Purpose: During the COVID-19 pandemic significant behaviour change occurred in response to public health orders. As a result, the public tended to present to hospitals more acutely unwell. This study aimed to use a multidisciplinary surgical and data analytics approach to assess the outcome of delaying presentation to hospital for patients suffering from diverticulitis
Methods: All patients admitted to The Canberra Hospital, a major tertiary hospital in Australia’s south-east, with a diagnosis of diverticulitis were recruited during 2019 (the year prior to the pandemic) and from January 2020 – September 2021 (21 months during the pandemic) as a retrospective cohort. A modified Hinchey grading system was applied to the computerised tomography scans, scores of sepsis were recorded and outcomes were correlated with the time patients self-managed before presenting to hospital.
Results: There was a 27% reduction in monthly presentations for diverticulitis during the pandemic. Women were more likely to manage at home. The time from symptom onset to hospital presentation increased by 54% during the pandemic and more patients presented febrile and hypotensive. Hinchey grade distribution was not associated with the delayed presentation. The incidence of abscesses requiring drainage appeared to be higher but the numbers of patients requiring laparotomy was unchanged during the pandemic.
Conclusions: Despite the tendency for patients to self-manage their diverticular disease during the pandemic and patients presented with more signs of sepsis, the severity of disease was not worse, and the most invasive surgical procedures were not increased.
Diverticulitis, COVID-19, pandemic, surgery.
Diverticulitis is a colonic disease with a typically benign course of illness. In some cases, however, if left undiagnosed or untreated, diverticulitis may progress to a severe illness requiring significant surgical interventions. The incidence of diverticulitis has increased sharply in the last three decades, becoming one of the most common acute surgical presentations to hospitals, especially in countries where dietary fibre intake is low [1]. The condition is commonly treated by community-based practitioners [2] while surgical referral is recommended for patients with abscesses >3cm, peritonitis, those not improving with medical management, immunocompromised or highly co-morbid [3]. The treatment of diverticulitis initially involves dietary modification including clear fluids with the addition of oral antibiotics in some cases. Without resolution or if the bowel wall is breached on presentation, intravenous antibiotics are introduced, or abscesses may be drained with imaging guidance. Surgery is reserved for the most severe forms, where bowel may be resected with potential formation of a stoma [4].
During the early stages of the COVID-19 pandemic in Australia, presentations to emergency departments (ED) fell by up to 38% [5,6]. The number of presentations gradually rose but until strong vaccine rates were established, remained lower than the preceding year. Elective surgery presentations declined significantly, however the rate of urgent surgeries increased by approximately 3.5% during 2020 [5]. The extent to which delayed ED presentations or resistance to present at all, has led to adverse health outcomes is unclear, especially for diseases that may have an initial sub-acute phase but may escalate in severity as the duration from symptom onset to presentation extends. Diverticulitis is one such disease.
