Objective: To map the infectious risk of the management of a hemodialysis patient with Covid-19 during a hemodialysis session in the hemodialysis department of a hospital in Morocco.
Methods: Our study focuses on the analysis of a priori risks during the management of a hemodialysis patient with Covid-19 during a hemodialysis session, carried out from September to November 2020, by applying the Failure Modes and Effects and Criticality Analysis (FMECA) method in the hemodialysis department of the Provincial Hospital Centre (PHC) El Jadida in Morocco.
Results: 18 failure modes were detected during the analysis of infectious risks in a hemodialysis patient with Covid-19 during a hemodialysis session, including 8 failure modes of criticality class C1, 2 failure modes of criticality class C2 and 8 failure modes of criticality class C3. Corrective actions were proposed to deal with the failure modes of criticality class C3.
Discussion: The FMECA method allowed us to identify the most critical failure modes, to prioritize them and to determine corrective actions in order to improve the management of a hemodialysis patient with Covid-19 and consequently to develop the quality and safety of this management.
Conclusion: Risk mapping is an essential tool for continuous quality improvement, the aim of which is to maximize the safety of the patient care process and finally satisfy the population.
Risk mapping, Hemodialysis, Covid-19, infectious risk.
Chronic kidney disease (CKD) is a major public health problem in the world [1,2] leading to a heavy burden of excessive morbidity [3,4] and health care expenses [5]. Hemodialysis is a recent palliative therapeutic management allowing the continuation of life in patients with chronic renal failure [6]. It is a budgetary treatment procedure [7,8] destabilizing the budgetary balances of health systems precisely in developing countries [9].
Hemodialysis is a technique predisposed to infectious risks [10], which constitute the second most common complication after cardiovascular complications [11] and are the second most common cause of mortality in hemodialysis patients [12]. Infectious transmission in hemodialysis goes beyond intra-individual transmission to direct or indirect cross-transmission and manuported transmission [13]. Caregiver-to-caregiver infectious transmission through accidental exposure to blood is a major concern in hemodialysis departments [14] and therefore safety of care in hemodialysis is an essential priority [15].
Among hemodialysis patients, there are patients with increased vital risks who require special care and medical prescriptions in order to maintain their tolerance to hemodialysis sessions [16]. These hemodialysis patients at risk are cardiac, vascular, diabetic, malnourished and elderly patients [16] and therefore the establishment of specific protocols for certain associated pathologies is indispensable [15]. Following the rapid worldwide spread of Covid-19 and its declaration as a pandemic on March 11, 2020 by the WHO [17], its impact on hemodialysis patients in Africa is unknown [18]. In the context of life-threatening hemodialysis patients, caregivers must think about personalizing treatment protocols for these different types of patients [15]. The infectious risk in hemodialysis constitutes a daily constraint that prevents the transmission of the usual pathogenic microorganisms (HB, HC, HIV) and nowadays extends to other poorly known contaminating agents [15] such as the new Covid-19 virus. Hemodialysis patients are a vulnerable population to Covid-19 due to their immunosuppression associated with CKD [18], and therefore the risk of these patients developing a severe form of Covid-19 is estimated to be 9 to 12 times higher [19]. Hemodialysis patients have been shown to be at high risk of developing COVID-19 with a high mortality rate [20]. COVID-19 has a significant impact on patients with chronic renal failure, especially those receiving hemodialysis treatment [21], so urgent adaptation of hemodialysis care is essential [22]. Early detection is crucial for possible control of the spread of the Covid-19 pandemic in the hemodialysis center [23]. Hence the importance of establishing a quality assurance system in hemodialysis centers [10] in this crisis context, which is operationally manifested by several methods, the main one being the analysis of failure modes, their effects and their criticality (FMECA) [10].
The hemodialysis department of the Provincial Hospital Centre of El Jadida has received hemodialysis patients with Covid-19, This had an impact on its internal organization by ensuring, on the one hand, the continuity of hemodialysis services for patients not affected by Covid-19 and, on the other hand, the management of patients affected by Covid-19 by respecting the application of specific protocols in this management with the aim of preventing and minimizing the risks related to the spread of this pandemic in the hemodialysis service.
