Background: Prophylactic drainage after elective Anterior
resections with stapled colorectal or colo-anal anastomosis decreases neither
the rate of cases with one or more post-operative complications maybe impacted
by drainage nor the complications severity.
Aim and objectives: This study aimed for comparing cases who
experienced routine pelvic drainage with those who didn’t regarding the
complication rate and severity thereafter elective anterior resection (AR).
Subjects and methods: Retrospective cohort study, 54 cases were
arbitrarily allocated into the pelvic drainage group and 29 to the no pelvic
drainage group. All 83 anastomoses were examined for air-tightness
intra-operatively and mended if leak was detected.
Results: This study shows that a statistically significant
change was found among the study groups as (With drainage and Without drainage)
regarding cardiovascular dis, HTN, IHD, drain, open/Lap, covering stoma and mean
mortality during hospital stay.
No significant change statistically was found among the study groups as (With
drainage and Without drainage) as regard post op leak, localized abscess
(infected haematoma), and mortality during hospital stay.
Conclusion: Routine pelvic drainage after elective anterior
resection does not reduce the rate or severity of anastomotic leak. It may,
infrequently, be harmful.
Prophylactic drainage, anterior resection, complications, anastomotic leakage.
The colonic lumen comprises from 108 to 1010 aerobic and
an-aerobic germs /gm of feces. This may clarify why post-operative infectious
complication, the occurrence of it ranged between 10 and 70%, can be more in
cases underwent operations of the colon than in those underwent any other
abdominal operations. Anastomotic leakages are the main reasons of
post-operative infectious complications, accountable for 25- 35% of mortalities
[1].
The Guidelines for Avoidance of Surgical Site Infections (SSIs), made by the
Centers for Diseases Controlling and Preventions (CDC) in 1999, indorses that
‘If drainage is essential, utilize a locked suction drains and eliminate
the drains once it possible’. New RCTs and
metanalyses have maintained the
restricted usage of prophylactic
intraabdominal drainages for several gastro-intestinal operations [2].
Numerous events were defined to reduce the post-operative complications rate and
the severity, particularly infectious side-effects, in addition to the reduction
anastomotic leakages. These comprise anti-biotic prophylaxis, anti-septic
mechanical preparations, diverting stomas, omental wrapping round the
anastomosis, and intra operative air- tightness test resulting in comprehensive
anastomotic air-tightness integrities [3].
The majority of surgeons were supporter repetitive usage of drains after pelvic
anastomose. Proponentes of this maintain that they permit egress of fluids
collection that have the possibility of becoming infected, permit early
recognition of anastomotic dehiscence, and do no harm. Objectors to the use
argue that it can impede healing of the anastomoses confer no benefit and may
cause harm. A recent RCT of pelvic drainage thereafter rectal ressection
suggested that a pelvic drain thereafter rectal resections didn’t present
any advantage to the patients [4].
The prophylactic drainages of the abdomen space were suggested for these same
causes in 1950th. Prophylactic drainage is supposed to (1) reduce the
rate of anastomotic leakages by the evacuation of serositis and blood that, once
contaminated, may cause sore formations and
hole of the abscess
into the inosculation; (2)
reduce the complication severity via early
diagnosing; and (3) ease the diagnosing
of intra- peritoneal hemorrhage [5].
In contrast, surgeons who are opposite to drainage trust that it (1) really
excites the formations of serous fluids; (2) may result in infections from
exterior; (3) rises the rate of leakages via avoiding the mobilizations of
omentum and neighboring organs, obstructing their closing action on the
anastomotic sutures or even making leak by mechanically erosion of the
inosculation; and (4) is enclosed off rapidly [6]. Suction drainages can (1)
reduce the quantity of infection coming from exterior by preserving -ve pressure
on the tissue, (2) be accompanying with lesser post-operative adherences, (3) be
accompanying with lesser anastomotic leakages, and (4) be encapsulated less
rapidly. Suction drainages was utilized in 1 of the RCTs, while non-suction
drainages were utilized in the other [7].
We, consequently, performed a great, multi-center,
prospective, controlled by randomization, to find out (1) whether prophylactic
drainages reduced the complication severity and rate ultimately connected to
drainages, thereafter colonic resections followed directly by intraabdominal
suprapromontory colonic inosculation; and (2) whether one kind of drains
(suctions or non-suction) was better than the other.
