Abstract
Scapulothoracic dislocation is a rare condition commonly occurring following trauma to the scapular region or a distraction injury to the arm. It is often associated with other serious injuries such as chest injuries brachial plexus lesions. We present a rare case of recurrent spontaneous scapulothoracic dissociations in a young female patient and raise suspicion whether her injury is due to hyperlaxity of the scapular region, or habitual, resulting from factitious disorder or malingering.
Keywords
Scapulothoracic dislocation; Scapulothoracic dissociation
Introduction
Scapulothoracic dislocation or dissociation is a rare condition. The scapula is attached to the rib cage through the insertion of different muscles [1]. It may be an isolated injury but is more commonly associated with multi trauma. Two mechanisms that leads to the injury are a distraction injury to the arm and a direct trauma to the posterior scapula [2]. It is often associated with ligament, muscle, and osseous insults to the shoulder girdle, along with vascular injuries and brachial plexus lesions [3]. It was also described following prior insult to the upper limb gridle, such as a bloc resection of a Pancoast tumour [4], or osteochondroma of the scapula [5]. Spontaneous dislocations are even more scarce and were reported following a firearm injury to the long thoracic nerve and the trapezius muscle [6], and in another patient diagnosed with hyperlaxity and collagen 3 deficit [1]. We found only one prior report of a patient with no associated pathology or trauma, where the brachial plexus was involved, and close reduction was successful [7].
We present a case of 21 years old psychology student who presented to our emergency department (ED) following a recurrent episode of spontaneous scapulothoracic dislocation.
Case report
The patient presented accompanied by her mother and grandparents, with right scapular dislocation following a cough. Her medical history was consisted with multiple events of scapulothoracic dislocations, initially starting two years prior to her presentation while she was combing her hair. Since than she recalled many occasions in which spontaneous dislocation occur, and reduction was either spontaneous or preformed in various local emergency rooms, usually under sedation.
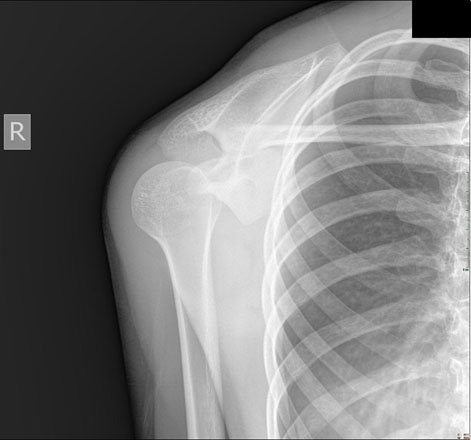
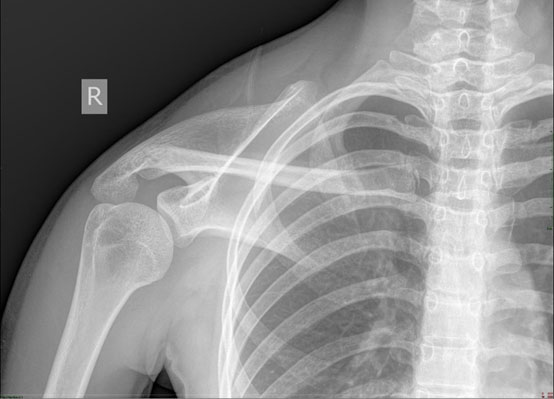
Physical examination revealed an anxious young woman with a displaced right scapula (Figure 1). An active shoulder range of motion limitation was noted, and a passive examination was limited due to pain and lack of compliance. Distal range of motion was intact as well as upper limb sensation and pulses. No signs of hyperlaxity were noted in her physical exam. X-rays revealed superior-lateral movement of the scapula (Figure 2A and Figure 2B). The patient insisted that all reduction maneuvers should be performed under sedation. Following administration of sedative medication and a decrease in muscles tone, a spontaneous reduction was evident.

Figure 1: clinical presentation, lateralization of the scapula with a prominent vertebral boarder.
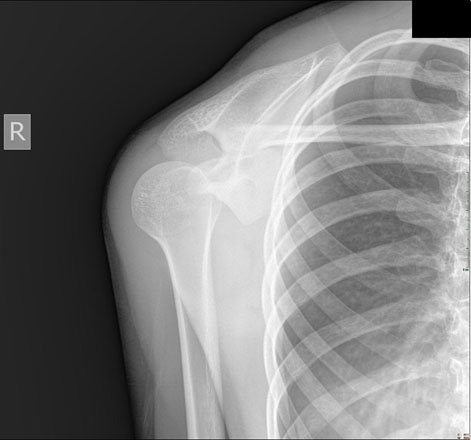
Figure 2A: X-Ray images revealing lateral dislocation of the scapula.
