Background: The incidence of scalp neoplasms is continuously increasing as a consequence of the progressive aging of the population. The need to perform a correct excision of scalp neoplasms often requires the removal of the entire skin, galeal and periosteum lining. The consequent complete uncovering of the thecal bone does not allow any type of local grafting and, in the past, has always involved the need to carry out the recovering using local or free flaps. The preparation of the local flaps generally involves large detachments of the scalp, which can cause severe complications of the haemorrhagic type, especially in elderly patients with anticoagulant or antiplatelet treatments. The realization of free flaps, on the other hand, involves a greater anesthetic effort and the creation of a further sacrifice in the donor site.
Methods: The introduction of Dermal Regeneration Templates made it possible to undertake repairing techniques for full-thickness lesions of the scalp with the simple aid of local anesthesia without the need to suspend antiplatelet treatments. The interventions based on the use of Dermal Regeneration Templates are not complex, however they require particular and simple measures which, if not applied, lead to not entirely satisfactory results. This work describes a method of using Dermal Regeneration Templates in the repair of full-thickness lesions of the scalp that follows a rigorous protocol as result of constant internal review.
In particular, we identified three details leading to better results:
- continuous Ford interlocking suture with “double pass” in the DRT ;
- tie-over compression fixed by sutures anchored approximately 5-8 mm externally to the margins of the main suture (8 points);
- antibacterial ointment sealing.
Conclusions: In our opinion, a correct protocol concerning surgical techniques and dressing management allows the shortening of Dermal Regeneration Templates placing times from 6 to 4 weeks; better results in terms of percentage of area with good flourishness, less fluid collection under the Dermal Regeneration Templates and consequently the formation of a more homogeneous and better quality neoderm.
Scalp neoplasm, Dermal regeneration template, Skin cancer, Ford interlocking suture, Tie over
Skin tumors are more frequent in photo-exposed areas and the scalp is the prevalent location for soft tissue malignancies. The scalp has always represented a challenge for reconstructive plastic surgery because the need of the tumor oncological removal often leads to the eradication of the whole soft tissues and frequently also periosteum or cranial theca. The reconstruction covering the resulting defect was entrusted to the usage of graft, proximity flaps or pedunculated and free flaps.
The preparation of the local flaps generally involves large detachments of the scalp, which can cause severe haemorragic complications especially in elderly patients with anticoagulant or antiplatelet treatments. The realization of pedunculated or free flaps, on the other hand, involves the creation of a further sacrifice in the donor site and require the use of general anesthesia. With the introduction of Dermal Regeneration Templates (DRT) it has been possible to perform minimally invasive and technically less complex reparative interventions even for full thickness lesions with local anesthesia and without the need to suspend antiplatelet treatments. Local anesthesia and intravenous sedation allow outpatient management with discharge to home.
One function of acellular dermal matrixes consists in the biologic modulation, meaning the capacity of having impact on organic processes such as the generation of neoderma and healing. The DRT used by our service always consisted in a matrix composed of porous type I collagen derived from bovine tendinous tissue, arranged in the form of a crisscross network including glycosaminoglycans and one layer of semipermeable polysiloxan (silicone). Likewise extracellular matrix this three-dimensional array represents a form of scaffold : the controlled microporosity consents the migration of fibroblasts, lymphocytes and macrophages with the subsequent initiation of cellular growth at its core, as well as concomitant production of endogenous collagen.
The array made of bovine collagen is biodegradable and can therefore be progressively substitued by an autogenous genereated derma. Contemporaneously we can observe a migration of endothelial cells within the reticular collagen master and thus the generation of a neo-vascularisation on its inside. Within a time span of 3-4 weeks a complete reabsorption of the placed DRT and its renewal with a autogenously produced and well vascularized neoderma, can be noted. This newly formed dermal basis allows the subsequent implantation of a thin epidermal graft and adds mechanic stability. Furthermore it’s not submitted to fibrosis and retraction of the graft and guarantees a satisfying cosmetic outcome, especially considering the low local and donor site morbidity.
This paper describes the rigorous surgical and management protocol, developed at the surgical department of the Regional Hospital in Mendrisio (Switzerland), for 26 patients with skin cancer of the scalp, subjected to full-thickness resectioning, exposure of the cranial theca and subsequent two-stage reconstruction with DRT.
We performed a review of all treated cases with DRT between 01/2016 and 12/2019 (4 years) within our department and we collected 82 patients. Among these cases we consequently identified 26 patients operated on the scalp for oncological pathologies.
Our sample has an M / F ratio of 5.5 and the average age consists in 85 years. Among the comorbidity we found hypertension in 12 patients (46%), diabetes in 6 patients (23%) and chronic renal insufficiency in 10 cases (38,4%).
The histological examination revealed 10 cases of Basal Cell Carcinoma (BCC), 14 cases of Squamous Cell Carcinoma (SCC), one case of Lentigo Maligna Melanoma and one case of Melanoma.