83 cases with ages mean of 67 years (22-95) enrolled in this work
from (December 2020 to December 2021). Data collections of all cases was
completed but all the cases weren’t enrolled in the research at similar
time.
Sample size: As mean length of hospital stays due to
complications in drainage group 24.5+/-1.89 compared to 26.1+/-2.87 in
non-drainage group [2]. So, sample size is 74. Sample was increased 10% to avoid
follow up bias and to be 83. Sample has been estimated via Open Epi program with
95 % confidence and 80% power methods.
Colonic Preparations: All cases experienced colonic
mechanically preparations, counting the administrations of laxatives
(sennosides) or poly-ethylene glycol, that comprised the administrations of
enemas which were applied at 6 PM and in the morning (3 h) preoperatively. All
cases have a 1-dosage mixture of systemic ceftriaxone sodium and metronidazole
at anesthesia inductions.
Resections and Anastomosis: Mechanical bowel preparations has
been performed in all cases the day pre-operation. Colorectal inosculation
stapled by means of linear stapling device. AII colorectal inosculates were
performed by means of a circular stapling instrument and were intra-operatively
examined by trans-anal air insufflations. The intestine was unfocussed by a
defensive loop ileostomy in 38 cases of 53 cases who had pelvic drains and 12
cases out of 30 in no drainage group for rectal resection with whole mesorectal
excisions and coloanal inosculation in cases with lower rectal tumor.
Testing for Airtightness: The contributing physicians were
requested to examine for airtightness by observing bubbles appearance when the
colon barrier was swollen with air inserted into the colonic lumens, and digits
located on two sides of colorectal or colo- anal anastomoses, or by a
balloon-overstated Foley catheter introduced via the anus for distal colorectal
inosculates clamped proximally. If anastomotic leak was observed,
additional sutures were added till comprehensive airtightness was attained.
Random Allotment: After the resections and inosculation were
accomplished and confirmed for airtightness, cases experienced drainages (D+) or
not (D−), as shown below the creased upper right corner of questionnaires
rather than the envelopes technique. Cases have been located in D+. Arbitrary
allocation was stable via blocks of four in every center. This work was accepted
by the ethics committee of the coordination center.
Drainage: A locked drainage system of silastic has been utilized
in all patients, no suctions has been used. The diameter of drainage was 24 Ch.
End Points: The initially end point was the percent of cases
with 1 or more post- operative complications
ultimately connected to drainages, counting
(1) Deep complication that maybe impacted by drainages and for which drainages
can cause earlier diagnosing, counting anastomotic leakages, general or local
peritonitis, intraabdominal haemorrhage, or haematoma. Anastomotic leakages were
detected via the egress of fecal fluids via drain, by a following
procedure or an autopsy (accomplished regularly for all cases who passed away in
hospital). The post-operative interval comprised the total hospitalization,
regardless of its period, and the 30-day after discharging. All cases were seen
on that date as wounds surface (infections) or deep (hematomas, sores, and
fistulae) side-effects are recognized to happen after discharging.
Statistical analysis was performed via SPSS version20. Data had been examined for
normal distribution by means of the Shapiro Walk testing. Qualitative data have
been introduced as frequencies and relative percentages. χ2 test
was utilized to determine change among qualitative variables as specified.
Quantitative have been introduced as mean and SD. Student t testing has been
utilized to determine variance among quantitative variables in 2 groups.
Results considered significant at P-value < 0.05.
This study shows that a statistically significant change was found among the
study groups as (With drainage and Without drainage) regarding cardiovascular
dis, HTN, IHD, drain, open/Lap, covering stoma and mean mortality during
hospital stay.
A statistically nonsignificant change was found among the study groups as (With
drainage and Without drainage) regarding post op leak, localized, abscess,
generalised and mortality during hospital stay.
The current work showed that 3 out of 83 cases (2 with drains and one without the
drain) had a post anastomotic leak with significant difference in age,
cardiovascular comorbidities and no defunctioning stoma was done on the same set
with elective anterior resection [8,9].
Prophylactic drainage after elective Anterior resections with stapled colorectal
or colo-anal anastomosis decreases neither the rate of cases with one or more
post-operative complications maybe impacted by drainage nor the complications
severity.