ED presentation figures during the pandemic indicate that the public tended to delay seeking appropriate medical attention or not present at all. However, there was an increase in the number of highly acute presentations [6]. For example, patients requiring resuscitation increased by up to 14% [5]. It was noted that during the pandemic, treatment with surgery for cancers fell and resulted in higher complication rates [7]. Globally, one in seven patients in regions experiencing full lockdowns in 61 countries either did not undergo surgery or experienced delays in pre-operative management [8]. The incidence of more acute surgical conditions such as appendicitis and cholecystitis remained stable throughout the even the most stringent lockdown periods [6].
Diverticulosis, the precursor to diverticulitis is a condition where patients who have had colonoscopy are often aware of their diagnosis and predisposition to diverticulitis, and patients may have recurrent episodes of diverticulitis that resolve with minimal intervention. Additionally, diverticulitis is a condition that is tolerable for a short period before attention is sought. This study hypothesises that during pandemic “stay at home” periods, individuals were reluctant to seek attention during episodes of diverticulitis until it became more severe which has led to worse outcomes, including surgical management or mortality.
In Australia, waves of outbreaks were responsible for changes in health seeking behaviour over many months. In The Australian Capital Territory, which geographically accounts for the majority of The Canberra Hospital’s patients, 88.3% of the over 15 population had received a double dose of the vaccine on October 24, 2021 [9-11] and freedom of movement public health restrictions had been lifted [9,10]. This study used this timepoint as the end of observation period for health-seeking behaviour during the pandemic.
During the period January 2020 to September 2021 inclusive, all patients presenting with a diagnosis of diverticulitis and admitted to The Canberra Hospital were included. Admissions with a diagnosis of diverticulitis during the calendar year of 2019 were included as a control group. One-hundred and ninety-four patients were in the study group and 151 in the control group. The modified Hinchey classification system by Wasvary et al. [12] and CT findings by Kaiser et al. [13] was applied.
Data points included in the study were: Days of illness before presentation (data was unavailable for one patient in the control group and four patients in the study group), the first recorded heart rate, temperature and systolic blood pressure on arrival at hospital, the length of admission, complications treated during the admission, readmission rates and the treatment provided (diet modification, oral and/or intravenous antibiotics, drainage of abscesses and surgical procedures).
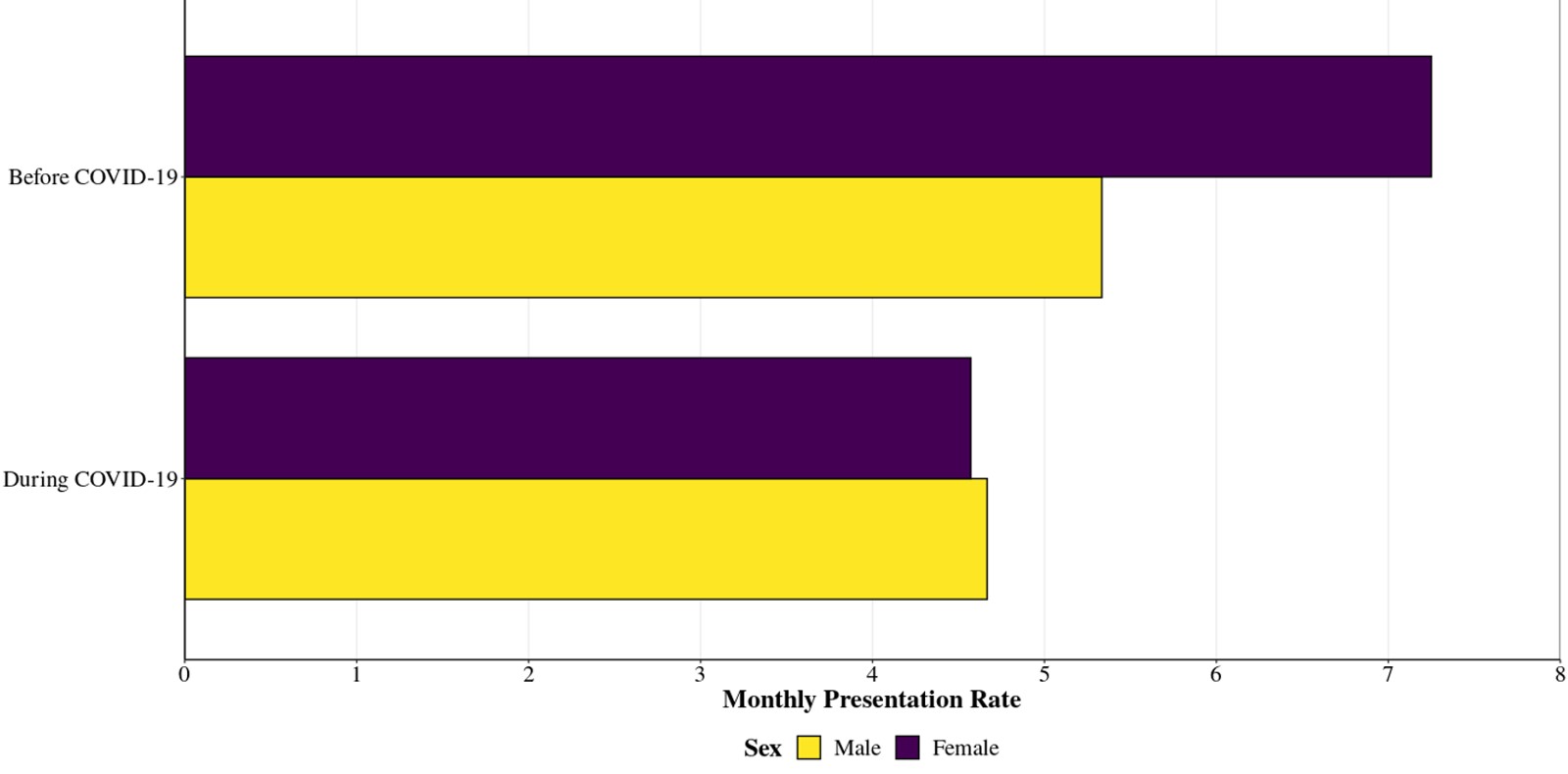
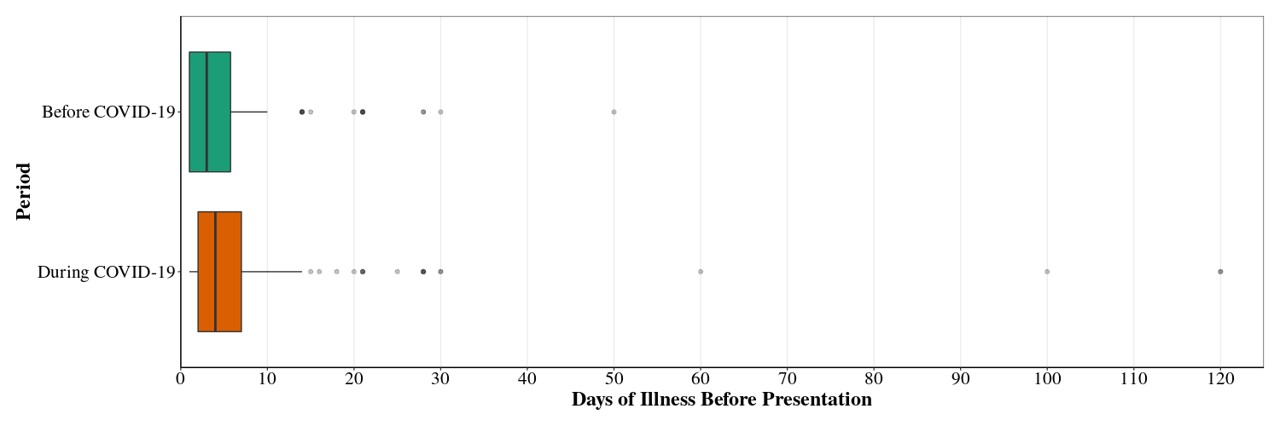
In the year preceding the pandemic, there was a 42:58 male to female ratio of patients requiring admission to the hospital for diverticulitis. During the pandemic the ratio was 50:50 reflecting a global trend for females to be more likely to delay or avoid seeking healthcare [14] (Table 1). A 27% decrease in the monthly presentations with diverticulitis was observed during the pandemic (Figure 1) and the length of time from when patients initially experienced symptoms to the time of presentation to the ED lengthened by 54% (mean 5.21 days to 8.03 days, Figure 2, Table 2).
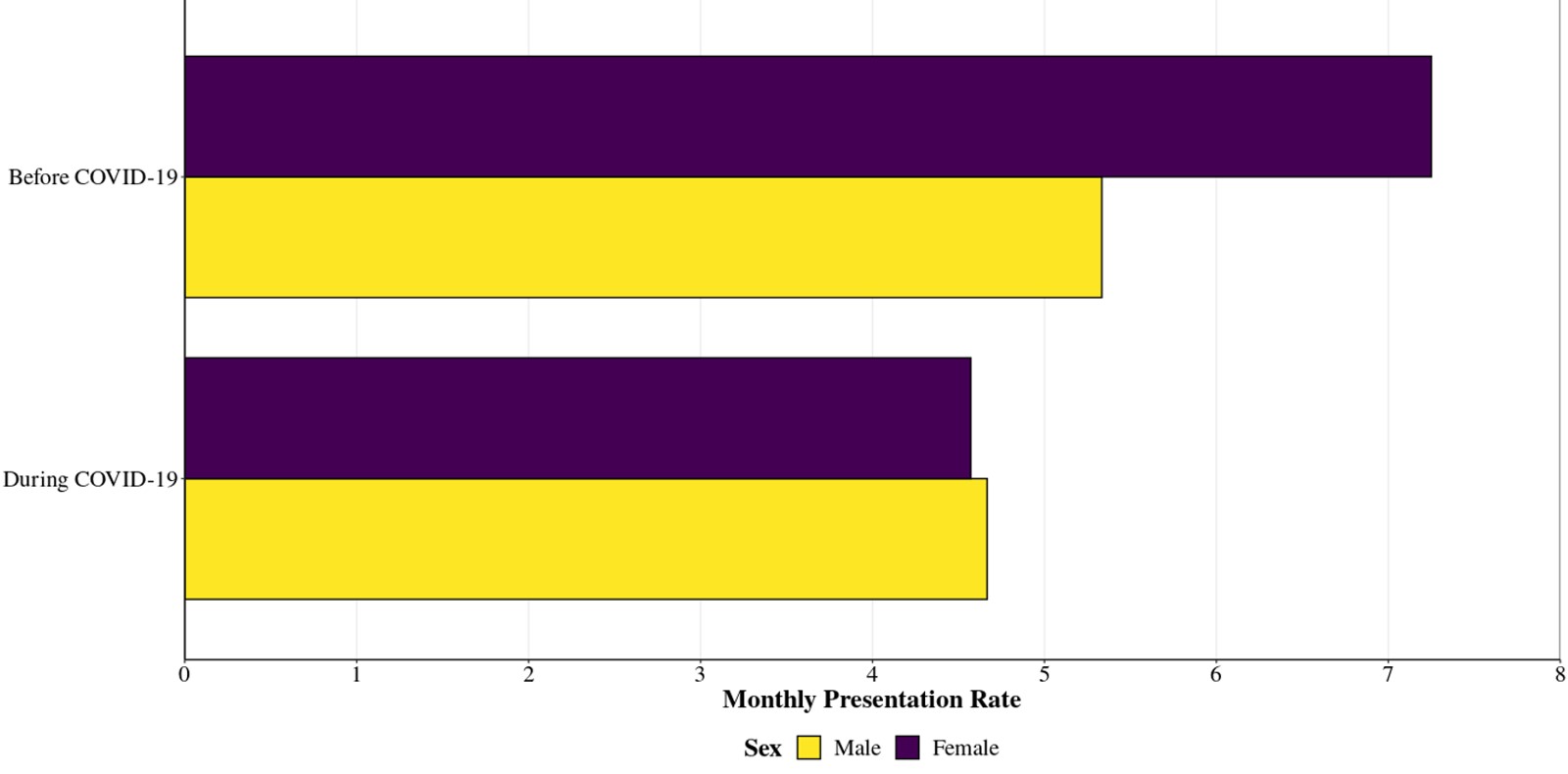
Figure 1. Average monthly rates of presentation with diverticulitis requiring admission to hospital. The ratio of female to male before the pandemic was 42:58 and during the pandemic was 49:51 suggesting females were more likely to self-manage their diverticulitis during the pandemic.