The objective of our study is to establish a mapping of the infectious risk in a patient suffering from Covid-19 during a hemodialysis session in order to set up preventive and corrective actions, by applying the FMECA method.
This study took place from September to November 2020 at the hemodialysis service of the PHC El Jadida and opted for the methodology of risk analysis a priori. The method applied was the Analysis of Methods of Failure Effects and Criticality (FMECA). The FMECA method is a quality tool based on the inductive approach, it allows to determine the failure modes of a process and to evaluate its importance or criticality [24] even before the problems appear. It therefore aims to classify the risks in order to design an effective prevention plan [24]. The use of the FMECA method in our study was done from a qualitative and quantitative perspective that allowed us to assess the risks and prioritize preventive actions [24].
The operationalization of the FMECA method in our study went through the following steps:
- Description of the process
The FMECA method began with the delimitation of the process of taking care of a patient with the Covid-19 virus during a session of hemodialysis by enumerating all the steps taken by any hemodialysis patient with the Covid-19 virus from the moment of his arrival at the hemodialysis department of the PHC El Jadida until his departure (Figure 1).
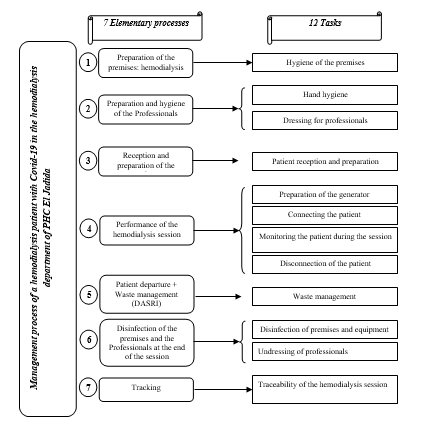
Figure 1. Management process of a hemodialysis patient with Covid-19.
- Process analysis
The analysis of the process was based on the analysis of the failures detected for each step of the process of taking care of these patients, using the Ishikawa Diagram and Brainstorming for a possible determination of the causes of the failures and their effects. This second step was initiated according to the following logic:
Determination of failures
The identification of the risks named failure modes is based on the identification of all the inappropriate actions or errors that may have occurred for each step of the process through Brainstorming.
Identification of causes
The identification of the causes is done through the Ishikawa Diagram for the process of managing a hemodialysis patient with Covid-19 (Figure 2).
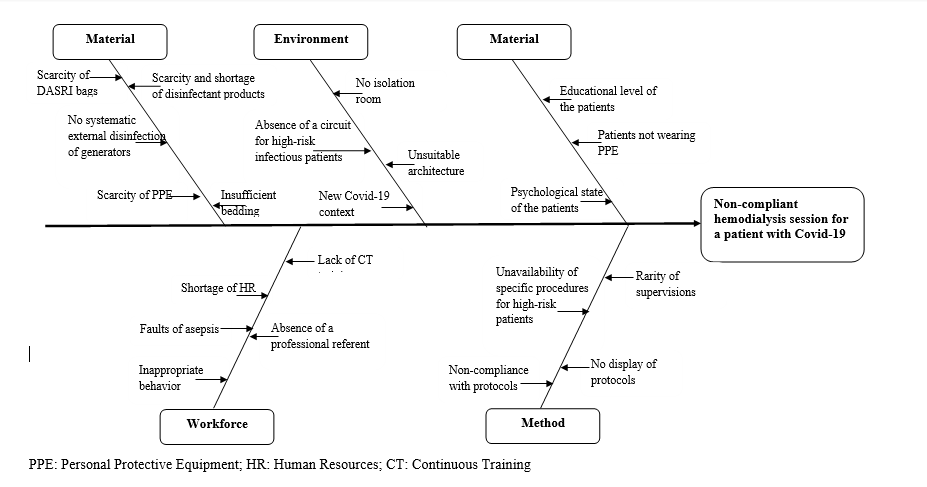
Figure 2: Ishikawa diagram.