This table (Table 1&2) shows that a statistically no significant change was
found among the study groups as (With drainage and Without drainage) and for
tumor site either Rectosigmoid or Rectal. No significant change was found
among the study groups as regard Neoadjuvant chemorad, Age, Gender, smoking, DM,
Steroids and ASA grade.
Table 1: Comparing among the study groups as regard
demographics.
|
|
With drainage
(n = 54)
|
Without drainage
(n = 29)
|
Test of Sig.
|
P
|
|
Rectosigmoid
|
4 (7.4%)
|
4 (13.8%)
|
χ2=0.883
|
FEp=0.441
|
|
Rectal
|
39 (72.2%)
|
19 (65.5%)
|
χ2=0.403
|
0.526
|
|
Neoadjuvant chemorad
|
3 (5.6%)
|
2 (6.9%)
|
χ2=0.060
|
FEp=1.000
|
|
Age
Mean ± SD.
Median (Min. – Max.)
|
66.30 ± 9.36
|
67.03 ± 12.53
|
t=0.304
|
0.762
|
|
66.30 ± 9.36
|
71.0 (28.0 - 84.0)
|
|
|
|
Gender
Male
Female
|
40 (74.1%)
|
17 (58.6%)
|
χ 2=2.094
|
0.148
|
|
14 (25.9%)
|
12 (41.4%)
|
|
Smoker
No
Smoker
EX
|
35 (64.8%)
|
26 (89.7%)
|
χ 2=6.058
|
MCp=0.04 4
|
|
4 (7.4%)
|
1 (3.4%)
|
|
15 (27.8%)
|
2 (6.9%)
|
|
DM
|
13 (24.1%)
|
5 (17.2%)
|
χ2=0.519
|
0.471
|
|
Steroids
|
2 (3.7%)
|
0 (0.0%)
|
0 (0.0%)
|
FEp=0.540
|
|
ASA
1
2
3
|
7 (13.0%)
|
5 (17.2%)
|
|
|
|
38 (70.4%)
|
18 (62.1%)
|
χ 2=0.601
|
0.741
|
|
9 (16.7%)
|
|
|
|
SD: Standard deviation, t: Student t-test, χ 2: Chi square
testing,
MC: Monte Carlo, FE: Fisher Exact,
*: Statistical significance at p
Table 2: Comparing among the study groups as regard different
parameters.
|
|
With drainage
(n = 54)
|
Without drainage
(n = 29)
|
Test of Sig.
|
P
|
|
Cardiovascular dis
|
2 (3.7%)
|
11 (37.9%)
|
χ 2=16.733*
|
FEp=<0.001
|
|
AF
|
0 (0.0%)
|
1 (3.4%)
|
χ 2=1.885
|
FEp=0.349
|
|
AO
|
0 (0.0%)
|
1 (3.4%)
|
χ 2=1.885
|
FEp=0.349
|
|
AVR
|
0 (0.0%)
|
1 (3.4%)
|
χ 2=1.885
|
FEp=0.349
|
|
Dil cardiomyopathy
|
0 (0.0%)
|
1 (3.4%)
|
χ 2=1.885
|
FEp=0.349
|
|
HF
|
0 (0.0%)
|
1 (3.4%)
|
χ 2=1.885
|
FEp=0.349
|
|
HTN
|
2 (3.7%)
|
6 (20.7%)
|
χ 2=6.250
|
FEp=0.019*
|
|
IHD
|
0 (0.0%)
|
3 (10.3%)
|
χ2=5.796*
|
FEp=0.040*
|
|
MVR
|
0 (0.0%)
|
1 (3.4%)
|
χ 2=1.885
|
FEp=0.349
|
|
Drain
|
54 (100.0%)
|
0 (0.0%)
|
χ 2=83.00
|
FEp =<0.001
|
|
Open/Lap
OPEN
|
37 (68.5%)
|
7 (24.1%)
|
χ 2=14.919
|
FEp<0.001
|
|
LAP
|
17 (31.5%)
|
22 (75.9%)
|
|
Covering stoma
|
42 (77.8%)
|
13 (44.8%)
|
χ 2= 9.164
|
FEp= 0.002
|
|
Post op leak
|
3 (5.6%)
|
1 (3.4%)
|
χ 2 =0.183
|
FEp =1.000
|
|
Localized
|
3 (5.6%)
|
0 (0.0%)
|
χ 2=1.672
|
FEp=0.548
|
|
Abscess
|
3 (5.6%)
|
0 (0.0%)
|
χ 2=1.672
|
FEp=0.548
|
|
Generalised
|
3 (5.6%)
|
0 (0.0%)
|
χ 2=1.672
|
FEp=0.548
|
|
Mortality during hospital
Stay
|
2 (3.7%)
|
0 (0.0%)
|
Χ2 =1.101
|
FEp=0.540
|
|
Mean ± SD.