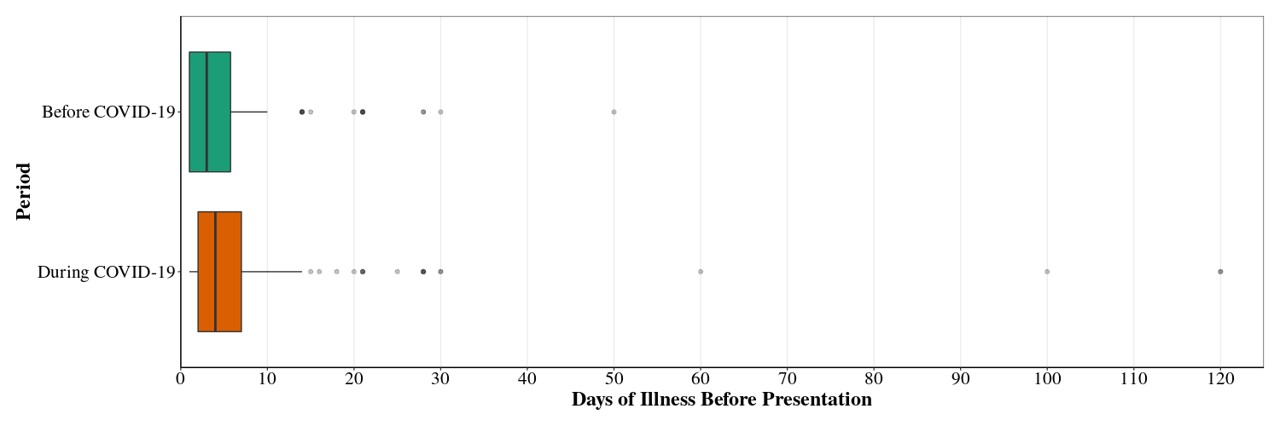
Figure 2. The median number of days of illness before presentation was increased 25% and mean of 54% (P=0.001, Wilcoxon rank sum test) during the pandemic period indicative of an overall inclination to self-manage longer and a significant minority of patients enduring a prolonged duration of symptoms.
Table 1. Patient Characteristics.
Characteristic |
Overall,
N = 345a |
Admission Date |
|
Before
COVID-19,
N = 151 |
During
COVID-19,
N = 194 |
p-value |
Sex, n (%) |
|
|
|
0.13b |
Male |
162 (47%) |
64 (42%) |
98 (51%) |
|
Female |
183 (53%) |
87 (58%) |
96 (49%) |
|
a n (%)
b Pearson's Chi-squared test
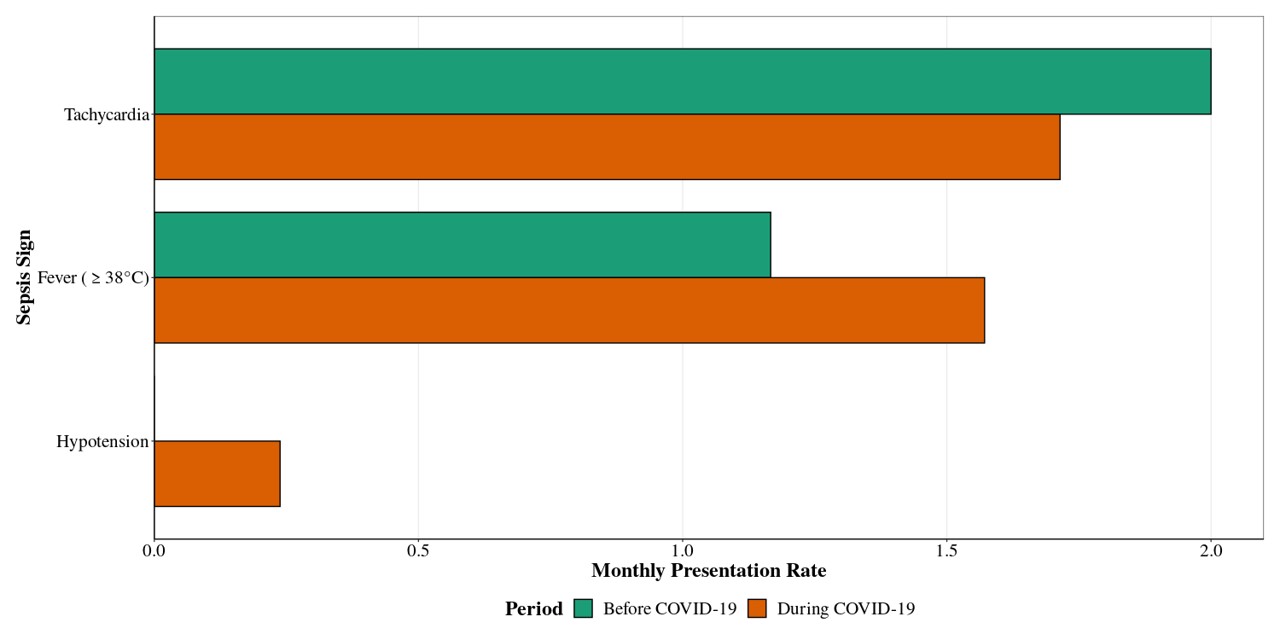
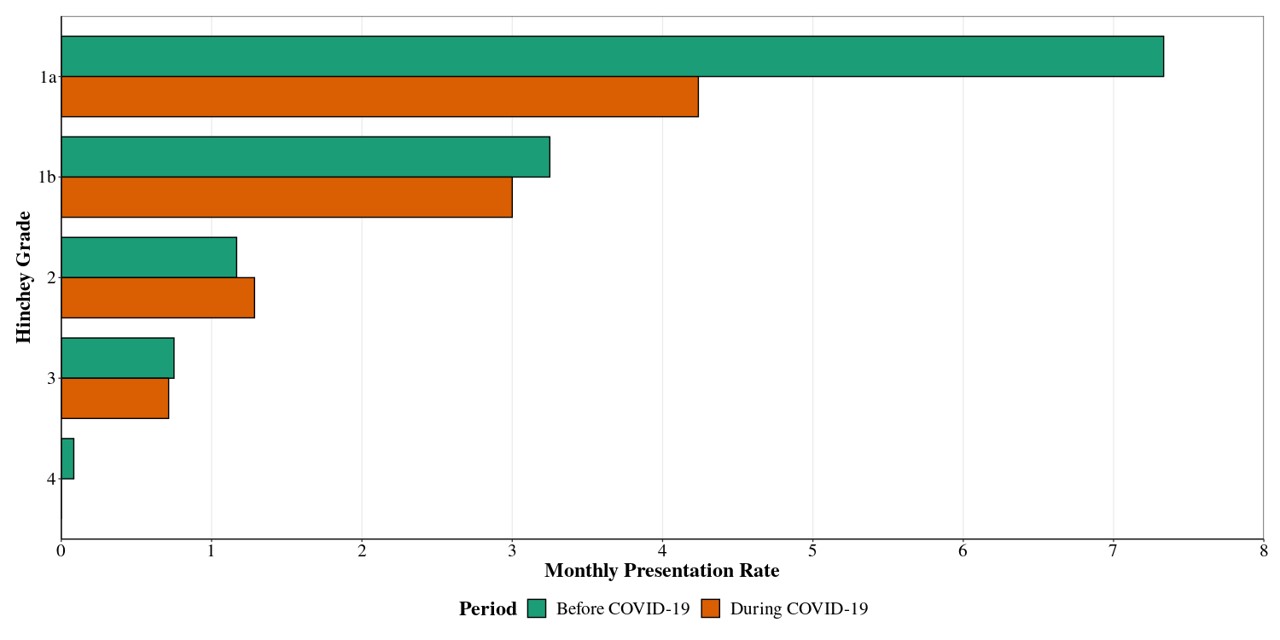
There was no statistically significant difference between the first recorded temperature and systolic blood pressure assessed during and before the pandemic (Figure 3). However, there was an increase in patients with diverticulitis who presented with a fever (>38°C, P=0.055, Table 2). Five patients during the pandemic presented with hypotension (<90mmHg systolic or >40mmHg below their usual BP) but no patients before the pandemic presented with this vital sign derangement. In addition, there was also no difference observed in the incidence of more advanced disease gauged by the modified Hinchey Classification which includes features on CT scan (Figure 4, Table 2).
