Introduction: Current implant rehabilitations must take into account prosthetic imperatives. Pre-implant planning permits to highlight some unfavorable clinical situations that compete against the ideal implant location. An alternative prosthetic design intending the use of an implant-supported cantilevered bridge may be suggested.
Purpose: The main aim of our review is to analyze the biomechanics of fixed partial implant cantilevered restorations as well as the criteria for a reliable choice of this design.
Materials and Methods: The literature research was performed using the PubMed, direct Science and Google scholar electronic databases, using the following keywords and Boolean equations: (((partial implant supported dental prosthesis) and (cantilever); ((((Biomechanics) and (fixed dentures)) and (implants)) and (cantilever)); ((((Biomechanics) and (fixed dentures)) and (implants)) and (extension)). To be selected, articles must be published between 2010 and 2020.
Results: Nine articles using various methods of stress evaluation: photoelasticimetry, strain‑gauge measurement, and finite element analysis (FEA) were included in our review to analyze the biomechanics of cantilevered fixed partial implant prostheses.
Conclusion: The prognosis of cantilever implant prostheses depends on the length, location of the cantilever, the superstructure materials, the density and the size of the available bone. The prosthodontist can choose the best treatment approach by acting on the factors improving the biomechanical behavior of cantilever restorations.
Partial implant supported dental prosthesis, Cantilever, Biomechanics, Fixed dentures, Extension
FEA: Finite element analysis, FPD: Fixed partial denture, VMS: Von Mises stress, EQS: Equivalent strain, CFP: Cantilever fixed partial denture, ICFDP: Implant cantilevered fixed dental prosthesis, ISFPD: Implant-supported fixed partial denture, RCT: Randomised controlled trial
Oral implant rehabilitations are set in two chronologically distinct stages: surgical stage and prosthetic stage. Specific requirements are necessary at each stage.
Implant placement guided by the prosthetic project results from the best compromise between local anatomical deformations and the possibility of adapting a functional, aesthetic prosthetic supra-structure without compromising the longevity of the underlying implant.
It is therefore necessary to analyze each clinical situation and achieve an appropriate implant-prosthetic planning, in order to achieve non-dogmatic and personalized treatment options for each clinical case.
In some clinical conditions, implant supported cantilevered bridges may be an alternative to avoid additional surgical interventions before or concomitant with the implant placement [1].
In spite of the positive clinical outcomes of cantilever bridges, long-term apprehensions have been expressed about the biomechanical consequences and the relevant technical complications [2]. Numerous studies have shown that implant-supported cantilever bridges can induce excessive stress concentrations in the supporting alveolar bone [3,4].
The purpose of this article is to analyze the biomechanics of cantilevered implant supported bridges, the reliability of this design as well as the choice criteria that manage it.
The MEDLINE, Google Scholar and direct Science databases were used to perform electronic searches of relevant published studies in English up to January 2010, according to the following Boolean equations: (((partial implant supported dental prosthesis) AND (cantilever) (((Biomechanics) AND (fixed dentures)) AND (implants)) AND (cantilever)) ((((Biomechanics) AND (fixed dentures)) AND (implants)) and (extension))
After the selection of articles beginning with the reading of the title and abstract, the complete texts of the studies of interest were assessed for analysis using the pre-established inclusion and exclusion criteria.
Inclusion criteria
The articles were included if they meet these criteria:
-Article dealing with the biomechanics of the cantilevered fixed partial implant prosthesis.
- Published from 2010 to 2020
- Written in English
Exclusion criteria
Articles were excluded if they meet one of the following criteria:
-Article does not match with the purpose of this article.
-The studies before 2010
- Articles that have titles or summaries that did not seem appropriate to our topic.
- Case reports, literature papers, surveys.
The PICO question was used to define the impact of cantilevers on biomechanical behavior of implant supported fixed partial dentures: (P) population as the groups or models studied; (I) intervention or study protocols; (C) for the Comparison and (O) for the Outcome.
The systematic review is performed according to the PRISMA statement (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) criteria [5].