After creating a database (Microsoft® Excel® 2016 MSO), we decided to retrospectively analyze the aesthetic and functional result of the reconstruction (primary end-point), focusing on those details of the patient's surgical technique and dressing that may have influenced the process of correct development of a homogeneous and well vascularized neodermis, also identifying the factors that could be the cause of a non-engraftment of the DRT or, on the opposite side, the excessive development of hypergranulation tissue. We relied on operative reports, outpatient letters and photo-documentation collected in all phases of the pre-, intra- and post-operative management.
We have identified as secondary endpoints the reduction of the DRT placing time from 6 to 4 weeks, better results in terms of percentage of engraftment and less fluid collection under the DRT.
To reduce the confounding factors related to the operator, we have selected all cases in which the same Plastic Reconstructive and Aesthetic Surgeon (MDM) was the first operator or second operator in teaching. Again, to reduce confounding factors, we only analyzed cases treated with DRT Integra® bilayer.
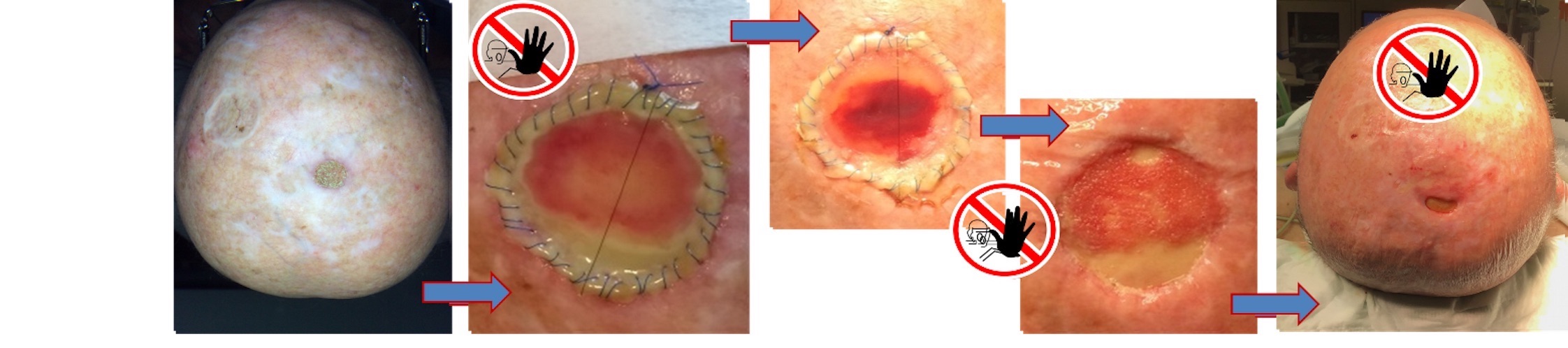