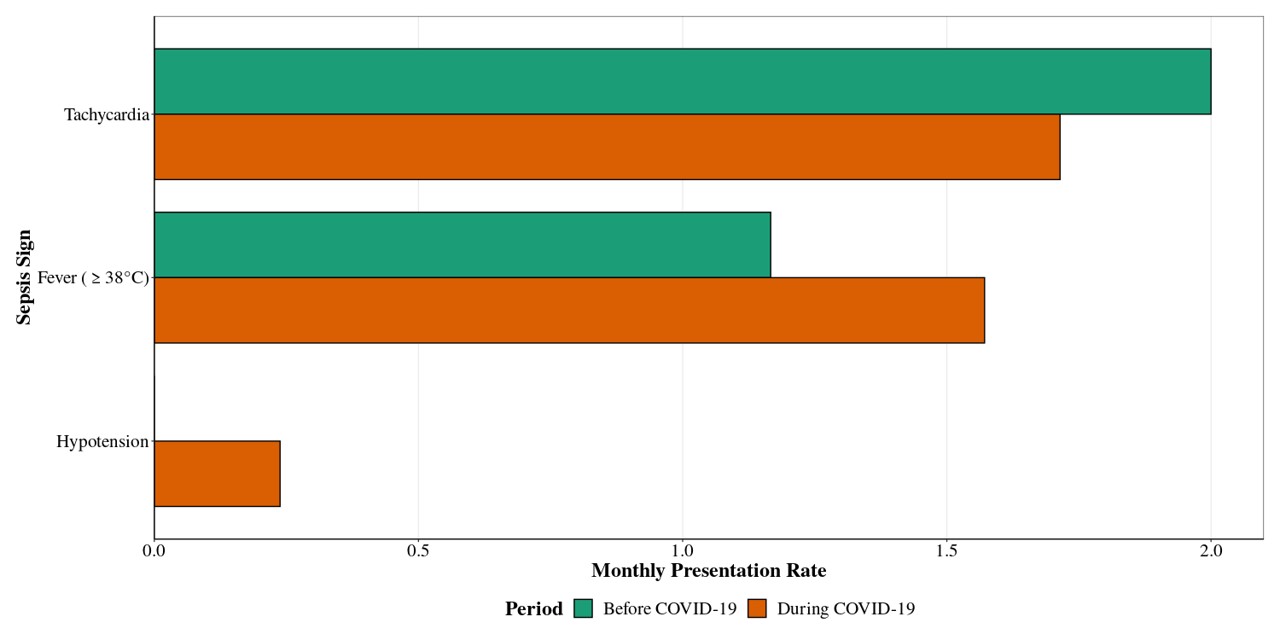
Figure 3. In line with an increase the number of days before presentation, there was a trend toward the development of signs of sepsis, particularly fever (P=0.055, two sample test for equality of proportions)
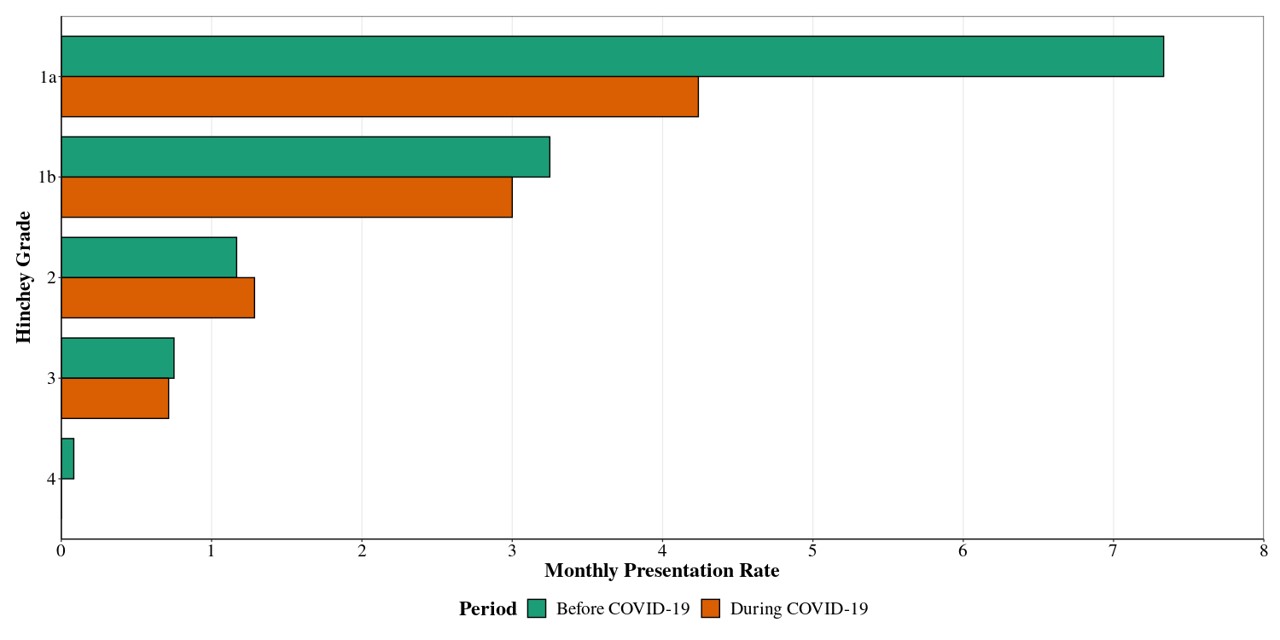
Figure 4. More severe features of diverticulitis (Hinchey Grade 1b to 4) were not observed despite delayed presentation and more evidence of systemic illness.
Table 2. Illness Severity measures.