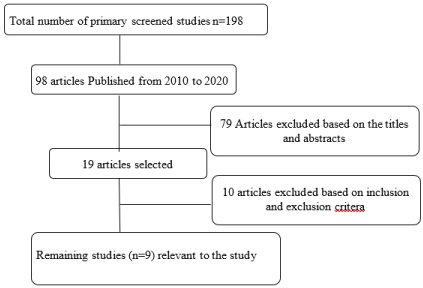
The electronic search identified more than 198 articles. Out of the 98 articles obtained, 79 were excluded based on initial screening of the title and abstract, as they are not relevant to the objectives of the present review. After the application of the inclusion and exclusion criteria during the reading of the complete texts, nine articles were included in the present study [Figure 1].
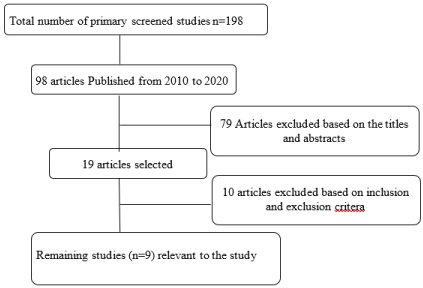
Figure 1. Flowchart of published literature search strategy
All included articles were in vitro studies. To evaluate the biomechanical behaviors of implant-supported cantilevered bridge, different methods have been reported such as photoelasticity, strain‑gauge measurement, and finite element analysis (FEA). FEA is a valuable tool for simulating oral conditions [6], especially in clinical situations that require high precision [7].
The results of our research have allowed us to identify several elements that may be included in the study of the biomechanics of cantilever fixed partial implant prostheses, such as bridges designs, characteristics, and position of supporting implants, cantilever lengths and fixation system. The data collected from the studies are summarized in (Tables 1-3).
Table 1. Bridge configurations
study |
Population |
intervention |
Comparison |
Outcomes |
Wang et al. [8] |
Model A: single implant-supported two-unit cantilever FPD;
Model B: double implant-supported two-unit non-cantilever FPD |
3D finite element model of a maxillary bone with two absent central incisors was constructed on the basis of clinical computed tomography data.
Bone responses under normal and overload conditions were compared between the cantilever and non-cantilever models. |
Compare the bony biomechanical response and possible long-term restorative consequences stemming from the use of two-unit fixed partial dentures (FPDs) with or without cantilever configuration. |
Bone resorption due to overloading was more severe in the cortical neck around the implant-supported cantilever FPD (bone density decreased by about 77%) as compared with the non-cantilever configuration |
Yoda et al. [9] |
Four different configurations of implants supporting 3-unit FPDs:
*Three implant-supported FPD,
*Conventional three-unit bridge FPD,
*Distal cantilever FPD
*Mesial cantilever FPD |
A 67-year-old healthy woman subject, who had three implants in her left mandibular free-end partially edentulous region.
The 3D dynamic loads exerted on implants were measured during chewing a piece of gum using a piezoelectric force transducer. |
Evaluate the effect of implant configurations supporting three-unit fixed partial denture (FPD) on the stress and strain distribution in the peri-implant bone |
The higher Von Mises stress (VMS) and equivalent strain (EQS) values were observed at the implant neck region adjacent to the cantilever extension in the cantilevered configurations.
In the case of the cantilevered design, the implant adjacent to the cantilever extension may be of a high risk of loss of osseointegration. |
Kobari et al. [10] |
Four implant configurations for a three-unit FPD depending on the number and position of the implants were Considered:
M1: A three-implant–supported FPD
M2: a conventional FPD
(central pontic),
M3: posterior cantilevered FPD (posterior cantilever), M4: anterior cantilevered FPD (anterior cantilever). |
A 67-year-old female patient with three implants (in the mandibular left second premolar, first molar, and second molar regions) was recruited.
The loads on the implants were
recorded during maximum voluntary clenching (MVC-test) and when chewing a piece of chewing gum (GUM-test). |
Investigate the effects of implant configuration on the load distribution under
a three-unit fixed partial denture (FPD) |
*A three-implant prosthesis and central pontic provide biomechanically beneficial designs compared with the posterior cantilever and anterior cantilever in terms of the equal distribution of loads on supporting implants.
*The maximum compressive load
(318.90 ± 70.71 N) was detected on the first molar in the posterior cantilever during the GUM-test. |
Batista et al. [11] |
The model configurations:
M1: Three implants supporting splinted crowns; M2: Two implants supporting prosthesis with central pontic; M3: Two implants supporting prosthesis with mesial cantilever;
M4: Two implants supporting prosthesis with distal cantilever |
Four models were developed with three variation factors: the number of implants, design of rehabilitation and loading type.