Patient treatment was always provided for 3 operative sessions (Figure 1):

Figure 1. Time-lapse of the treatment protocol of neoplastic lesions of the scalp with DRT.
- first operative step consisting of the removal of the lesion according to oncologic criteria; the application of a temporary synthetic skin substitute of polytetrafluorethylene/polyurethane (EpiGARD®) and the histological examination for R staging of the margins.
- second operative session consisting in the application of DRT after the histological confirmation of R=0
- third operative step by performing a thin skin graft
Extreme attention was paid to the following details of the operative technique:
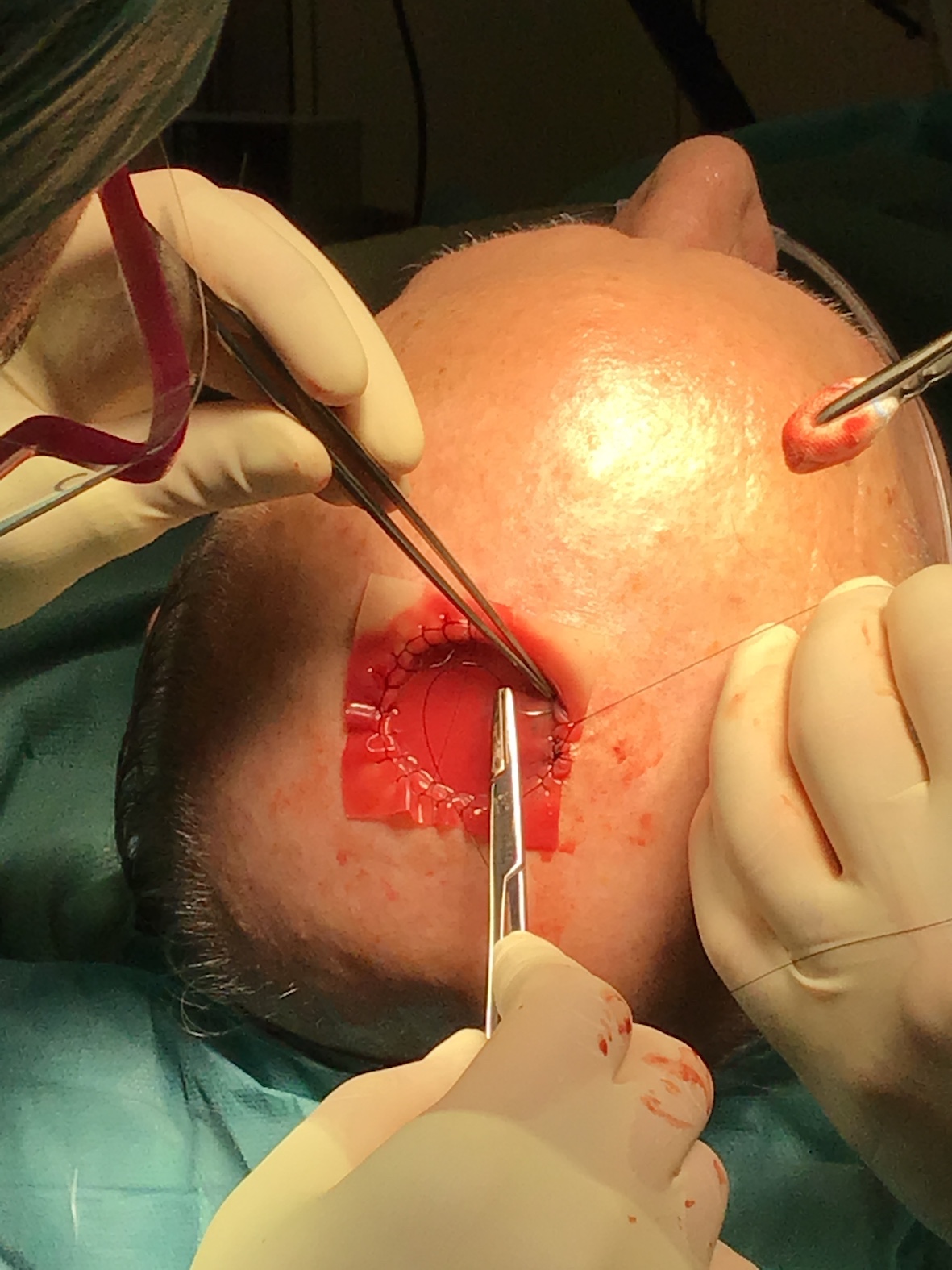
- accurate fixation of the template with continuous Ford interlocking suture using a monofilament suture with “double pass” in the DRT (Figure 2)
- strong compression of the DRT to ensure complete contact with the wound bed using a tie-over fixed by sutures anchored approximately 5-8 mm externally to the margins of the main suture (8 points) (Figure 3)
- careful positioning of dressing and its sealing with an antibacterial fusidic acid ointment to be renewed every two days by experienced nursing staff.
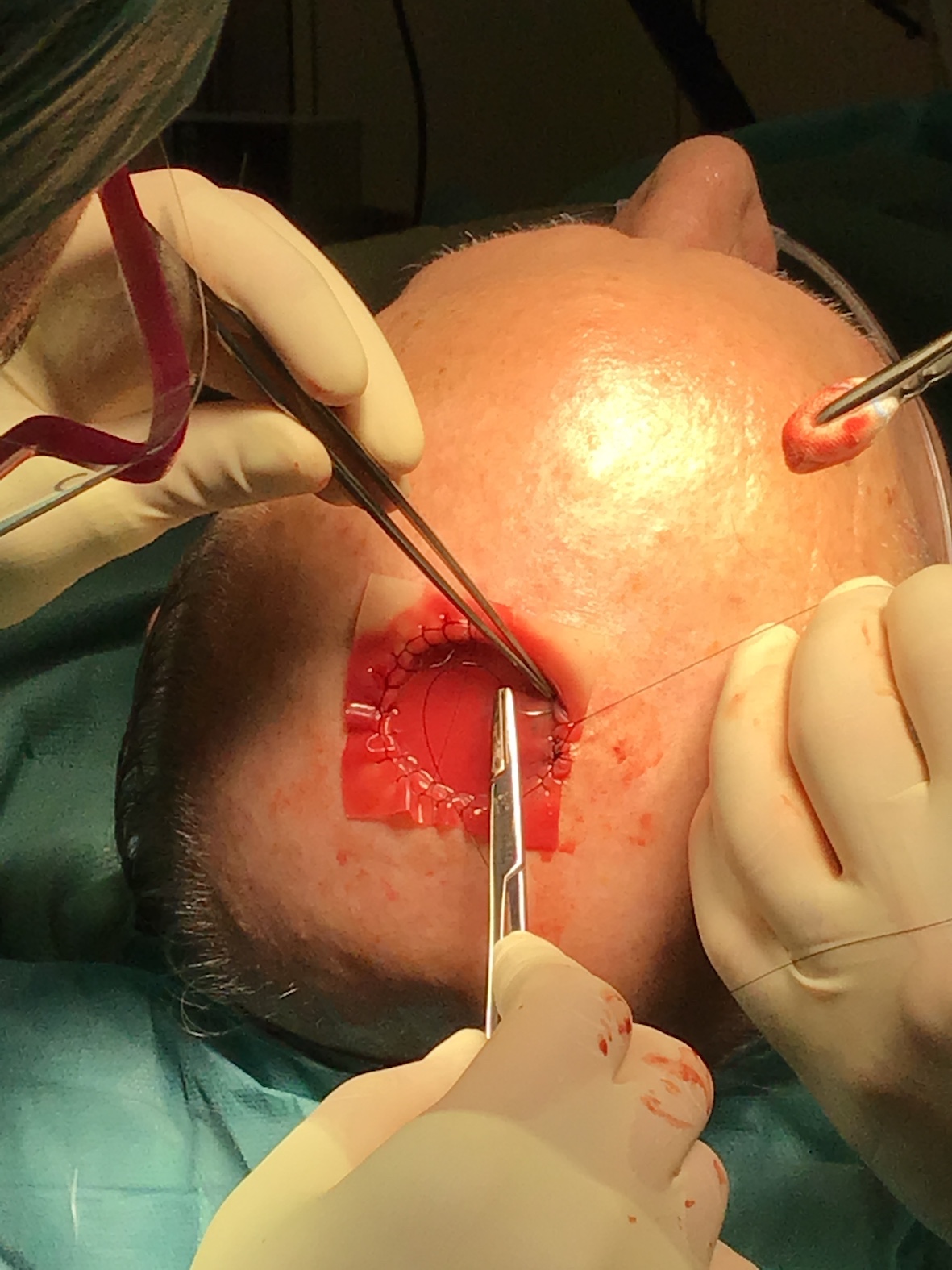