|
10.25 ± 5.06
|
7.28 ± 2.90
|
|
|
|
Median (Min. – Max.)
|
9.0 (5.0 - 30.0)
|
6.0 (3.0 - 14.0)
|
Χ2 =418.50*
|
FEp=0.001
|
SD: Standard deviation; U: Mann Whitney test; χ 2: Chi square
testing;
FE: Fisher Exact
*: Statistical significance at p < 0.05
A statistically nonsignificant change was found among the study groups as
open/lap (With drainage and without drainage) post op leak, localized abscess,
generalized peritonitis and mortality during hospital stay.
Merad et al. [10] showed that the two studied groups were similar regarding pre-
operative data, excluding that there were significantly (P
value<0.02) more cases with ascites in cases who didn’t
experience drainages. In accordance with our findings, other parameters,
counting weight losing (P value<0.20), corticosteroids usage (P
value<.10), Crohn disorder (P value<0.30),
intra-operative fecal soiling (P<0.10), and leakages on testing for
airtightness (P value<0.50), were met more commonly in who
didn’t experience drainages, but these variances were nonsignificant
(Figure 1&2).
Figure 1: Comparing among the study groups (With drainage and
Without drainage) according to gender.
Comparing among the study groups as regard gender
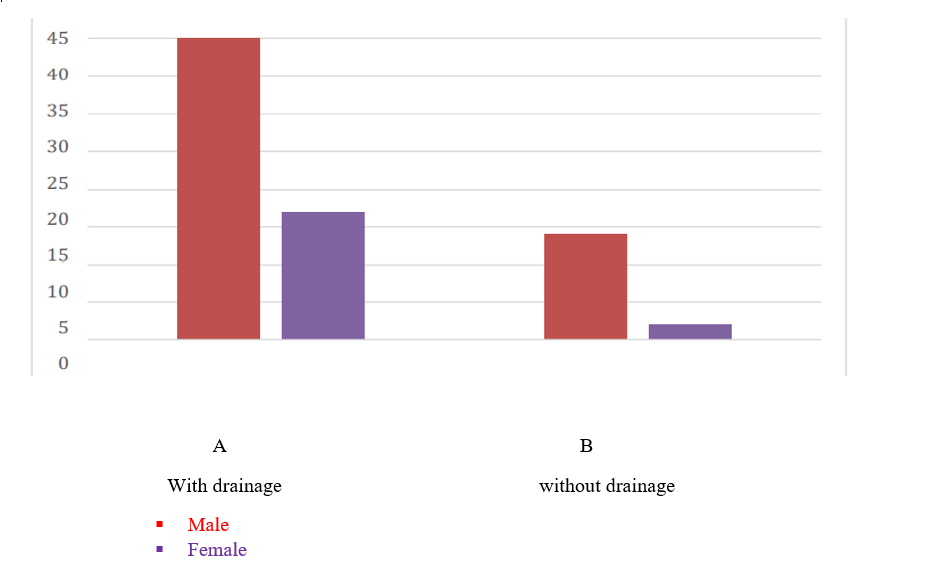
Figure 2: Comparing among the study groups (With drainage and
Without drainage) according to age.
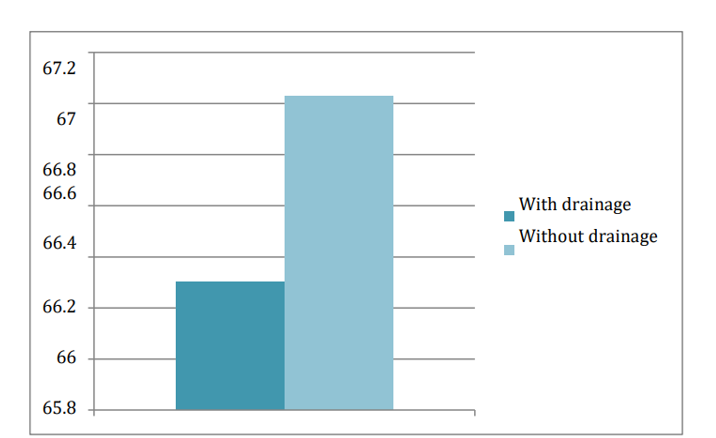
In agreement with our results, Hirahara et al. [2] found nonsignificant changes
in terms of the mean age of the cases, males/females’ ratio, BMI, and
concurrent disorders among the study groups.