The applied forces were 400 N axial and 200 N oblique.
*Maximum principal stress and microstrain criteria were used to evaluate the bone tissue. |
Evaluate the influence of pontic and cantilever designs (mesial and distal) on 3-unit implant-retained prosthesis at maxillary posterior region |
the use of the central pontic (M2)
showed stress and strain distributions more favorable in the analyzed structures.
The use of cantilever showed unfavorable biomechanical behavior (M3 and M4), mainly for distal cantilever (M4). |
Goiato et al. [12] |
Models were made in photoelastic resin and divided depending on the cantilever lengths (one or two crowns/elements in the
cantilever). |
The implant-prosthesis unit was positioned in a circular polariscope. Photographic recording was initially performed without loading. Next, axial and oblique
loadings of 100 N were applied
* Results were recorded on a digital camera and visualised in a computer graphics program. |
The photoelastic analysis is used to evaluate the biomechanical behaviour of double-screwed, implant-supported crowns with different cantilever lengths |
*During axial loading, all of the groups with one or two elements had a similar number of fringes
*The number of fringes increased when oblique loading was applied.
Groups with longer cantilevers (two crowns) had higher stress. |
Table 2. Implant characteristics: diameter, lengths and collar geometries of implants
Study |
|
Population |
intervention |
Comparison |
Outcomes |
Meriç et al. [13] |
|
Unilateral posterior 3-unit cantilever FPDs supported with two osseointegrated implants which contain different collar geometries :
microthread collar structured (MCS) and nonmicrothread
collar structured (NMCS) |
FEA was conducted using mathematical models of unilateral posterior 3-unit cantilever FPDs.
300 N vertical and 150 N oblique forces were applied to the models separately. The stress values in the bone, implant-abutment complex were calculated. |
Comparing the effects of two distinct collar geometries of implants on stress distribution in the bone around the implants supporting cantilever fixed partial dentures |
Stress distribution in implant-supported CFPDs correlated with the macro design of the implant collar and the direction of applied force.
Higher von Mises stresses have been noted in veneering material for NMCS models. |
Sallam et al. [14] |
|
Model 1: Two standard-size implants (3.75/13 mm) were inserted in the position of the second premolar and first molar to support 3-unit cantilever bridges.
Model 2: A standard implant and a mini implant (3.0/ 13 mm) were inserted in the position of the second premolar and second molar, respectively, to support fixed-fixed 3-unit bridges. |
Two models simulating mandibular unilateral free-end saddle were fabricated.
*Four strain gauges were mounted buccally, lingually, mesially, and distally adjacent to each implant. A 300 N vertical load was applied. Microstrains were recorded and analyzed. |
Analysis of the microstrains around small- versus standard diameter implants used in restoration of thin wiry ridge through different bridge designs |
*Cantilever bridges recorded higher microstrains than fixed-fixed bridges for both loading conditions.
*Mini implant revealed greater strain values than standard implant supporting the same fixed partial denture. |
Borie et al. [15] |
|
Model 1 : two implants with 4.0-mm diameters placed in the maxillary central incisors to simulate an implant-supported fixed prosthesis with four elements with a cantilever of both maxillary lateral incisors.
Model 2 : two implants with 3.75-mm diameters placed in the maxillary lateral incisors to simulate a conventional fixed prosthesis with four elements with pontics for maxillary central incisors. |
A finite element model of a maxillary image was created from a tomography data bank. The simulations were executed in two types of models.
The models created were subdivided according to implant length ( 8.5mm/ 10mm) and connection ( flat top/ Conical cone)
*A total static oblique load of 150 N was applied to the cingulum area of the palatal surfaces of the four incisors
*Bone stresses were analyzed through maximum and minimum principal stresses. |
Evaluation of the biomechanical behaviors of multiple implant-supported prostheses with different implant lengths, locations, and connections, in the maxillary anterior region using three-dimensional finite element analysis |
*The cantilever prosthesis model
with flat top connection exhibited considerable stress concentrations in the abutment and fixation screw.