Figure 2. Ford interlocking suture.

Figure 3. Tie over.
We have therefore created a 0-3 rating scale to describe the success after the placing of the DRT (First Reconstructive Time):
- 0: Therapeutic failure (infection or absence of neodermis or hypergranulation tissue with consequent inability to perform grafting)
- 1: complete or partial granulation tissue
- 2: almost complete coverage with good quality neodermis (> 80%)
- 3: complete coverage with vital neodermis, homogeneous and bleeding to the touch
Another scale from 0-3 to describe the final end-point (Second reconstructive time):
- 0: Therapeutic failure (non-healing / re-intervention / healing with another method)
- 1: Partial closure of the defect (Figure 4)
- 2: Total functionally healing but with poor aesthetic result
- 3: Total functionally healing with a satisfactory aesthetic result
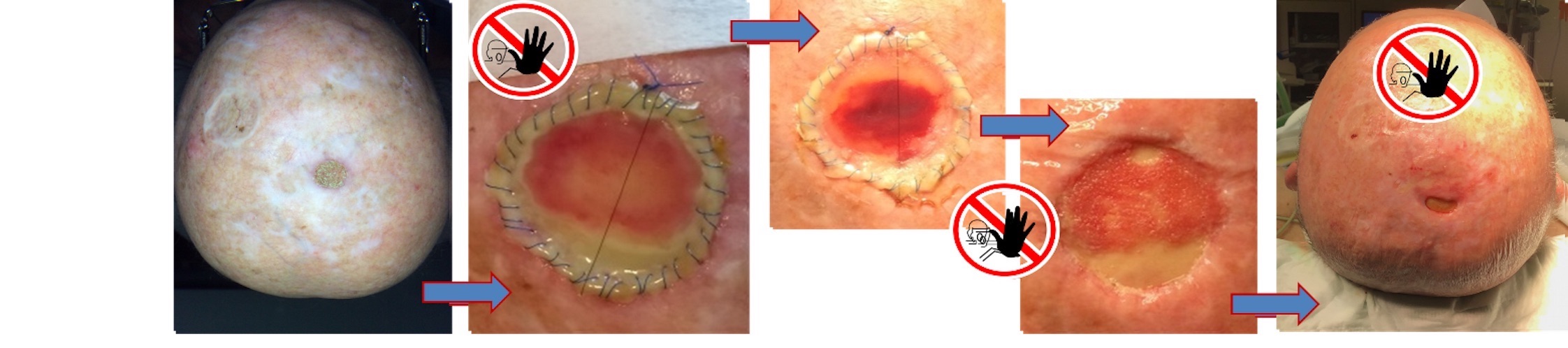
Figure 4. Partial healing defect. Continuous suture but not continuous Ford interlocking suture and incomplete adhesion of the DRT to the inferior pole wound bed identified as failure factors.
Descriptive analyzes were performed using the IBM SPSS (version 26) statistical package for Apple. Values are shown as mean plus standard error of mean (s.e.m.).