- Definition of the possible effects
Then the projection of the consequences and impact of these failures on the management process of hemodialysis patients with Covid-19 virus.
- Risk assessment and prioritization
The risks were rated according to three dimensions (Table 1):
Table 1: Risk Rating Scale.
Frequency |
Score |
Frequency level |
Criteria |
F1 |
1 |
Infrequent |
Failure noted at least once a month |
F2 |
2 |
Somewhat frequent |
Failure noted at least once a week |
F3 |
3 |
Common |
Failure noted once a day |
F4 |
4 |
Very common |
Failure noted more than once a day |
Severity |
Score |
Severity level |
Criteria |
S1 |
1 |
Minor |
Minor incident with no impact |
S2 |
2 |
Moderate |
Incident with temporary injury |
S3 |
3 |
Major |
Incident with impact |
S4 |
4 |
Review |
Serious incident |
Detectability |
Score |
Detectability level |
Criteria |
D1 |
1 |
Very detectable |
Always detectable by observation |
D2 |
2 |
Detectable |
Easily detectable |
D3 |
3 |
Not very detectable |
Difficult to detect |
D4 |
4 |
Not detectable |
Never detectable |
- Frequency (F): How often does this risk occur?
- Severity (S): What is the magnitude of the risk to the patient?
- Detectability (D): How easy or difficult is it to detect the risk?
Each measurement dimension has a rating from 1 to 4 (Table 1) which was used to calculate the criticality (C) from the product of the frequency, severity and detectability C = F*S*D of each failure mode and was illustrated by a criticality decision matrix (Table 2).
Table 2: Criticality Decision Matrix.
|
Severity
|
|
|
Frequency
|
|
1
|
2
|
3
|
4
|
|
Detectability
|
|
1
|
1
|
2
|
3
|
4
|
1
|
|
2
|
4
|
8
|
12
|
16
|
2
|
|
3
|
9
|
18
|
27
|
36
|
3
|
|
4
|
16
|
32
|
48
|
64
|
4
|
The prioritization of risks is always based on the calculation of criticality (C), which allows us to categorize the levels of risk (Table 3):
Table 3: Risk acceptability level.
Criticality class |
Score |
Level of risk |
Actions |
C 1 |
1 à 8 |
Acceptable under control |
Evaluation implemented, effective follow-up |
C 2 |
9 à 16 |
Tolerable under control and must be corrected |
Action to be taken to reduce the risk |
C 3 |
17 à 64 |
Unacceptable to be treated as a priority |
Immediate action to be taken |
- Low criticality: Acceptable under control;
- Moderate criticality: Tolerable under supervision and must be corrected;
- High criticality: Unacceptable and should be treated as a priority.
Finally, the determination of the criticality levels of the different failure modes allowed the elaboration of the risk control plan by prioritizing the implementation of the proposed corrective actions in order to reduce the failures whose criticality is high first, followed by the failures whose criticality is moderate.
The mapping of the infectious risk in a patient with Covid-19 during a hemodialysis session from arrival to departure by applying the FMECA method allowed us to deconstruct the process of managing the hemodialysis patient with Covid-19 into 7 elementary processes containing 12 tasks (Figure 1).
The Ishikawa Diagram identified the causes of the various failures leading to the non-compliant management of the hemodialysis patient with Covid-19 (Figure 2).
The FMECA analysis illustrated 18 failures in the ECP of a Covid-19 patient during a hemodialysis session, including 8 failure modes classified in criticality class C3 (44.44%), 2 failure modes classified in criticality class C2 (11.11%) and 8 failure modes classified in criticality class C1 (44.44%) (Table 4).
Table 4: FMECA analysis.