Planning for cantilever prostheses with metal-ceramic restorations and 4-mm diameter, 8.5-mm-long implants seems to be the best option. This approach exhibited a better stress distribution in the peri-implant bone |
Table 3. Fixation system: cemented or screwed?
study |
Population |
Intervention |
comparison |
Outcomes |
Alencar et al. [16] |
*Group 1: models of fixed partial prostheses cemented onto implants with mesial or distal cantilevers;
*Group 2 : models of fixed partial denture screwed onto implants with mesial or distal cantilevers |
The experimental design consisted of four 3D models
obtained by volumetric computerized tomography and analyzed using finite FEA. To simulate implant-supported cantilevers fixed partial in the region of teeth (34, 35, 36)
The axial and oblique loads were applied (50 N for molar implants and 30 N for premolar implants) |
Compare stresses in the peri-implant bone produced by fixed partial prostheses with mesial and distal cantilevers, when cemented or screwed onto implants |
*The screwed fixed prostheses caused less stress on peri-implant bone regardless of whether the cantilever was located mesially or distally.
*Oblique loads produce more stress in peri-implant bone.
*Stresses are more homogenously distributed in the bone around implants with mesial cantilevers, when compared with distal cantilevers. |
The purpose of our review is to study the biomechanics of cantilever fixed partial implant restorations. therfore, we excluded studies reporting on the biomechanics of complete implant-supported restorations in order to provide an accurate answer to our problem.
Bridge configurations
Biomechanically, peri-implant bone remodeling is induced by mechanical stimuli [17], therefore, it is essential to quantify the mechanical stimuli generated by the functional occlusal load transferred to the implants for the success of the implant treatment.
Our analysis of the literature revealed that under normal conditions of masticatory forces, there were no statistically significant differences in biomechanical behavior between cantilever and non-cantilever implant restorations [18,19]. The success rate and survival rate of cantilever fixed partial prostheses is about 57.7% and 100%, respectively [20]. Storelli et al. in a systematic review, investigated the success rate of implant supported cantilevered fixed dental rehabilitations in partially edentulous patients. The estimated survival rate for 5–10 years was calculated to be 98.4% for the implants and 99.2% for the rehabilitations [21]. Another systematic review assessed the survival rate of cantilevered and non-cantilevered partial rehabilitations: the survival rate of the prostheses was calculated to be 95.4% at 5 years. The survival rate of ICFDP rehabilitations appears to be similar to that of non-cantilevered restorations [21]. A retrospective study reported that a cumulative survival rate at 30 years was 72.7% [22].
Some differences were obvious in other studies. According to Yoda et al. and Kobari et al. the bridge configuration induces a more evenly distributed bone density compared to the cantilever design [9,10]. Furthermore, under overload conditions, the highest levels of stress are located in the alveolar bone crest of the implant closest to the cantilever [8,9].
Although some studies have concluded that the implant supported fixed partial dentures with a distal cantilever is a reliable therapeutic option [10,23]. Another study reported that the use of one implant for each missed tooth provides lower values of stress/strain in all structures. In cases where one implant for each missing tooth is not possible, the use of a distal cantilever should be avoided due to unfavorable biomechanical behavior, which could increase the chances of treatment failure [11]. These results corroborate with Kreissl et al. [24] Other authors have specified that a posterior cantilevered FPD require more careful consideration, as these FPDs can potentially be overloaded, particularly in patients with powerful masticatory muscles or parafunctional habits [10,18].
Cantilever length:
The two main types of force that act on the implant are the axial force and oblique force. Axial force is more favorable in that it distributes stress more uniformly along the long axis of the implant. However, oblique force generates greater stress on the implant and bone tissue [25], and this increase disproportionately with increase in cantilever length.
Coelho Goaito et al. used photoelastic analysis to evaluate the biomechanical behavior of implant-supported cantilevers FPD. They concluded that a cantilever length did have a direct influence on stress distribution, with a greater concentration of force on the cervical part of the implant [12]. Another study suggested, a minimum bone resorption increase of 0.1 mm per 1 mm increase in cantilever length [26].
It is also interesting to note that, ISFPDs with a cantilever prosthetic arm presented a higher risk of prosthesis failure, as well as a higher risk for screw loosening or screw fracture. This is in agreement with some previous studies [1,2]. Suedam et al. demonstrate that the increase of the cantilever arm, promotes an increase in stress concentration around the implant adjacent to the cantilever [27]. Furthermore, the length of the cantilever arm was significantly correlated with both biological and technical complications, in particular in implants, that lost more than 1.5 mm of bone. Palmer et al. concluded based on a 3-year prospective study that a single implant could be used to support a cantilever extension up to 8 mm [2]. Nevertheless, Rangert et al. suggested that an extension length of 10 mm was critical [25]. Generally, cantilever arm length greater than 8 mm was associated with failure category [18].