In a systematic review by Podda et al. [11], several series stated a diversity of
risk- factors for AL post colo-rectal operation, counting age, pre-operative
nutritious condition, cardio-vascular and respirational co-morbidities,
incidence of opposing intra- operative effects, and the existence of a
de-functioning stoma. Tumor localizations in the lower and middle third of the
rectum, predominantly with an anastomotic height of<50 mm from the anal
border, have as well been measured clinical risk-factors for AL This study shows
that a statistically significant change was found among the study groups as
(With drainage and Without drainage) regarding cardiovascular dis, HTN, IHD,
drain, open/Lap, covering stoma and mean mortality during hospital stay. A
statistically nonsignificant change was found among the study groups as (With
drainage and Without drainage) and AF, AO, AVR, Dil cardiomyopathy, HF, MVR,
post op leak, localized, abscess, generalised and mortality during hospital
stay.
In disagreement with our results, Hirahara et al. [2] revealed that there
was insignificant difference between both groups as regard
cardiovascular diseases, Hypertension, Ischemic heart disease.
Post-operative outcomes are summarized in a study by Hirahara et al. [2]. Total
post- operative problems built on the Clavien-Dindo classifications were found
in 31% and 30% of cases in the drain and no drain groups, resp., and a
nonsignificant change was found in complication rates among the study groups.
There was no in-hospital death in this work, but single case in the no-drain
group who advanced Petersen’s hernia needed re-operation on
8thday post-operatively. As regard the post-operative
hospitalization, a nonsignificant change was detected among both groups. When
taking the existence and non-presence of post-operative problems into attention,
the hospitalization period didn’t vary among both groups.
In disagreement to preceding suggestion, the metanalysis by Rondelli et al., [12]
which enrolled randomized and nonrandomized reports, revealed that the existence
of a prophylactic drains decreased the occurrence of extra-peritoneal colorectal
AL and the rate of re-operations thereafter anterior rectal resection. But the
protecting value of PD was maintained by the data from nonrandomized reports
only, as the sub-group investigation of RCTs didn’t display any advantage
for PD usage.
Moreover, the big Dutch study by Peeters et al., [13] revealed that, on multi-
regression analysis, the non-presence of a pelvic drainages and a de-functioning
stoma were the issues accompanying with anastomotic dehiscence. More definitely,
the existence of one or more pelvic drains postoperatively was significantly
accompanied with a lower AL: 9.59% of cases with pelvic drainages had leakages,
in comparison with 23.50% of cases with no drain, and 8.20% of cases with a
de-functioning colostomy or ileostomy had a leakage, in comparison to 16% with
not a stoma. Consequently, the authors reported that, in a try to minimalize the
risks of clinical AL, the constructions of a de-functioning stoma and the
assignment of one or more drainages in the presacral cavity looks desirable for
cases with proximal as well as distal rectal tumors.
Merad et al. [10] showed that the post-operative death in their study was 4.4%,
which was within the rates of post-operative mortality reported in the other
studies:
3- 6% in a trial by Hoffmann et al. [14] and in a study by Sagar et al. [15]
Merad et al. [10] showed that 0.30% rate of mortality because of anastomotic
leakages was less than the rates of 0.85- 2.00% stated somewhere else in a study
by Hagmüller et al. [16] and a study by Sagar et al., [15]. In contrast,
there were no mortalities secondary to anastomotic leakages in 2 of the other
trials by Johnson et al. [17] and Sagar et al. [15].
Routine pelvic drainage after elective anterior resection does not reduce the
rate or severity of anastomotic leak. It may, infrequently, be harmful.
The Authors declares no potential conflicts of interest with respect to the
research, authorship, and / or publication of this article.
Ethical Approval and Consent to participate: Consent to
participate was gained by the patient.