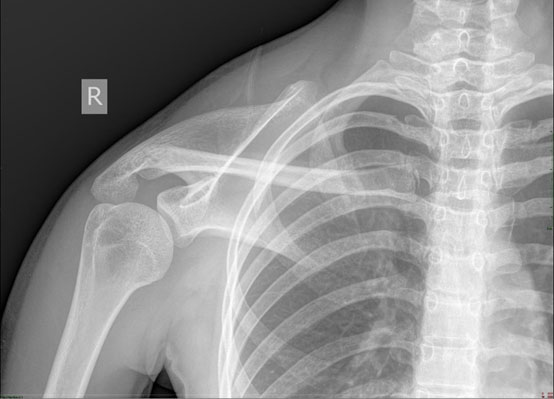
Figure 2B: X-Ray images revealing lateral dislocation of the scapula.
Further investigation into this patient's medical history have revealed seven prior emergency department visits to six other hospitals during the preceding 2 years. No preceding trauma was documented in any of these medical encounters, and reduction attempts were usually done under sedation. In one of the ED records a diagnosis of Fascioscapulohumeral muscular dystrophy (FSHD) was suggested, and it was stated as a reason for discharge from mandatory military service. In a later encounter, it was noted that genetic testing for FSHD was negative. Further imaging was recommended in most hospitals, yet the patient did not comply with the recommendations.
Discussion
Scapular dislocations are rare, and spontaneous ones are even more exceptional. Several of our patients' characteristics raises concerns regarding the nature of her disorder. Her frequent visits to different medical centers with accompanying demands for sedative medication, alongside with her insistence on close familial support at all, times raise concern of immediate primary gain. Her dispensation from mandatory army service, a notable secondary gain, as well supports an understanding that the etiology of these events may be self-inducted, perhaps a factitious disorder or malingering [8], where the manifestation is scapular dislocations. It should be noted that during the time interval starting with the patients' presentation and ending with sedation and the spontaneous reduction, a good part of an hour, a clinical scapulothoracic dissociation was apparent. The position of the scapula was lateral and externally rotated. No effort was seen on the patient's part in maintaining this abnormal position. This might have been enabled by hyper laxity of the scapular region. The event itself may be similar to the more familiar cases of habitual shoulder dislocations, where physicians are instructed to approach patients with caution, as often a subtle underlying psychiatric condition is present [9]. Long thoracic nerve injury may also be suspected, yet no details in the patients’ history indicated a mechanism for such injury, as no trauma or repetitive stretch injuries were noted.
The case presented here is distinguished from other cases by the spontaneous manner of the dislocation, the lack of preceding injury to the upper gridle, and the noted primary and secondary gains mentioned. While scapulothoracic dislocation is a rare condition, one must keep a high index of suspicion whenever a patient presents following a blunt trauma to the shoulder or the thorax. The brachial plexus may be endangered, and a close reduction can lead to good outcomes.
Conflicts of Interest
All authors claim no conflict of interests.
Funding/Support Statement
None
References
- Morande SC, Duart CJ, Llombart BR, Luis J, Gurpide B (2015) Research paper Voluntary Bilateral. UNAV J Med Students.1: 23-26.
- Muniz AE (1998) Scapular dislocation. Am J Emerg Med. 16: 690-691. [Crossref]
- Brucker PU, Gruen GS, Kaufmann RA (2005) Scapulothoracic dissociation: evaluation and management. Injury 36: 1147-1155. [Crossref]
- Ward WG, Weaver JP, Garrett WEJ (1989) Locked scapula. A case report. J Bone Joint Surg Am 71: 1558-1559. [Crossref]
- Hollinshead R, James KW (1979) Scapulothoracic dislocation (locked scapula). A case report. J Bone Joint Surg Am 61: 1102-1103. [Crossref]
- Ibrahim D, Bs BS, Mervis E, Chandwani C (2013) Visual Diagnosis in Emergency Medicine. J Emerg Med 45: 912-914.
- Kushwaha VP, Shapiro MS (1997) Voluntary scapulothoracic subluxation: a case report. Am J Orthop (Belle Mead NJ) 26: 499-501. [Crossref]
- Bass C, Halligan P (2014) Factitious disorders 2 Factitious disorders and malingering?: challenges for clinical assessment and management. Lancet 383:1422-1432. 10.1016/S0140-6736: 62186-62188. [Crossref]
- Goroll, Allan H, Mulley AGJ (2014) Primary Care Medicine?: Office Evaluation and Management of the Adult Patient. 7th ed. (Goroll, Allan H, Mulley AGJ, ed.). Philadelphia: Philadelphia?: Wolters Kluwer/Lippincott Williams & Wilkins Health, [2014]e.