Implant characteristics
In our study, sallam et al. concluded that implant diameter has a significant influence on the stress distribution in bone because of different load transfer mechanisms and because of its diminished ability to withstand off-axial loading [14]. That was in agreement with Cehreli et al. and Matsushita et al. who stated that the use of narrow diameter implants resulted in an overall increase in stress and strain magnitudes around supporting implants [28,29]. That might be due to the smaller surface area and volume of these implants, which places more force per square millimeter against the encasing bone than do larger diameter implants, as explained by Flanagan [30].
According to some studies, the choice of a standard diameter (4mm) and a length between 8.5 and 10 mm improves the biomechanical behavior of cantilever of rehabilitation [11,15,31,32]. Moreover, it was established that the short implants have lower survival rates compared to conventional implants [32]. In addition, it has been concluded that stress distribution in implant-supported CFPDs correlated with the macro design of the implant collar. Meriç et al. showed that stresses at the veneering material decreased with microthreaded collar implant design [13].
Regarding the fixation system, Alencar et al. Compare stresses in the peri-implant bone produced by cantilevers fixed partial prostheses, when cemented or screwed onto implants [16]. They noted that the screwed prosthesis models had lower stress peaks in the peri-implant bone than the cemented models, when subjected to oblique loads, probably because screwed models have a lower tendency to bend. Screwed prostheses are also advantageous from the biological point of view, because cemented prostheses have a higher marginal microgap area, and are positioned more coronally [23,34]. However, this does not seem to influence the amount of peri-implant marginal bone loss [34].
In the studies included in this review, higher prosthetic complications occurred in models with a cantilever. However, it is important to affirm that the presence of technical complications does not necessarily compromise the longevity of the rehabilitations with a cantilever [19]. Nevertheless, requires adequate accompaniment, control of the patient situation, and efficient occlusal adjustments [1]. Reducing the occlusal table and the cusp inclination, can contribute to better stress distribution [35]. The cantilevered design of FPD should not be recommended in the subjects who have high occlusal bite forces or a history of bruxism [2]. Therefore, the patient must be advised about the possibility of mechanical complications occurring, and the cantilever being removed if necessary [19].
The use of the cantilever (mesial or distal) is suggested as an alternative, in order to avoid surgical procedures that generate more time for the treatment as well as an increase in cost and surgical morbidity. Nevertheless, there is much debate regarding the biomechanics of cantilevers, because they receive more complex stresses than conventional prostheses. Although questions still exist about their performance, when used according to defined criteria, they can be successful and have predictable results. Thus, it is important to understand how these clinical criteria affect the distribution of stresses in order to successfully design and implement cantilever prostheses. Such understanding can reduce mechanical failures and improve the longevity of these prostheses.
Adequate planning is essential. It includes the correct selection of type, number, diameter, and length of the implant, as well as the design of the prosthesis, length and location of the cantilever, and material of the prosthesis. In addition, condition of the antagonist arch, and control of masticatory force should be taken into consideration.
Furthermore, more clinical studies and RCT are necessary to determine the tension generated on prosthetic implants and components by this type of prosthesis, to produce a more complete analysis of the longevity of rehabilitations with cantilevered fixed partial prostheses.