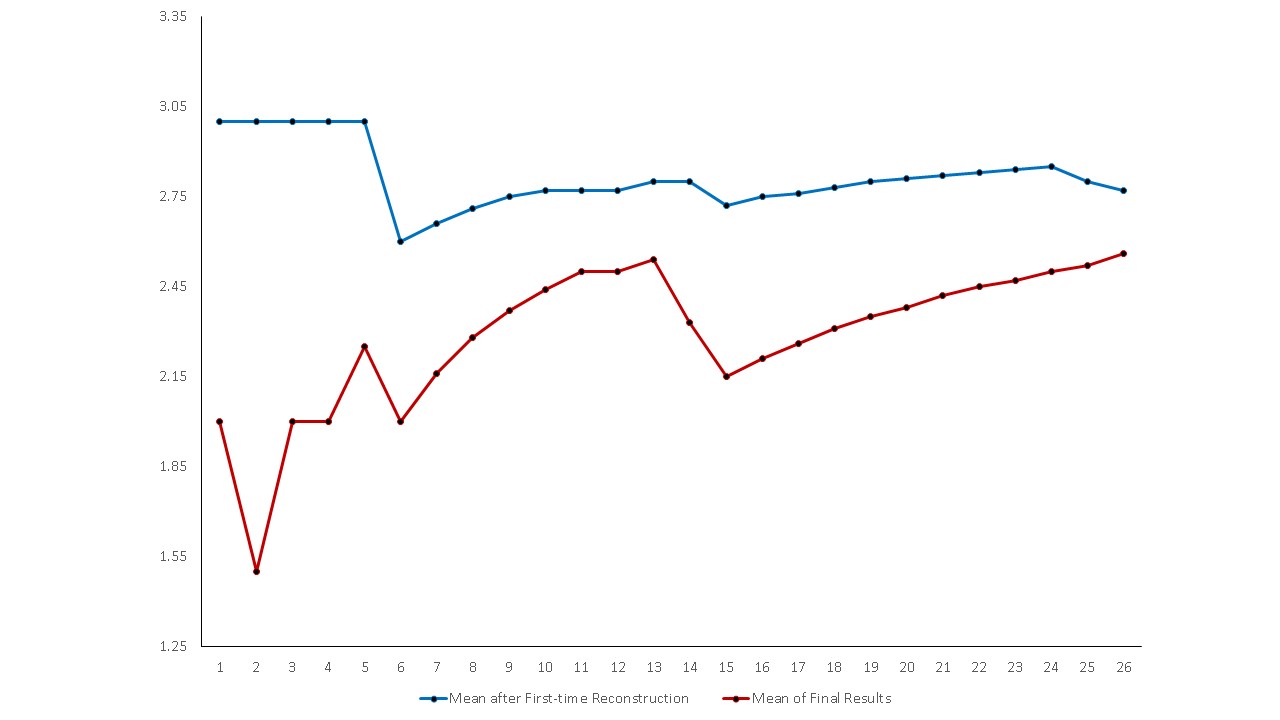
We created a graph by inserting the moving average of the results obtained after the placement of the DRT (first reconstructive time) and the moving average of the final results based on the primary end-points (Figure 5).
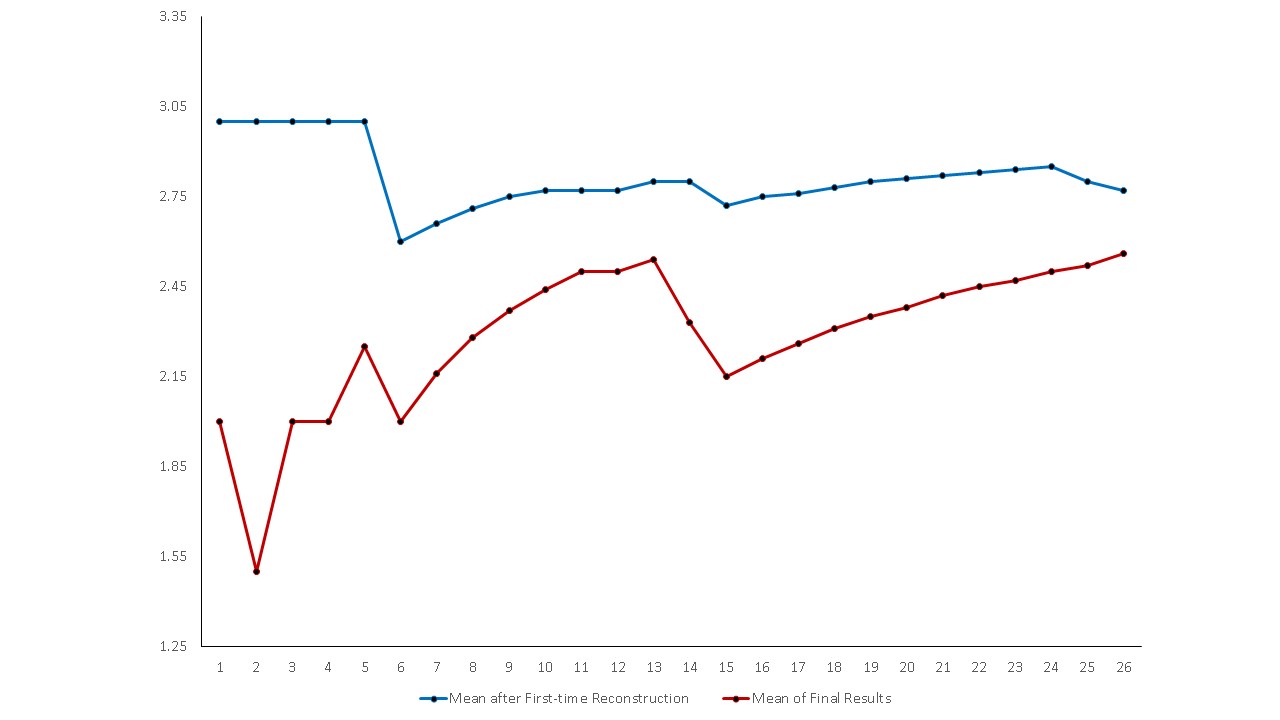
Figure 5. Moving Average of the results after the first reconstruction time and at the end of the reconstruction process.