Elementary process |
Tasks |
Failures |
Causes |
Consequences |
F |
S |
D |
C |
1 |
Hygiene of the premises
|
Inappropriate state of disinfection |
-Scarcity and shortage of disinfecting products;
-Absence of protocols for disinfecting the premises. |
Infectious risks |
3 |
3 |
2 |
18 |
2 |
Hand hygiene
|
Lack of hand hygiene |
-Non-compliance with handwashing protocols;
-Failure to post handwashing protocols. |
Infectious risks
Professional risks |
1 |
3 |
2 |
6 |
Dressing for professionals
|
Dressing techniques |
- Lack of ongoing training;
-No specific protocol developed |
Infectious risks
Professional risks |
3 |
4 |
2 |
24 |
3 |
Patient reception and preparation
|
Poor patient hygiene |
Non-application of hygiene rules by the patient;
Non-use of PPE by patients (surgical mask;
-Dependent patient. |
Infectious risks
Professional risks |
2 |
4 |
2 |
16 |
Poorly maintained bedding material |
-Insufficient Bedding;
-Lack of linen change between two patients Covid-19; |
Infectious risk; Organizational risk. |
2 |
3 |
1 |
6 |
Lack of knowledge of the modes of transmission of Covid-19 |
-New context of the Covid-19 pandemic
- Scarcity of scientific studies |
Infectious risk; Organizational risk
Professional risks |
3 |
3 |
3 |
27 |
Isolation of the uninsured patient |
-Absence of the isolation room
-Lack of appropriate procedures |
4 |
3 |
2 |
24 |
4 |
Preparation of the generator |
External disinfection of the generator (EDG) |
-Failure to develop disinfection procedures;
-Failure to provide ongoing training in this area (EDG) |
Infectious risks
Professional risks |
1 |
3 |
3 |
9
|
Connecting the patient |
Asepsis and safety rules not respected for intravenous fistula (IF) puncture or catheter placement |
Non-application of management protocols ;
-Aseptic errors. |
Infectious risk; |
2 |
4 |
3 |
24 |
Monitoring the patient during the session |
Accidental removal of the catheter |
Insufficient fixation of the catheter |
Risk of infection
Risk of bleeding |
1 |
3 |
2 |
6 |
Improper handling of the line during the session |
Lack of immediate needle removal. |
Infectious risk; |
1 |
2 |
1 |
2 |
Asepsis rules not respected during the session |
Faults of asepsis. |
Infectious risks
Professional risks |
1 |
3 |
1 |
3 |
Disconnection of the patient |
Septic Compression |
Non-sterile dressings |
Infectious risk |
1 |
2 |
1 |
2 |
Inappropriate catheter or fistula dressing |
Asepsis rules not respected |
Infectious risk |
1 |
2 |
1 |
2 |
5 |
Waste management |
Inadequate Waste from Healthcare Activities with Infectious Risks (WHAIR) management |
- Absence of WHAIR bags;
-Absence of a central waste management room in the hemodialysis department; |
Infectious risk |
2 |
3 |
3 |
18 |
6 |
Disinfection of premises and equipment |
-Inappropriate disinfection of premises |
-Inappropriate disinfectant quality;
-Professional not trained in disinfection of premises; |
Infectious risks
Professional risks |
3 |
3 |
3 |
27
|
Undressing of professionals |
- Undressing technique difficult to practice and not mastered |
-Duration of the hemodialysis session;
-Non-compliance with the protocol for undressing after contact with a Covid-19 positive patient |
Infectious risks
Professional risks |
2 |
3 |
3 |
18 |
7 |
Traceability of the hemodialysis session |
Input error |
Workload |
Organizational risk |
1 |
2 |
2 |
4 |
Figure 3 represents the risk map of the complete process of managing a patient with Covid-19 during a hemodialysis session highlighting 7 elementary processes, 12 tasks, 18 failure modes and 3 criticality levels.