There are no conflicts of interest
Benazouz I: Data collection, writing, and structuring the manuscript, Amine M: revising the data, giving the corrections and revising the final manuscript, Andoh A: revising the data and revising the final manuscript
- Hälg GA, Schmid J, Hämmerle CH (2008) Bone level changes at implants supporting crowns or fixed partial dentures with or without cantilevers. Clin Oral Implants Res 19: 83-990. [Crossref]
- Palmer RM, Howe LC, Palmer PJ, Wilson R (2012) A prospective clinical trial of single Astra Tech 4.0 or 5.0 diameter implants used to support two-unit cantilever bridges: Results after 3 years. Clin Oral Implants Res 23:35-40. [Crossref]
- Kunavisarut C, Lang LA, Stoner BR, Felton DA (2002) Finite element analysis on dental implant-supported prostheses without passive fit. J Prosthodont 11: 30e40. [Crossref]
- Stegaroiu R, Sato T, Kusakari H, Miyakawa O (1998) Influence of restoration type on stress distribution in bone around implants: A threedimensional finite element analysis. Int J Oral Maxillofac Implants 13: 82–90. [Crossref]
- Hutton B, Salanti G, Caldwell DM, Chaimani A, Schmid CH, et al. (2015)The PRISMA extension statement for reporting of systematic reviews incorporating network meta‑analyses of health care interventions: Checklist and explanations. Ann Intern Med 162: 777‑784. [Crossref]
- Lotti RS, Machado AW, Mazzieiro ET, Landre JJ (2006) Aplicabilidade cientıfica do m´etodo dos elementos finitos. R Dental Press Ortodon Ortop Facial 11: 35-43.
- Silva AAP, Teixeira MF (2009) Implantes curtos. Revista Implant News 6: 649-653.
- Wang C, Li Q, McClean C, Fan Y (2013) Numerical simulation of dental bone remodeling induced by implant-supported fixed partial denture with or without cantilever extension. Int J Numer Method Biomed Eng 29: 1134-1147. [Crossref]
- Yoda N, Liao Z, Chen J, Sasaki K, Swain M, et al. (2016) Role of implant configurations supporting three-unit fixed partial denture on mandibular bone response: biological-data-based finite element study. J Oral Rehab 43: 692-701. [Crossref]
- Kobari H, Yoda N, Chen J, Kawata T, Sasaki K (2016) An In Vivo Study on Load Distribution in Different Implant Configurations for Supporting Fixed Partial Dentures. Int J Oral Maxillofac Implants 31: 1049-1057. [Crossref]
- Batista VED Souza, Verri FR, Almeida DAF, Junior JFS, Lemos CAA, et al. (2017) Finite element analysis of implant-supported prosthesis with pontic and cantilever in the posterior maxilla. Comput Methods Biomech Biomed Engin 20: 663-670. [Crossref]
- Goiato MC, Shibayama R, Gennari Filho H, de Medeiros RA, Pesqueira AA, et al. (2016) Stress distribution in implant-supported prostheses using different connection systems and cantilever lengths: digital photoelasticity. J Med Eng Technol 40: 35-42. [Crossref]
- Merıç G, Erkmen E, Kurt A, Eser A, özden A (2011) Biomechanical effects of two different collar implant structures on stress distribution under cantilever fixed partial dentures. Acta Odontol Scand 69: 374-384. [Crossref]
- Sallam H, Sayed Kheiralla L, Aldawakly A (2012) Microstrains Around Standard and Mini Implants Supporting Different Bridge Designs. J Oral Implantol 38: 221-229. [Crossref]
- Borie E, Augusta Orsi I, Yoshito Noritomi P, Takanori Kemmoku D (2016) Three-Dimensional Finite Element Analysis of the Biomechanical Behaviors of Implants with Different Connections, Lengths, and Diameters Placed in the Maxillary Anterior Region. Int J Oral Maxillofac Implants. 31: 101-110. [Crossref]
- Alencar SMM, Lorenna Bastos LVN, Moura WLD, Rubo JH, Oliveira Silva TSD, et al. (2017) FEA of Peri-Implant Stresses in Fixed Partial Denture Prostheses With Cantilevers. J Prosthodont 26: 150-155. [Crossref]
- Lin D, Li Q, Li W, Swain M (2009) Dental implant induced bone remodeling and associated algorithms. J Mech Behav Biomed Mater 2: 410–432. [Crossref]
- Kim P, Ivanovski S, Latcham N, Mattheos N (2014) The impact of cantilevers on biological and technical success outcomes of implant-supported fixed partial dentures. A retrospective cohort study. Clin Oral Impl Res 25: 175–184. [Crossref]