From the graph it’s possible to observe a good and stable improvement of the final result especially in the last 10 patients. It is possible to correlate the constant improvement with better surgical performance and or better clinical management throughout the therapeutic process.
In particular, we identified the details of the patient's surgical and dressing techniques leading to better results, and in particular the following factors:
- continuous Ford interlocking suture with “double pass” in the DRT;
- tie-over compression fixed by sutures anchored approximately 5-8 mm externally to the margins of the main suture (8 points);
- antibacterial ointment sealing.
The analysis of cases with unsatisfactory results made it possible to verify that the measures mentioned above had not been adequately adopted in these patients (Figure 4).
Skin cancer is the most common form of neoplasm [1]. Studies also show that the global incidence of BCCs increased by 145% between 1976-1984 along to 2000-2010, and that the global incidence of SCC increased by 263% over the same period [2]. The survival rate of BCC and SCC, the two most common forms of skin cancer, is very high if diagnosed appropriately and early [3]. Invasive melanoma is expected to become the 5th most prevalent cancer in both men and women in 2020. Caucasian men over 50 years old have a higher risk of developing melanoma than the general population and the incidence of melanoma in men over 80 years old is three times higher than in women in the same age group. The 5-year survival rate in patients diagnosed and treated for melanoma before it has spread to the lymph nodes is 99% [4].
A shared risk factor for all skin cancers consists in the exposure to natural and artificial ultraviolet (UV) rays [5]. Likewise, most cases of melanoma are attributed to exposure to UV rays [6]. The increasing intermittent exposure to sunlight during youth, but in general throughout life, is associated also with an increased risk of developing BCC and SCC [7].
Skin tumors are more frequent in photo-exposed areas and the scalp is the prevalent location for soft tissue malignancies [8].
The scalp reconstruction has always represented a difficult challenge for reconstructive plastic surgery [9,10].
Following the ladder rule in reconstructive surgery, scalp reconstruction has always involved surgical treatments using grafts or local flaps for moderate partial thickness loss of substance, while surgery using pedunculated flaps or free flaps was reserved for large losses of substance or full-thickness lesions of the scalp [11,12].
These types of surgery always involved inpatient treatment, the use of general anesthesia and has always represented a surgery not free from complications, often creating permanent functional and aesthetic damage in the donor site.
Surgical treatment with one-time reconstruction using grafts or flaps was also burdened by a high risk of necrosis of the covering tissue, especially in the case of bone exposure following a total thickness demolition surgery [13].
In cases of melanoma or very advanced carcinomas, immediate cover with flap can also be an obstacle to careful follow-up surveillance as the neoplasm can regenerate again in the deeper layers covered by the flap and escape periodic clinical control [12,14].
The DRT is composed of a layer of bovine collagen crossinked with glycosaminoglycan and covered by a silastic membrane. The first description of the use of the DRT dates back to the early 1980s, when it was published by Burke et al. its use for the treatment of extensive burns [15,16].
Currently, the use of DRT for skin and scalp reconstruction after cancer surgery is widely accepted and allows the execution of less complex operations in two steps with the aid of local anesthesia associated with intravenous sedation in an outpatient setting with rapid home discharge after a few hours [9].
Regarding the reconstructive surgery of the scalp there is today an agreement between the authors regarding the indications. The treatment by DRT is recommended in the following cases:
1) elderly or extreme elderly patients which may present additional risk factor related to comorbidity [9,17,18]
2) in case of wide local excision (>4cm) [19-21]
3) in case of bone exposure resulting from the removal of the periosteum [8,9,22]; in this case it is recommended to drill the outer table to vascularize the DRT from the bone marrow [23]
4) in case of previous surgery with graft or flap failure or in case of recurrence of the neoplasm [9,24,25]
5) in case of previous radiation therapy (pre or postoperative irradiation at the surgical site) [26- 28]
6) in patients with very aggressive cancer in which close postoperative clinical surveillance is deemed necessary. [17, 21, 24, 27, 29, 30]
There is also agreement among the authors that the use of the DRT is more economically advantageous than the cover with flaps [31] especially if the operated surface is greater than 120 square cm [23].
Some authors have proposed the use of the DRT with the one step technique without subsequent thin skin grafting, thus favoring healing by secondary intention [32]. Considering that healing by secondary intention can take up to 13 weeks, we believe this is a procedure not recommended. In addition, we usually precede the use of the DRT by a histopathological report that certifies the health of the resection margins and therefore at the end of the demolition operation we use a temporary economic cover in polytetrafluorethylene / polyurethane. So, our procedure consists of three outpatient steps under local anesthesia with rapid discharge at home.