Characteristic |
Overall,
N = 345a |
Admission Date |
|
Before
COVID-19,
N = 151 |
During
COVID-19,
N = 194 |
p-value |
Days of Illness (Before Presentation) |
|
|
|
0.001b |
Mean (SD) |
6.79 (12.45) |
5.21 (6.97) |
8.03 (15.37) |
|
Median (IQR) |
3 (2, 7) |
3 (1, 5.75) |
4 (2, 7) |
|
Range |
1, 120 |
1, 50 |
1, 120 |
|
Unknown |
5 |
1 |
4 |
|
Sepsis Sign - Tachycardia, n (%) |
60 (17%) |
24 (16%) |
36 (19%) |
0.6c |
Sepsis Sign - Fever (≥ 38°C), n (%) |
47 (14%) |
14 (9.3%) |
33 (17%) |
0.055c |
Sepsis Sign - Systolic <90mmHg or >40mmHg drop from normal, n (%) |
5 (1.4%) |
0 (0%) |
5 (2.6%) |
0.13c |
Hinchey Grade, n (%) |
|
|
|
0.12d |
1a |
177 (51%) |
88 (58%) |
89 (46%) |
|
1b |
102 (30%) |
39 (26%) |
63 (32%) |
|
2 |
41 (12%) |
14 (9.3%) |
27 (14%) |
|
3 |
24 (7.0%) |
9 (6.0%) |
15 (7.7%) |
|
4 |
1 (0.3%) |
1 (0.7%) |
0 (0%) |
|
a Mean (SD), Median (IQR), Range; n (%)
b Wilcoxon rank sum test
c Two sample test for equality of proportions
d Fisher's exact test
Abscesses requiring drainage did show a trend towards a higher rate during the pandemic (10% vs 6%) of all admissions for diverticulitis (P=0.10, Table 3). A larger sample size combining results from several centres may demonstrate a significant difference. However, no difference was observed between the incidence of laparotomies performed including Hartmann’s procedures and anterior resections. There was no difference in the mean or median length of stay in the 2 groups (Table 3). The rate of readmission to hospital within 30 days was also comparable (Table 4).
Table 3. Patient Outcomes.
Characteristic |
Overall,
N = 345a |
Admission Date |
|
Before
COVID-19,
N = 151 |
During
COVID-19,
N = 194 |
p-value |
Surgical Interventions, n (%) |
|
|
|
0.5b |
Abscess Drainage |
29 (8.4%) |
9 (6.0%) |
20 (10%) |
|
Anterior Resection |
7 (2.0%) |
4 (2.6%) |
3 (1.5%) |
|
Diagnostic Laparoscopy |
1 (0.3%) |
1 (0.7%) |
0 (0%) |
|
Hartmann’s Procedure |
26 (7.5%) |
11 (7.3%) |
15 (7.7%) |
|
Laparotomy and Bowel Resection |
1 (0.3%) |
0 (0%) |
1 (0.5%) |
|
None |
281 (81%) |
126 (83%) |
155 (80%) |
|
Length of Stay |
|
|
|
0.5c |
Mean (SD) |
4.40 (5.32) |
4.66 (6.30) |
4.21 (4.43) |
|
Median (IQR) |
3 (2, 5) |
3 (2, 5) |
3 (2, 5) |
|
Range |
0, 52 |
0, 52 |
0, 36 |
|
a n (%); Mean (SD), Median (IQR), Range
b Fisher's exact test
c Wilcoxon rank sum test
Table 4. Readmission rate.
Characteristic |
Overall,
N = 345a |
Admission Date |
|
Before
COVID-19,
N = 151 |
During
COVID-19,
N = 194 |
p-value |
Readmission Episode, n (%) |
|
|
|
0.2b |
Single Admission |
299 (82%) |
136 (86%) |
163 (80%) |
|
Readmission |
64 (18%) |
23 (14%) |
41 (20%) |
|
a n (%)
b Pearson's Chi-squared test
Presentation to EDs during the COVID-19 pandemic with urgent and semi-urgent issues were reduced across the globe [15,16] and this led to a likely increase in total excess mortality not related to the pandemic [17]. In Australia, urgent presentations (those requiring attention within 30 minutes of arrival) fell by 4% during 2020 and only returned to pre-pandemic levels in 2021 despite a trend towards overall increase by approximately 5% per year over the last 10 years [18]. Most studies of hospital presentations have focussed on changes during outbreaks but the pandemic has been a significant force behind hesitative behaviour and motivation even when the most stringent public health measures were lifted [19]. There is little known about the implications for overall disease burden because of prolonged periods of reduced healthcare seeking behaviour. This study utilises a surgical condition to model the effect of reduced healthcare seeking behaviour during the pandemic on longer term outcomes to assess whether delaying treatment and self-management has led to more significant pathology and a need for more serious interventions.
In Australia, access to healthcare did not change during the pandemic, a feature of some overseas experiences, suggesting that patients were delaying or avoiding seeking care by volition. Vulnerable groups including female sex, fragile self-appreciated health, and high levels of depression and anxiety were identified as traits commonly associated with avoiding healthcare [14]. Specifically, patients who feared contracting COVID-19 or who believe they would be less likely to overcome a severe infection due to their poor perceived health were not seeking attention [20,21].
Consistent with the global trend, females appeared to be more reluctant than males to present to the ED with diverticulitis during the pandemic in this study. This may be explained by the observation that diverticulitis has a female predominance in older patients (2:1 in over age 45) [22] and a male predominance in younger patients (3:1 in under age 45) [22,23] and COVID-19 has a higher mortality associated with older individuals potentially acting as a more significant deterrent to female presentation.
Diverticulitis is often self-limiting [1]. Transient symptoms of diverticulitis, similar to other conditions like cerebrovascular or cardiovascular events, may herald a more sinister underlying pathology resulting in significant health consequences if left untreated. During the pandemic this study showed that the median time before patients presented after symptom onset with diverticulitis increased by 25% and the mean by 54%. These figures suggest that even the most anxious to receive treatment were delaying presentation and a small group of individuals were persisting with self-management for weeks or even months before presenting.
Patients presenting with diverticulitis requiring admission to hospital (Hinchey grade >0, immunosuppressed, comorbid) declined by 27% during the pandemic. It was clear from previous studies of diverticulitis that presentations during the peak of the COVID-19 lockdowns in March – June 2020 were sharply decreased [24] and the proportion of patients presenting with CT findings suggestive of more severe disease (i.e. Abscess) may have been approximately double [25]. Although these findings are significant, they focus on the early weeks of the pandemic. This study takes a longer view of the pandemic and demonstrates that this reluctance persisted even when more austere public health orders were lifted.
The incidence of certain high acuity conditions including surgical issues such as appendicitis were reported to be lower during the pandemic across the globe [26-29] but the incidence of patients presenting acutely unwell was variable [6,30]. In this study, measures of sepsis including heart rate, temperature and blood pressure, when combined, showed no significant difference during the pandemic for patients with diverticulitis despite a median increase in the number of days before presentation. There was, however, an increase in the number of patients presenting with fever.
Despite the delay in presentation and overall reduction in incidence of hospitalisation for diverticulitis suggesting that patients were opting for self-management, there was no difference in the grade of disease, the acuity of illness or the likelihood of requiring the most invasive surgical procedures during the 21-month pandemic, observation period. There was a trend towards an increase in the rate of patients requiring drainage of abscesses but not for laparotomies. Larger studies would be required to confirm these trends.
By demonstrating that self-management or more active community physician management of diverticulitis during the pandemic did not increase the risk of more severe disease and more complex surgical interventions, the study also suggests that hospital-based care may safely be reduced even for more complicated diverticulitis when the pandemic ends.
A cost-benefit analysis involving the costs of delayed presentation to hospital for an acute surgical issue like diverticulitis in this study during the pandemic and the benefit of strong public health messaging that results in behaviour change strongly supports the public health messaging adopted in Australia. Although previous studies on the topic showed an increase in disease severity during the peak infection periods, the findings in this study, which includes peak infection periods and many months after, suggest that this likely does not apply in the long run. The suppression policy in Australia resulted in comparatively low case numbers, severe illness, and deaths related to COVID-19 and appears not to have impacted significantly on acute surgical outcomes.