Consent for publication: N/A
Availability of data and materials: All data and materials are
available if further steps required.
Competing interests: Not Applicable
Funding: There is no funding source -Authors' contributions:
Mr. Mena: collect the data, writing the article and do analysis; Mr. Bisheet:
review and revise the paper
- Abu-Omar Y, Kocher GJ, Bosco P, Barbero C, Waller D, et al. (2017) European
Association for Cardio-Thoracic Surgery expert consensus statement on the
prevention and management of mediastinitis. Eur J Cardiothorac Surg
51: 10-29. [Crossref]
- Hirahara N, Matsubara T, Hayashi H, Takai K, Fujii Y, et al. (2015)
Significance of prophylactic intra-abdominal drain placement after
laparoscopic distal gastrectomy for gastric cancer. World J Surg
Oncol 13: 181. [Crossref]
- Cerda-Cortaza JL, Prieto Aldape R, González Muñoz AH,
Campos-Campos SF, Fuentes Orozco C, et al. (2019) Results of a National
Survey on the preparation, management and monitoring of colonic anastomosis.
Cirujano General 41:168-176.
- Anderson TA, Anderson R, Nargozian C (2018) Specific Newborn and Infant
Procedures. Essentials of Anesthesia for Infants and Neonates, 199.
- Birolini C, de Miranda JS, Tanaka EY, Utiyama EM, Rasslan S, et al. (2020)
The use of synthetic mesh in contaminated and infected abdominal wall
repairs: challenging the dogma—a long-term prospective clinical
trial. Hernia 24: 307-323. [Crossref]
- Nussbaum MS, McFadden DW (2019) Gastric, duodenal, and small intestinal
fistulas. In Shackelford's Surgery of the Alimentary Tract, 2: 886-907.
- Watanabe Y, Koshiyama M, Seki K, Nakagawa M, Ikuta E, et al. (2019)
Development and themes of diagnostic and treatment procedures for secondary
leg lymphedema in patients with gynecologic cancers. In Healthcare,
Multidisciplinary Digital Publishing Institute, 7: 101.
- Saikaly E, Saad MK (2020) Anastomotic Leak in Colorectal Surgery: A
Comprehensive Review. Epidemiology 5: 6.
- Moro ML, Carrieri MP, Tozzi AE, Lana S, Greco D (1996) Risk factors for
surgical wound infection in clean surgery: a multicenter study.Ann Ital
Chir 67: 13–9. [Crossref]
- Merad F, Yahchouchi E, Hay J, Fingerhut A, Laborde Y, et al. (1998)
Prophylactic abdominal drainage after elective colonic resection and
suprapromontory anastomosis: A Multicenter Study Controlled by
Randomization. Arch Surg 133: 309–314. [Crossref]
- Podda M, Di Saverio S, Davies RJ, Atzeni J, Balestra F, et al. (2019)
Prophylactic intra-abdominal drainage following colorectal anastomoses. A
systematic review and meta-analysis of randomized controlled trials. Am
J Surg 219: 164-174. [Crossref]
- Rondelli F, Bugiantella W, Vedovati MC, Balzarotti R, Avenia N, et al.
(2014) To drain or not to drain extraperitoneal colorectal anastomosis? A
systematic review and meta-analysis. Colorectal Dis 16:
O35-eO42. [Crossref]
- Peeters KC, Tollenaar RA, Marijnen CAM, Kranenbarg KE, Steup WH, et al.
(2005). Risk factors for anastomotic failure after total mesorectal excision
of rectal cancer. Br J Surg 92: 211-216. [Crossref]
- Hoffmann J, Shokouh-Amiri MH, Damm P, Jensen R (1987) A prospective
controlled study of prophylactic drainage after colonic anastomoses. Dis
Colon Rectum 30: 449- 452. [Crossref]
- Sagar PM, Couse N, Kerin M, May J, MacFie J (1993) Randomized trial of
drainage of colorectal anastomosis. Br J Surg 80: 769- 771. [Crossref]
- Hagmüller E, Lorenz D, Werthmann K, Trede M (1989) Prophylactic
drainage in elective colic resections? Program and abstracts of the
33rd World Congress of Surgery September 10-16.
- Johnson CD, Lamont PM, Orr N, Lennox M (1989) Is a drain necessary after
colonic anastomosis? J R Soc Med 82: 661- 664. [Crossref]