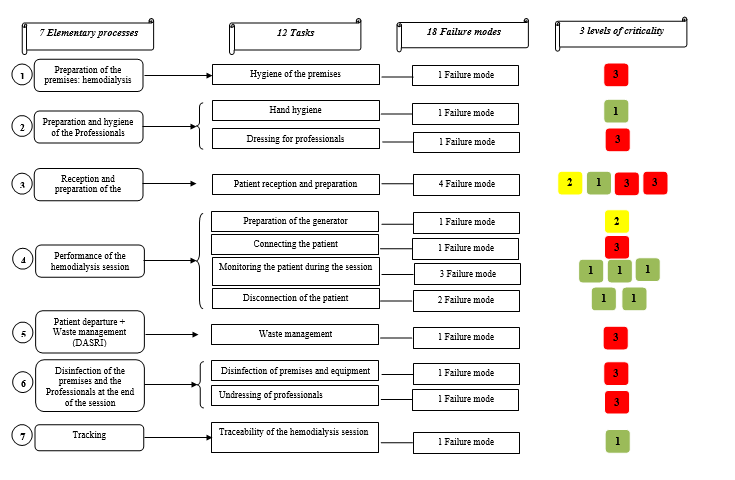
Figure 3: Représentation de la cartographie des risques du processus complet.
The failure modes of criticality level 3 are the object of immediate corrective actions that have been reported in table 5.
Table 5: Corrective actions for criticality level 3 failure modes.
Elementary process |
Tasks |
Failures |
Causes |
Consequences |
F |
G |
D |
C |
Corrective actions |
1 |
Hygiene of the premises
|
Inappropriate state of disinfection |
-Scarcity and shortage of disinfecting products;
-Absence of protocols for disinfecting the premises. |
Infectious risks |
3 |
3 |
2 |
18 |
-Elaboration of disinfection protocol;
-Availability of quality disinfectant products. |
2 |
Dressing for professionals
|
Dressing techniques |
-Lack of ongoing training;
-No specific protocol developed |
Infectious risks
Professional risks |
3 |
4 |
2 |
24 |
-Continuous training for the staff of the department in the management of a Covid-19 patient;
-Elaboration of specific protocols for this management. |
3 |
Patient reception and preparation
|
Lack of knowledge of the modes of transmission of Covid-19 |
-New context of the Covid-19 pandemic;
- Scarcity of scientific studies. |
Infectious risk; Organizational risk
Professional risks |
3 |
3 |
3 |
27 |
-Adaptation of management to the latest scientific developments. |
Isolation of the uninsured patient |
-Absence of the isolation room;
-Lack of appropriate procedures. |
4 |
3 |
2 |
24 |
-Proposal to set up an isolation room in the hemodialysis department.
|
Connecting the patient |
Asepsis and safety rules not respected for IF puncture or catheter placement |
Non-application of management protocols ;
-Aseptic errors. |
Infectious risk; |
2 |
4 |
3 |
24 |
- Updating and application of management protocols;
-Supervision of management activities. |
5 |
Waste management |
Inadequate WHAIR management |
- Absence of WHAIR bags;
-Absence of a central waste management room in the hemodialysis department; |
Infectious risk |
2 |
3 |
3 |
18 |
-Availability of DASRI bags.
-Training of professionals in DASRI management in Covid-19
|
6 |
Disinfection of premises and equipment |
-Inappropriate disinfection of premises |
-Inappropriate disinfectant quality;
-Professional not trained in disinfection of premises; |
Infectious risks
Professional risks |
3 |
3 |
3 |
27
|
-Training of professionals in disinfection;
-The supply of sufficient quantities of quality disinfectants. |
Undressing of professionals |
- Undressing technique difficult to practice and not mastered |
-Duration of the hemodialysis session;
-Non-compliance with the protocol for undressing after contact with a Covid-19 positive patient |
Infectious risks
Professional risks |
2 |
3 |
3 |
18 |
-Continuing education for department staff in the management of a Covid-19 patient. |
The application of the FMECA method in the process of managing a hemodialysis patient with Covid-19 during a hemodialysis session allowed us to map the infectious risk in this patient by highlighting 18 failure modes likely to affect the quality of this management. The evaluation of the degree of risk acceptability highlighted 8 failure modes of unacceptable criticality (C3) which must be treated as a priority.
