582. [Crossref]
- Bost, Nerolie, Crilly J, Patterson E, Chaboyer W (2012) Clinical handover of patients arriving by ambulance to a hospital emergency department: A qualitative study. International Emergency Nursing 20:133-141. [Crossref]
- Chen, Liangyou, Reisner AT, Gribok A, Reifman J (2009) Exploration of prehospital vital sign trends for the prediction of trauma outcomes. Prehospital Emergency Care 13:286-294. [Crossref]
- Cooke, William H, Salinas J, Convertino VA, Ludwig DA, et al (2006) Heart rate variability and its association with mortality in prehospital trauma patients. Journal of Trauma and Acute Care Surgery 60:363-370. [Crossref]
- Gausche, Marianne, Henderson DP, Seidel JS (1990) Vital signs as part of the prehospital assessment of the pediatric patient: a survey of paramedics. Annals of Emergency Medicine 19:173-178. [Crossref]
- Hu, Peter, Defouw G, Mackenzie C, Handley C, et al (2006) What is happening to the patient during Pre-Hospital Trauma Care? American Medical Informatics Association 2006:955. [Crossref]
- Jones, Daniel W, Appel LJ, Sheps SG, Roccella EJ, et al (2003) Measuring blood pressure accurately: New and persistent challenges. Jama 289:1027-1030. [Crossref]
- Mackenzie, Colin F, Hu P, Sen A, Dutton R, et al (2008) Automatic pre-hospital vital signs waveform and trend data capture fills quality management, triage and outcome prediction gaps. American Medical Informatics Association 2008:318-322. [Crossref]
- Owen, Christine, Hemmings L, Brown T (2009) Lost in translation: maximizing handover effectiveness between paramedics and receiving staff in the emergency department. Emergency Medicine Australasia 21:102-107. [Crossref]
- Shah, Yousaf, Alinier G, Pillay Y (2016) Clinical handover between paramedics and emergency department staff: SBAR and IMIST-AMBO acronyms. International Paramedic Practice 6:37-44.
- Wood K, Crouch R, Rowland E, Pope C (2015) Clinical handovers between prehospital and hospital staff: literature review. Emergency Medicine Journal 32:577-581. [Crossref]
- Klim, Sharon, Kelly AM, Kerr D, Wood S, et al (2013) Developing a framework for nursing handover in the emergency department: an individualized and systematic approach. Journal of Clinical Nursing 22:2233-2243. [Crossref]