No funding was sought for the study.
The authors declare no competing interests.
- Weizman AV, Nguyen GC (2011) Diverticular disease: epidemiology and management. Can J Gastroenterol 25: 385-389. [Crossref]
- Mizuki A, Nagata H, Tatemichi M, Kaneda S, Sukada N, et al. (2005) The out-patient management of patients with acute mild-to-moderate colonic diverticulitis. Aliment Pharmacol Ther 21: 889-897. [Crossref]
- Feingold D, Steele SR, Lee S, Kaiser A, Boushey R, et al. (2014) Practice parameters for the treatment of sigmoid diverticulitis. Dis Colon Rectum 57: 284-294. [Crossref]
- Nagorney DM, Adson MA, Pemberton JH (1985) Sigmoid diverticulitis with perforation and generalized peritonitis. Dis Colon Rectum 28: 71-75. [Crossref]
- AIHW (2020) Australia's health performance. Covid-19 and looking back on health 2020.
- Kam AW, Chaudhry SG, Gunasekaran N, Jr White A, Vukasovic M, et al. (2020) Fewer presentations to metropolitan emergency departments during the COVID-19 pandemic. Med J Aust 213: 370-371. [Crossref]
- COVIDSurg Collaborative (2020) Outcomes from elective colorectal cancer surgery during the SARS-CoV-2 pandemic. Colorectal Dis [Crossref]
- COVIDSurg Collaborative (2021) Effect of COVID-19 pandemic lockdowns on planned cancer surgery for 15 tumour types in 61 countries: an international, prospective, cohort study. Lancet Oncol 22: 1507-1517.
- Health A (2021) ACT reaches 80% of eligible population fully vaccinated: ACT Business Hub.
- Government A (2021) Operation Covid shield vaccine sentiment summary. In: Health Do.
- Government A (202) COVID-19 vaccination – Geographic vaccination rates – SA4 – 25 October 2021. In: Health Do.
- Wasvary H, Turfah F, Kadro O, Beauregard W (1999) Same hospitalization resection for acute diverticulitis. Am Surg 65: 632-635. [Crossref]
- Kaiser AM, Jiang JK, Lake JP, Ault G, Artinyan A, et al. (2005) The management of complicated diverticulitis and the role of computed tomography. Am J Gastroenterol 100: 910-917. [Crossref]
- Splinter MJ, Velek P, Ikram MK, Kieboom BCT, Peeters RP, et al. (2021) Prevalence and determinants of healthcare avoidance during the COVID-19 pandemic: A population-based cross-sectional study. PLoS Med 18: e1003854.
- Lange SJ, Ritchey MD, Goodman AB, Dias T, Twentyman E, et al. (2020) Potential indirect effects of the COVID-19 pandemic on use of emergency departments for acute life-threatening conditions - United States, January-May 2020. Am J Transplant 20: 2612-2617. [Crossref]
- Collyer TA, Athanasopoulos G, Srikanth V, Tiruvoipati R, Matthews C, et al. (2021) Impact of COVID-19 lockdowns on hospital presentations and admissions in the context of low community transmission: evidence from time series analysis in Melbourne, Australia. J Epidemiol Community Health jech-2021-217010. [Crossref]
- New York City Department of Health and Mental Hygiene (DOHMH) COVID-19 Response Team (2020) Preliminary Estimate of Excess Mortality During the COVID-19 Outbreak - New York City, March 11-May 2, 2020. MMWR Morb Mortal Wkly Rep 69: 603-605.
- AIHW (2021) Emergency Department Care. In: Health Do, ed.
- Saladino V, Algeri D, Auriemma V (2020) The Psychological and Social Impact of Covid-19: New Perspectives of Well-Being. Front Psychol 11: 577684. [Crossref]
- Taylor S, Landry CA, Paluszek MM, Rachor GS, Asmundson GJG (2020) Worry, avoidance, and coping during the COVID-19 pandemic: A comprehensive network analysis. J Anxiety Disord 76: 102327. [Crossref]
- Taylor S, Landry CA, Paluszek MM, Asmundson GJG (2020) Reactions to COVID-19: Differential predictors of distress, avoidance, and disregard for social distancing. J Affect Disord 277: 94-98.
- Lahat A, Menachem Y, Avidan B, Yanai H, Sakhnini E, et al. (2006) Diverticulitis in the young patient--is it different? World J Gastroenterol 12: 2932-2935. [Crossref]
- Warner E, Crighton EJ, Moineddin R, Mamdani M, Upshur R (2007) Fourteen-year study of hospital admissions for diverticular disease in Ontario. Can J Gastroenterol 21: 97-99. [Crossref]
- Hossain N, Naidu V, Hosny S, Khalifa M, Mathur P, et al. (2022) Hospital Presentations of Acute Diverticulitis During COVID-19 Pandemic may be More Likely to Require Surgery due to Increased Severity: A Single-Centre Experience. Am Surg 88: 133-139. [Crossref]
- Zintsmaster MP, Myers DT (2021) Patients avoided important care during the early weeks of the coronavirus pandemic: diverticulitis patients were more likely to present with an abscess on CT. Emerg Radiol 28: 279-282. [Crossref]
- De Filippo O, D'Ascenzo F, Angelini F, Bocchino PP, Conrotto F, et al. (2020) Reduced Rate of Hospital Admissions for ACS during Covid-19 Outbreak in Northern Italy. N Engl J Med 383: 88-89. [Crossref]
- Morelli N, Rota E, Terracciano C, Immovilli P, Spallazzi M, et al. (2020) The Baffling Case of Ischemic Stroke Disappearance from the Casualty Department in the COVID-19 Era. Eur Neurol 83: 213-215. [Crossref]
- Rosenbaum L (2020) The Untold Toll - The Pandemic's Effects on Patients without Covid-19. N Engl J Med 382: 2368-2371. [Crossref]
- Orthopoulos G, Santone E, Izzo F, Tirabassi M, Pérez-Caraballo AM, et al. (2021) Increasing incidence of complicated appendicitis during COVID-19 pandemic. Am J Surg 221: 1056-1060. [Crossref]
- Hughes HE, Hughes TC, Morbey R, Challen K, Oliver I, et al. (2020) Emergency department use during COVID-19 as described by syndromic surveillance. Emerg Med J 37: 600-604.
Editorial Information
Editor-in-Chief
Kleanthis Giannoulis
Thessaloniki School of Medicine, Greece
Article Type
Research article
Publication history
Received: January 31, 2022
Accepted: February 11, 2022
Published: February 14, 2022
Copyright
©2022 Whiley PJ. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Citation
Whiley PJ, Voo TV (2022) The impact of delayed acute diverticulitis presentations during the COVID-19 pandemic on acuity and surgical complexity in the long-term. Glob Surg 8: DOI:10.15761/GOS.1000239.