- Freitas da Silva EV, Dos Santos DM (2018) Does the Presence of a Cantilever Influence the Survival and Success of Partial Implant-Supported Dental Prostheses ? Systematic Review and Meta-Analysis. Int J Oral Maxillofac Implants 33: 815-823. [Crossref]
- Romeo E, Tomasi C, Finini I, Casentini P, Lops D (2009) Implant-supported fixed cantilever prosthesis in partially edentulous jaws: A cohort prospective study. Clin Oral Implants Res 20: 1278–1285. [Crossref]
- Pjetursson BE, Thoma D, Jung R, Zwahlen M, Zembic A (2012) A systematic review of the survival and complication rates of implant-supported fixed dental prostheses (FDPs) after a mean observation period of at least 5 years. Clin Oral Implants Res 23: 22–38. [Crossref]
- Bruno RC, Kisch J, Larsson C (2020) Retrospective clinical evaluation of 2- to 6-unit implant-supported fixed partial dentures: Mean follow-up of 9 years. Clin Implant Dent Relat Res 22: 201-212. [Crossref]
- Romanos GE, Gupta B, Gaertner K, Nentwig GH (2014) Distal cantilever in full-arch prostheses and immediate loading: A retrospective clinical study. Int J Oral Maxillofac Implants 29: 427–431. [Crossref]
- Kreissl ME, Gerds T, Muche R, Heydecke G, Strub JR (2007) Technical complications of implant-supported fixed partial dentures in partially edentulous cases after an average observation period of 5 years. Clin Oral Implants Res 18: 720–726. [Crossref]
- Rangert B, Jemt T, Jorneus L (1989) Forces and moments on Branemark implants. Int J Oral Maxillofac Implants 4: 241–247. [Crossref]
- Romeo E, Lops D, Margutti E, Ghisolfi M, Chiapasco M, et al. (2003) Implant-supported fixed cantilever prostheses in partially edentulous arches. A seven-year prospective study. Clin Oral Implants Res 14: 303–311. [Crossref]
- Suedam V, Moretti Neto RT (2016) Effect of cantilever length and alloy framework on the stress distribution in peri-implant area of cantilevered implant-supported fixed partial dentures. J Appl Oral Sci 24: 114-120. [Crossref]
- Cehreli MC, Akca K (2004) Narrow diameter implants as terminal support for occlusal three-unit FPDs: biomechanical analysis. Int J Periodont Restor Dent 24: 513–519. [Crossref]
- Matsushita Y, Kitoh M, Zutak MI, Ikeda H, Suetsugu T (1990) Two-dimensional FEM analysis of hydroxyl apatite implants: diameter effects on stress distribution. J Oral Implantol 16: 611. [Crossref]
- Flanagan D (2008) Fixed partial dentures and crowns supported by very small diameter dental implants in compromised sites. Implant Dent 17: 182–188. [Crossref]
- Pellizzer EP, de Mello CC, Santiago Junior JF, de Souza Batista VE, de Faria Almeida DA, et al. (2015) Analysis of the biomechanical behavior of short implants: the photoelasticity method. Mater Sci Eng C Mater Biol Appl 55: 187–192. [Crossref]
- Lemos CA, Ferro-Alves ML, Okamoto R, Mendonca MR, Pellizzer EP (2016) Short dental implants versus standard dental implants placed in the posterior jaws: a systematic review and meta-analysis. J Dent 47: 8–17. [Crossref]
- Keith SE, Miller BH, Woody RD, Higginbottom FL (1999) Marginal discrepancy of screw-retained and cemented metal-ceramic crowns on implant abutments. Int J Oral Maxillofac Implants 14: 369-378. [Crossref]
- Guichet DL, Caputo AA, Choi H, Sorensen JA (2000) Passivity of fit and marginal opening in screw- or cement-retained implant fixed partial denture designs. Int J Oral Maxillofac Implants 15: 239-246. [Crossref]
- Verri FR, Batista VE, Santiago JF Jr, Almeida DA, Pellizzer EP (2014) Effect of crown-to-implant ratio on peri-implant stress: a finite element analysis. Mater Sci Eng C Mater Biol Appl 45: 234–240. [Crossref]
Editorial Information
Editor-in-Chief
Terai Masanori
Tokyo Ariake University of Medical and Health Sciences
Article Type
Research Article
Publication history
Received: December 08, 2020
Accepted: February 02, 2021
Published: February 05, 2021
Copyright
©2020 Amine M. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Citation
Amine M, Benazouz I, Andoh A (2020) The biomechanics of implant-supported cantilevered fixed partial dentures: Systematic review of the literature. Oral Health Care 5: DOI: 10.15761/OHC.1000198.