The FMECA method helped us to determine the different stages of the process of care of a patient with Covid-19 during a hemodialysis session as well as the failures related to any stage of the process based on two components. On the one hand, the qualitative part of the FMECA elucidated the failure modes related to each task in each step of the process by deconstructing the causes through the Ishikawa diagram (Figure 2), and the consequences through brainstorming (Table 4). On the other hand, the quantitative part of this method has counted the criticality of each failure mode by adopting a scale of frequency, severity and detectability (Table 1) in order to categorize the criticality of all failures and then prioritize the corrective actions following this component (Table 5).
The detected failures and their consequences (Table 4) have been categorized into three levels of criticality:
Acceptable risks under control
The FMECA allowed us to identify 8 failure modes with acceptable risks in the different steps of the process of taking care of hemodialysis patients suffering from Covid-19 during a hemodialysis session at low frequency and easily detectable:
The lack of hand hygiene with low frequency resulting in infectious and professional risks;
Poorly stored bedding material, mainly due to the non-availability of bedding linen, leading to the non-change of this linen between two patients (Covid-19);
Accidental removal of the catheter due to inadequate fixation, which leads to hemorrhagic and infectious risks;
Inadequate handling of the line during the session due to the absence of immediate removal of the needle, leading to an infectious risk;
Asepsis rules not respected during the session due to asepsis faults, which can lead to infectious and professional risks;
Septic compression at very low frequency due to the use of non-sterile dressings generating an infectious risk;
Inappropriate dressing of catheters or fistulas due to non-compliance with asepsis rules resulting in the appearance of infectious risks.
All these C1 criticality risks must be controlled so that they do not develop into another criticality level (C2 or C3) and must be managed by training professionals, raising their awareness and standardizing and applying management procedures and protocols.
Tolerable risks under supervision
Two failure modes have been identified for tolerable risks in the different steps of the management process of hemodialysis patients with Covid-19 during a hemodialysis session:
Faulty hygiene of the patient due to the non-application of hygiene rules by the patient, non-use of PPE by the patients, which generates infectious and professional risks;
The external disinfection of the generator (EDG) due to the non-elaboration of disinfection procedure and non-dispensation of continuous training in EDG during the Covid-19 pandemic.
The monitoring of these two failures will be ensured on the one hand by training and information of professionals, and on the other hand by sensitizing patients to hygiene and the use of PPE during the hemodialysis session.
Unacceptable Risks to be Prioritized
Eight failure modes have been identified for unacceptable risks in the different steps of the process of taking care of hemodialysis patients with Covid-19 during a hemodialysis session and which must be treated as a priority given their criticality and their impact:
The state of disinfection of the premises is inappropriate due to the scarcity and shortage of disinfecting products, the absence of protocols for disinfection of the premises during the Covid-19 pandemic, which includes the infectious and professional risk. The corrective actions lie in the elaboration of protocols of disinfection of the premises in the context of Covid-19, in addition to the availability of disinfecting products in quality and sufficient quantity;
The inappropriate dressing and undressing techniques used by professionals during this care due to lack of training, non-development of protocols for these techniques, and finally, the difficulty in implementing these techniques, which results in the propagation of infectious and professional risks. The corrective actions are based on the practical training of the professionals in the management of a Covid-19 patient as well as the elaboration of protocols for this management;
The lack of knowledge of all the modes of transmission of Covid-19 given the new context of the Covid-19 pandemic and the scarcity of scientific studies, which leads to the appearance of infectious risk. Nevertheless, the adaptation of the management to the scientific actuality, to the evidences and to the directives of the Ministry of Health;
The isolation of the patient suffering from Covid-19 is not ensured because of the absence of an isolation room in the hemodialysis department, which facilitates the propagation of the infectious risk. So, the installation of an isolation room remains the most appropriate way to deal with this risk, nevertheless it will take time and in order to act immediately the department has recommended two to three half-days per week dedicated to the care of only those patients with Covid-19 and requiring hemodialysis;
Risk of asepsis and safety not respected for IF puncture or catheter placement due to asepsis and non-application of management protocols, which results in the appearance of infectious risks. In order to cope with this, supervision activities must be organized to ensure rigorous application of management protocols;
Inappropriate Waste from Healthcare Activities with Infectious Risks (WHAIR) management at the end of the hemodialysis session due to the unavailability of WHAIR bags, the absence of a central waste management room in the hemodialysis department, and the absence of WHAIR management training in the Covid-19 context. However, the correction of this risk lies in the training of professionals in the management of WHAIR as well as the adequate supply of WHAIR bags;
Inappropriate disinfection of the premises and equipment at the end of the hemodialysis session of the Covid-19 patient due to the inadequate quality of the disinfectant products and the lack of expertise of the professionals in the department in the area of disinfection of the premises. However, the resolution of this risk lies in the adequate choice of the quality of the disinfectants that meet the need and the organization of practical workshops on disinfection of the premises for the benefit of the professionals of the hemodialysis service.