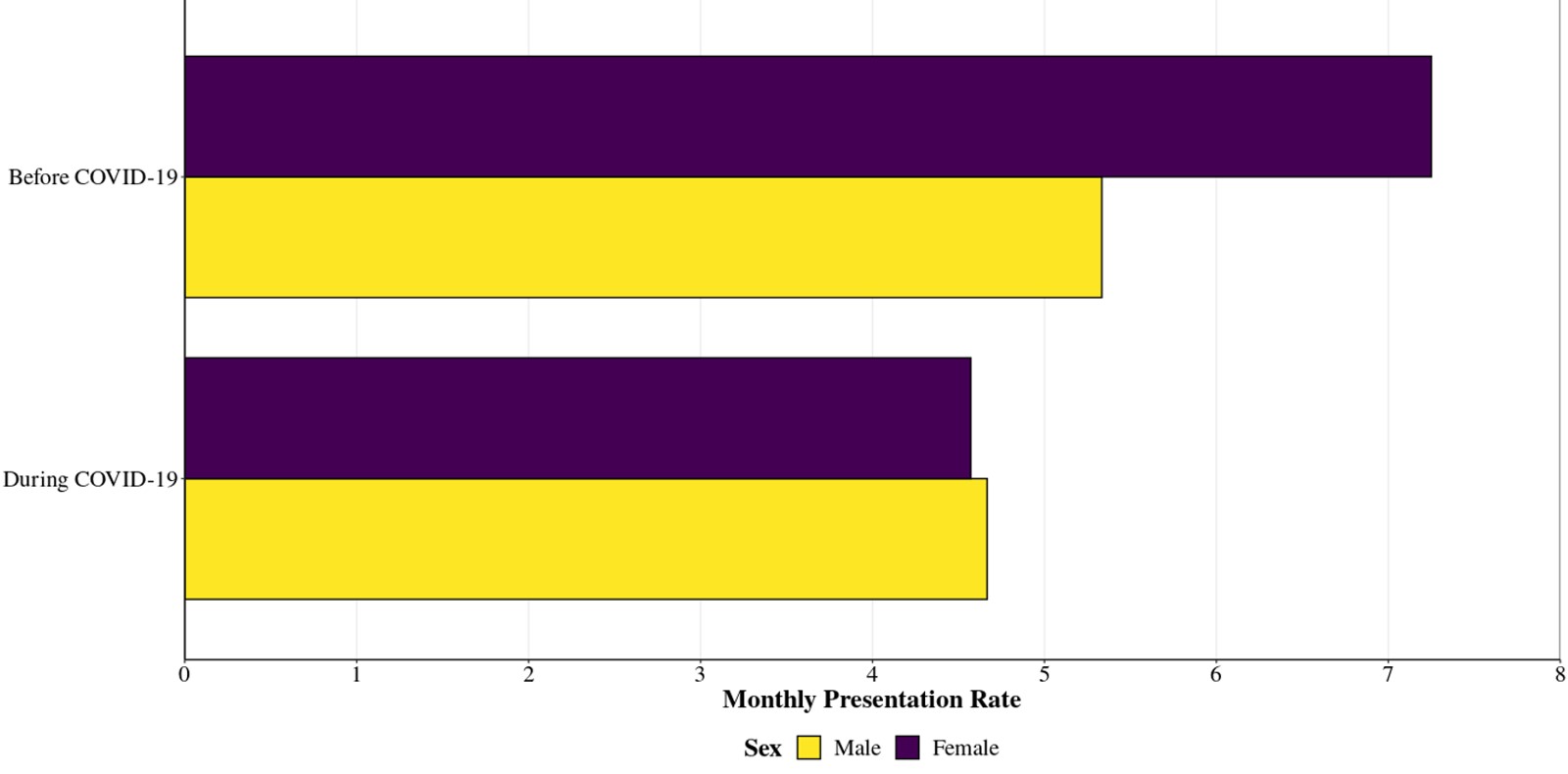
Figure 1. Average monthly rates of presentation with diverticulitis requiring admission to hospital. The ratio of female to male before the pandemic was 42:58 and during the pandemic was 49:51 suggesting females were more likely to self-manage their diverticulitis during the pandemic.
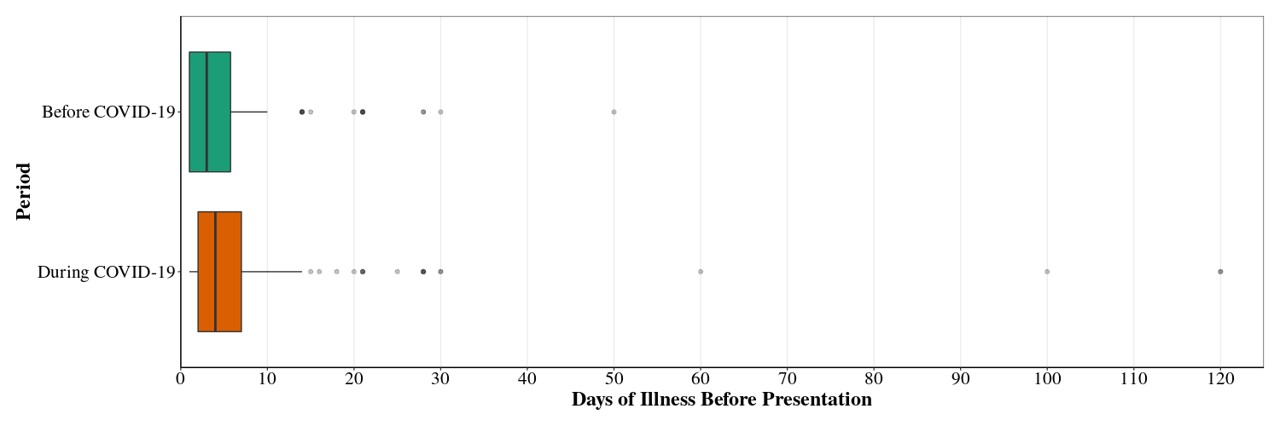
Figure 2. The median number of days of illness before presentation was increased 25% and mean of 54% (P=0.001, Wilcoxon rank sum test) during the pandemic period indicative of an overall inclination to self-manage longer and a significant minority of patients enduring a prolonged duration of symptoms.