The use of compression by NPWT can be indicated in case of large excisions even if it must be carefully monitored as it can cause superinfection or better selection of resistant germs [9,33].
In the international literature, as mentioned, there is a common agreement on the indications for the use of the DRT, however the technical details relating to the positioning, fixation and dressing of the DRT are never described with due precision, details that in our opinion are fundamental for obtain quality and constant results. Some authors [15] have reported infection as the only significant variable in relation to the outcome of the application of DRT, however we consider that the technical precision of positioning, compression and dressing can make a significant difference in the primary end point. Our technique derives from the application of a protocol refined over time that has proven to be able to make a statistical difference between the first operated cases and the last of the series.
This study represents a relevant case history regarding the problem faced. Although our attention has focused on reconstruction of the scalp after cancer surgery using DRTs, we believe neoplasms of the scalp can become increasingly important. Based on the United Nations Department of Economic and Social Affairs and the WHO World Report on Aging and Health, we expect the demand for treating this type of diseases to steadily increase in the upcoming years.
The reconstructive technique with skin grafts is a less invasive method in the comparison to other alternatives and thus allows to treat more fragile patients with different comorbidities. The ability to perform the surgery under local anesthesia, the low morbidity of the donor site and the relatively simple surgical technique allow this treatment modality to be performed even in the smallest hospitals.
Our protocol proposes three operative sessions to be sure of having performed an R0 removal of the tumor.
The simplification of the surgical technique, the standardization of the post-operative management protocol and the creation of a validated treatment path are the basis for offering a good service in the treatment of scalp cancer of any size.
Regarding the data we produced, it was not possible to perform an inferential statistic, but only a descriptive one. By increasing the number of cases, and following a systematic review of the literature, it would be possible to perform a detailed analysis with Paerson-type correlation indices.
The protocol we proposed has shown good results, with satisfaction on the patients and we hope to contribute with this work to the standardization of procedures using DRT as treatment modality within treating neoplastic lesions of the scalp.
Marco De Monti: surgeon, clinical management of the case, writing and supervision of the paper, corresponding Author.
Fabiana Castonovo: statistical processing
Marta Teglas: clinical management of the case
Laura De Pellegrin: resident surgeon, proof reading
Alessandro Torre: study conception, acquisition of data, writer
All Authors read and approved the final version of the manuscript; all Authors declare there are no conflicts of interest associated with this publication and there has been no significant financial support for this work that could have influenced its outcome.
In view of the fact that this is an anonymized and non-randomized retrospective study, approval by the ethics committee was not required.
Patients are hereby declared to have signed consent for the retrospective and anonymized use of their data.
- Guy GP Jr, Thomas CC, Thompson T, Watson M, Massetti GM, et al. (2015) Vital signs: Melanoma incidence and mortality trends and projections—United States, 1982–2030. MMWR Morb Mortal Wkly Rep 64: 591-596. [Crossref]
- American Academy of Dermatology/Milliman (2017) AAD Burden of Skin Disease.
- American Cancer Society (2019) Cancer Facts & Figures, Atlanta.
- Siegel RL, Miller KD, Jemal A (2019) Cancer statistics, 2019. CA Cancer J Clin 69: 7-34. [Crossref]
- Parkin DM, Mesher D, Sasieni P (2011) 13. Cancers attributable to solar (ultraviolet) radiation exposure in the UK in 2010. Br J Cancer 105: S66-S69. [Crossref]
- Arnold M, de Vries E, Whiteman DC, Jemal A, Bray F, et al. (2018) Global burden of cutaneous melanoma attributable to ultraviolet radiation in 2012. Int J Cancer 143: 1305-1314. [Crossref]
- Lin JS, Eder M, Weinmann S (2011) Behavioral counseling to prevent skin cancer: asystematic review for the U.S. Preventive Services Task Force. Ann Intern Med 154: 190-201. [Crossref]
- Harirah M, Sanniec K, Yates T, Harirah O, Thornton JF (2021) Scalp Reconstruction after Mohs Cancer Excision: Lessons Learned from More Than 900 Consecutive Cases. Plast Reconstr Surg 147: 1165-1175. [Crossref]
- Magnoni C, De Santis G, Fraccalvieri M, Bellini P, Portincasa A, et al. (2019) Integra in Scalp Reconstruction After Tumor Excision: Recommendations From a Multidisciplinary Advisory Board. J Craniofac Surg 30: 2416-2420. [Crossref]
- Garcovich S, Colloca G, Sollena P, Andrea B, Balducci L, et al. (2017) Skin cancer epidemics in the elderly as an emerging issue in geriatric oncology. Aging Dis 8: 643–661. [Crossref]
- Boyce DE, Shokrollahi K (2006) Reconstructive surgery. BMJ 332:710– 712.