The method of risk analysis FMECA is an essential tool in the detection a priori of risks that can affect the process of taking care of a patient with Covid-19 during a session of hemodialysis by making a risk map whose goal is to improve the safety of the patient during this care and consequently to improve the quality of care and satisfy the population. Nevertheless, this method illustrates certain limitations, particularly the choice of failures and the rating of criticality, which depended on the work team.
- Liyanage T, Ninomiya T, Jha V, Neal B, Patrice HM, et al. (2015) Worldwide access to treatment for end-stage kidney disease: a systematic review. Lancet 385: 1975-1982. [Crossref]
- Pippias M, Stel VS, Abad Diez JM, Afentakis N, Herrero-Calvo JA, et al. (2015) Renal replacement therapy in Europe: a summary of the 2012 ERA-EDTA Registry Annual Report. Clin Kidney J 8: 248-261. [Crossref]
- Arulkumaran N, Annear NM, Singer M (2013) Patients with end-stage renal disease admitted to the intensive care unit: systematic review. Br J Anaesth 110: 13-20. [Crossref]
- Cheng X, Nayyar S, Wang M, Li X, Sun Y, et al. (2013) Mortality rates among prevalent hemodialysis patients in Beijing: a comparison with USRDS data. Nephrol Dial Transplant 28: 724-732. [Crossref]
- Divajeva D, Marsh T, Logstrup S, Kestens M, Vemer P, et al. (2014) Economics of chronic diseases protocol: cost-effectiveness modelling and the future burden of non-communicable disease in Europe. BMC Public Health 14: 456. [Crossref]
- Elisabeth Hermès, Lynda Sifer (2005) LE PROCESSUS IDENTITAIRE DES PATIENTS EN HÉMODIALYSE : L'IMPACT DE LA TECHNIQUE SUR LA TRAJECTOIRE DE VIE. 2005/2 N° 81 | pages 56 à 77.
- Coentrao L (2013) Costs and outcomes of endovascular treatment of thrombosed dialysis autogenous fistulae. Nefrologia 33: 470-477. [Crossref]
- Just PM, de Charro FT, Tschosik EA, Noe LL, Bhattacharyya SK, et al. (2008) Reimbursement and economic factors influencing dialysis modality choice around the world. Nephrol Dial Transplant 23: 2365-2373. [Crossref]
- Asserraji M, Maoujoud O, Belarbi M, Oualim Z (2015) Profil épidémiologique de l’insuffisance rénale terminale a` l’hôpital Militaire de Rabat, Maroc. Pan Afr Med J 20: 439. [Crossref]
- Marnissi S, Khomsi Z, Sylvestre ALR, El Harti J, Taoufik J, et al. (2020) Analyse du risque infectieux autour du patient dans l’unité d’hémodialyse de l’hôpital Ibn Sina de Rabat par application de la méthode d’analyse des modes de défaillance, de leurs effets et de leur criticité. Nephrol Ther 16: 105-117. [Crossref]
- Grenêche S, D’Andon A, Jacquelinet C, Faller B, Fouque D, et al. (2005) Le choix entre dialyse péritonéale et hémodialyse : une revue critique de la littérature. Nephrol Ther 1: 213-220.