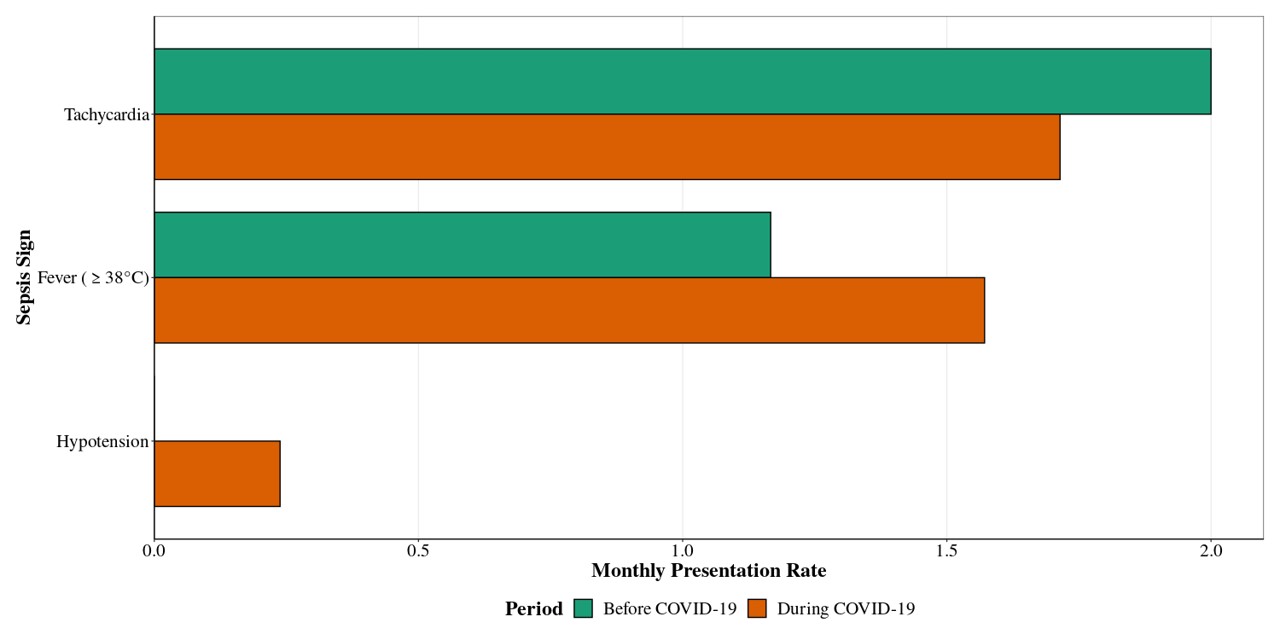
Figure 3. In line with an increase the number of days before presentation, there was a trend toward the development of signs of sepsis, particularly fever (P=0.055, two sample test for equality of proportions)
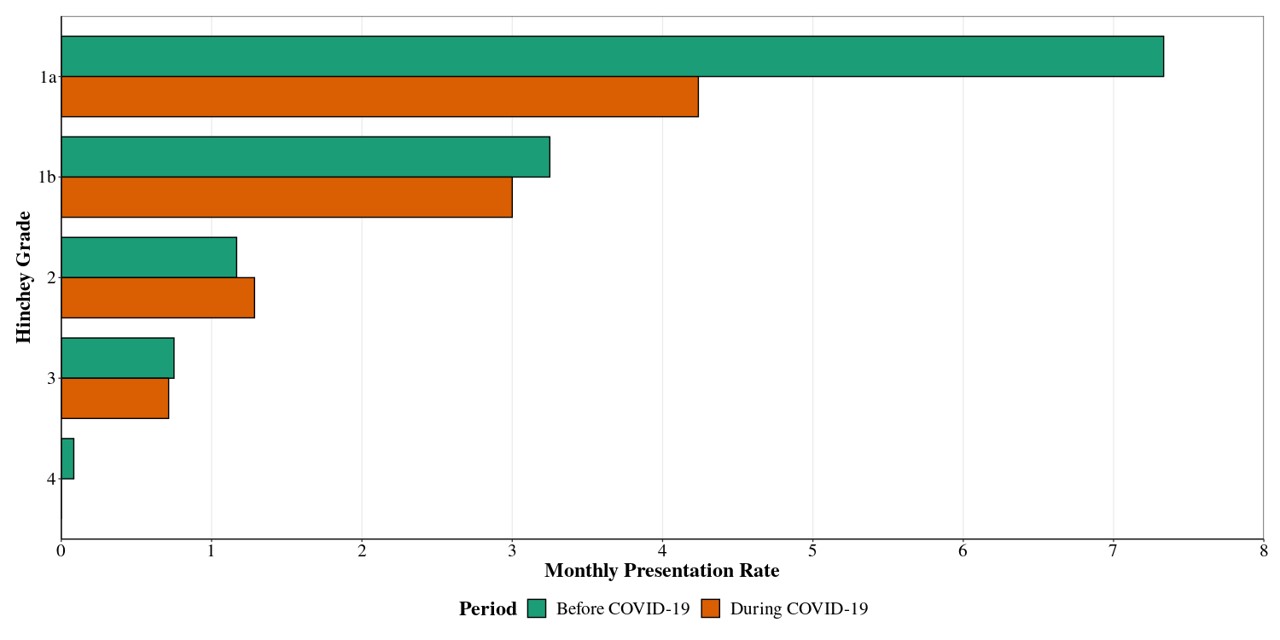
Figure 4. More severe features of diverticulitis (Hinchey Grade 1b to 4) were not observed despite delayed presentation and more evidence of systemic illness.
Table 1. Patient Characteristics.
Characteristic |
Overall,
N = 345a |
Admission Date |
|
Before
COVID-19,
N = 151 |
During
COVID-19,
N = 194 |
p-value |
Sex, n (%) |
|
|
|
0.13b |
Male |
162 (47%) |
64 (42%) |
98 (51%) |
|
Female |
183 (53%) |
87 (58%) |
96 (49%) |
|
a n (%)
b Pearson's Chi-squared test
Table 2. Illness Severity measures.
Characteristic |
Overall,
N = 345a |
Admission Date |
|
Before
COVID-19,
N = 151 |
During
COVID-19,
N = 194 |
p-value |
Days of Illness (Before Presentation) |
|
|
|
0.001b |
Mean (SD) |
6.79 (12.45) |
5.21 (6.97) |
8.03 (15.37) |
|
Median (IQR) |
3 (2, 7) |
3 (1, 5.75) |
4 (2, 7) |
|
Range |
1, 120 |
1, 50 |
1, 120 |
|
Unknown |
5 |
1 |
4 |
|
Sepsis Sign - Tachycardia, n (%) |
60 (17%) |
24 (16%) |
36 (19%) |
0.6c |
Sepsis Sign - Fever (≥ 38°C), n (%) |
47 (14%) |
14 (9.3%) |
33 (17%) |
0.055c |
Sepsis Sign - Systolic <90mmHg or >40mmHg drop from normal, n (%) |
5 (1.4%) |
0 (0%) |
5 (2.6%) |
0.13c |
Hinchey Grade, n (%) |
|
|
|
0.12d |
1a |
177 (51%) |
88 (58%) |
89 (46%) |
|
1b |
102 (30%) |
39 (26%) |
63 (32%) |
|
2 |
41 (12%) |
14 (9.3%) |
27 (14%) |
|
3 |
24 (7.0%) |
9 (6.0%) |
15 (7.7%) |
|
4 |
1 (0.3%) |
1 (0.7%) |
0 (0%) |
|
a Mean (SD), Median (IQR), Range; n (%)
b Wilcoxon rank sum test
c Two sample test for equality of proportions
d Fisher's exact test
Table 3. Patient Outcomes.
Characteristic |
Overall,
N = 345a |
Admission Date |
|
Before
COVID-19,
N = 151 |
During
COVID-19,
N = 194 |
p-value |
Surgical Interventions, n (%) |
|
|
|
0.5b |
Abscess Drainage |
29 (8.4%) |
9 (6.0%) |
20 (10%) |
|
Anterior Resection |
7 (2.0%) |
4 (2.6%) |
3 (1.5%) |
|
Diagnostic Laparoscopy |
1 (0.3%) |
1 (0.7%) |
0 (0%) |
|
Hartmann’s Procedure |
26 (7.5%) |
11 (7.3%) |
15 (7.7%) |
|
Laparotomy and Bowel Resection |
1 (0.3%) |
0 (0%) |
1 (0.5%) |
|
None |
281 (81%) |
126 (83%) |
155 (80%) |
|
Length of Stay |
|
|
|
0.5c |
Mean (SD) |
4.40 (5.32) |
4.66 (6.30) |
4.21 (4.43) |
|
Median (IQR) |
3 (2, 5) |
3 (2, 5) |
3 (2, 5) |
|
Range |
0, 52 |
0, 52 |
0, 36 |
|
a n (%); Mean (SD), Median (IQR), Range
b Fisher's exact test
c Wilcoxon rank sum test
Table 4. Readmission rate.
Characteristic |
Overall,
N = 345a |
Admission Date |
|
Before
COVID-19,
N = 151 |
During
COVID-19,
N = 194 |
p-value |
Readmission Episode, n (%) |
|
|
|
0.2b |
Single Admission |
299 (82%) |
136 (86%) |
163 (80%) |
|
Readmission |
64 (18%) |
23 (14%) |
41 (20%) |
|
a n (%)
b Pearson's Chi-squared test