- Hussussian CJ, Reece GP (2002) Microsurgical scalp reconstruction in the patient with cancer. Plast Reconstr Surg 109: 1828–1834. [Crossref]
- Koenen W, Goerdt S, Faulhaber J (2008) Removal of the outer table of the skull for reconstruction of full-thickness scalp defects with a dermal regeneration template. Dermatol Surg 34:357–363. [Crossref]
- Rudolph R (1982) Complications of surgery for radiotherapy skin damage. Plast Reconstr Surg 70: 179–185. [Crossref]
- Ferrari B, Reggiani C, Francomano M, Bellini P, Ferrari F, et al. (2020) Clinical Factors Influencing the Outcomes of an Acellular Dermal Matrix for Skin Cancer Treatment: A Retrospective Study. Adv Skin Wound Care 33: 367-374. [Crossref]
- Burke JF, Yannas IV, Quinby WC, Bondoc CC, Jung WK (1981) Successful use of physiologically acceptable artificial skin in the treatment of extensive burn injury. Ann Surg 194: 413-428. [Crossref]
- Corradino B, Di Lorenzo S (2011) An algorithm for oncologic scalp reconstruction. Plast Reconstr Surg 127: 2506. [Crossref]
- Bernstein JL, Premaratne ID, Levy AS, Kuhel WI, Kutler DI, et al. (2020) Reconstruction of Full Thickness Scalp Defect in Extremely Elderly Patients Using Dermal Regeneration Templates. J Craniofac Surg 31: 511-514. [Crossref]
- Fung V, Chalmers RL, Geh JL (2014) Scalp reconstruction using Integra, an alternative to free tissue transfer—case report. OALib J 1: 1–5.
- Cunningham T, Marks M (2014) Vacuum-assisted closure device and skin substitutes for complex Mohs defects. Dermatol Surg 40: S120–S126. [Crossref]
- Romano G, Bouaoud J, Moya-Plana A, Benmoussa N, Honart JF, et al. (2021) Integra® dermal regeneration template for full thickness carcinologic scalp defects: Our 6 years' experience retrospective cohort and literature review. J Stomatol Oral Maxillofac Surg 122: 256-262. [Crossref]
- Pannucci CJ, Collar RM, Johnson TM, Bradford CR, Rees RS (2012) The role of full-thickness scalp resection for management of primary scalp melanoma. Ann Plast Surg 69: 165–168. [Crossref]
- Benecke J, Koenen W, Mager L, Weina K, Klemke CD, et al. (2021) Reconstruction of Full Thickness Defects on the Scalp with Artificial Dermal Regeneration Template: Analysis of Long-Term Results in 68 Cases. Dermatol Surg 47: e1-e4. [Crossref]
- Komorowska-Timek E, Gabriel A, Bennett DC, Miles D, Garberoglio C, et al. (2005) Artificial dermis as an alternative for coverage of complex scalp defects following excision of malignant tumors. Plast Reconstr Surg 115: 1010–1017. [Crossref]
- Stroder M, Litt JS, Litofsky NS (2021) Complex Multidisciplinary Cranial and Scalp Reconstruction for Patient Salvage. World Neurosurg 152: e549-e557. [Crossref]
- Tufaro AP, Buck DW 2nd, Fischer AC (2007) The use of artificial dermis in the reconstruction of oncologic surgical defects. Plast Reconstr Surg 120: 638–646. [Crossref]
- Khan MA, Ali SN, Farid M, Pancholi M, Rayatt S, et al. (2010) Use of dermal regeneration template (Integra) for reconstruction of full-thickness complex oncologic scalp defects. J Craniofac Surg 21: 905–909. [Crossref]
- Gonyon DL Jr, Zenn MR (2003) Simple approach to the radiated scalp wound using INTEGRA skin substitute. Ann Plast Surg 50: 315–320. [Crossref]
- Chalmers RL, Smock E, Gen JLC (2010) Experience of Integra in cancer reconstructive surgery. J Plast Reconstr Aesthet Surg 63: 2081– 2090. [Crossref]
- Baldelli I, Mangialardi ML, Salgarello M, Raposio E (2020) Surgical Reconstruction following Wide Local Excision of Malignant Melanoma of the Scalp. Plast Reconstr Surg Glob Open 8: e3059. [Crossref]
- Schiavon M, Francescon M, Drigo D, Salloum G, Baraziol R, et al. (2016) The use of Integra dermal regeneration template versus flaps for reconstruction of full-thickness scalp defects involving the calvaria: A cost-benefit analysis. Aesthetic Plast Surg 40: 901-907. [Crossref]
- De Angelis B, Gentile P, Tati E, Bottini DJ, Bocchini I, et al. (2015) One-stage reconstruction of scalp after full-thickness oncologic defects using a dermal regeneration template (Integra). Biomed Res Int 2015: 698385. [Crossref]
- Apelqvist J, Willy C, Fagerdah AM, Fraccalvieri M, Malmsjö M, et al. (2017) Negative pressure wound therapy – overview, challenges and perspectives. J Wound Care 26: S1–S154. [Crossref]