- Mekouar S, Mekouarsofia-aimad (2011) Les infections chez les hémodialysés et facteurs de risque. Néphrologie, CHU Ibn rochd, Casablanca, Maroc. Dialyse/ Néphrologie & Thérapeutique 7: 301-343.
- Société française d’hygiène hospitalière (SFHH) (2005) Recommandations de la SFHH. Bonnes pratiques d’hygiène en hémodialyse. Hygiènes 13: 2.
- Litchinko MB. Analyse des risques d’exposition au sang en hémodialyse : Prévention et recommandations. Néphrologie-Hémodialyse Clinique médicale et pédagogique Edouard Rist – PARIS.
- Canaud B (2000) Contrôle de qualité en hémodialyse : Démarche assurance qualité. Néphrologie et Institut de recherche et formation en dialyse, CHRU Hôpital Lapeyronie, Montpellier. Néphrologie 21: 403-411.
- Pollak VE, Pesce A, Kant KS (1992) Continuous quality improvement in chronicdisease : A computerized medical record enables description of a severity index to evaluate outcomes in end-stage renal disease. Am J Kidney Dis 19: 514-522. [Crossref]
- Bracey T, Arif S, Ralte AR, Shaaban AM, Ganesan R, et al. (2021) Histopathology during the COVID-19 pandemic: resilience through adaptation and innovation. Diagn Histopathol (Oxf) 27: 108-115. [Crossref]
- Ebana HDFME, Halle M, Onana CM, Mbatchou BH, Namme HL, et al. (2021) Epidemiologic and clinical profile, 90 days survival of incident end stage renal patient in haemodialysis during SARS-CoV2 pandemic: Experience of the General Hospital of Douala. Nephrol Ther 17: 226-232. [Crossref]
- CDC Covid-19 Response Team. (2020) Preliminary estimates of the prevalence of selected underlying health conditions among patients with coronavirus disease 2019 – United States, February 12–March 28, 2020. MMWR Morb Mortal Wkly Rep 69: 382-386. [Crossref]
- Keller N, Chantrel F, Krummel T, Bazin-Kara D, Faller AL, et al. (2020) Impact of first-wave COVID-19 infection in patients on haemoDIALysis in Alsace. The observational COVIDIAL study. Néphrologie & Thérapeutique 16: 324-325.
- Almonte K, Weiner DE (2020) COVID-19 universal testing in hemodialysis facility to reduce infection risk. Kidney Med 2: 681-683. [Crossref]
- Guerraoui A, Idier L, Azzouz L,Pelletier S, Bouiller M, et al. (2020) Les soignants en dialyse face à la crise sanitaire (COVID-19) : quels risques pour leur santé mentale ? Étude PsyCoviDial. Nephrol Ther 16: 278. [Crossref]
- Collart F, Salaouatchi T, Clevenbergh P, Maillart E, Mahadeb et B (2020) Dépistage systématique par culture virale des patients COVID en hémodialyse. Nephrol Ther 16: 275-276. [Crossref]
- Lipol L, Haq J (2011) Risk analysis method: FMEA/FMECA in the organizations. Int J Basic Appl Sci 11: 74-82.
Editorial Information
Editor-in-Chief
Ying-Fu Chen
Kaohsiung Medical University, Taiwan
Article Type
Research Article
Publication history
Received date: June 07, 2021
Accepted date: June 28, 2021
Published date: July 02, 2021
Copyright
©2021 Ahizoune S. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Citation
Ahizoune S, Benkirane R, El Hiyani M, Alaoui AM (2021) Risk mapping of the management of a hemodialysis patient with Covid-19 in the hemodialysis department of a Moroccan hospital. Trends Med 21: DOI: 10.15761/TiM.1000280
