Introduction
Hereditary hemorrhagic telangiectasia – HHT (Osler-Weber-Rendu syndrome) is a heterogeneous autosomal dominant genetic disease, in which cutaneous-mucosal telangiectasia and arterio-venous malformations occur in various organs. From its first description in 1865 (Figure 1), it is frequently mentioned in Textbooks of Hematology, Dermatology or Gastroenterology and is known for its numerous eponymous attributes throughout the time. In medical practice, the disease is rarely encountered, with an incidence of 1-2/100000. Our paper presents a case with multilevel gastrointestinal lesions that we endoscopically highlighted both in white light and in FICE virtual chromoendoscopy.
Figure 1. From the first cases described in the literature to our case (male, 63 years old)
Case
A 62-year-old man presented for evaluation of serious iron deficiency anemia, in whose family six other members of four consecutive generations had the same manifestations (Figure 2). In addition, the patient has numerous telangiectasia in the skin and mucous (Figures 3-5), including several level of the digestive tract (oral cavity-Figure 6, esophagus-Figure 7, gastric body-Figure 8, pyloric antrum-Figure 9, duodenal bulb-Figure 10, postbulbar duodenum-Figure 11, sigmoid colon-Figure 12 and rectum-Figure 13). The patient has no manifestations of arterio-venous abnormalities in the nervous system, the lungs and the liver, and the CT scan of these organs did not identify vascular malformations (Table 1).
Table 1. Diagnostic criteria present at the patient
Criteria | Organs | +/- | Location | Bleeding | Investigations |
Epistaxis | | þ | | +++ (spontaneous, recurrent) | Nasal endoscopy revealed septo-torsional synechiae and telangiectasia |
Telangiectasia | | þ | Lips | + | |
Oral cavity | + | |
Face (periorbitar, nose) | | |
Auricular pavilion | | |
Visceral lesions | Gastro-intestinal | þ | Pharynx Esophagus Stomach Duodenum Rectum | ++ | Superior digestive endoscopy revealed multiple telangiectasia in the esophagus, gastric body, pyloric antrum and bulbar duodenum and post-bulbar duodenum. Lower digestive endoscopy revealed telangiectasia only in the rectum. |
Broncho-pulmonary | ý | | | Without pulmonary aneurysmal dilatation or arterio-venous malformations (CT) |
Brain injuries | ý | | | Without cerebral aneurysmal dilatation or arterio-venous malformations (CT) |
Spinal | ? | | | Uninvestigated |
Liver damage | ?/ý | | | Unidentified (Echo) |
Arterio-venous malformations | ?/ý | | | Unidentified at the brain, lung and liver |
Family history | | þ | Great-grandfather GG Grandmother-GM Father-F Uncle-U Uncle-U Daughter-D | | Analysis of mutations - the results obtained were aligned with the human genome hg38; the genes tested were: ACVRL1, ENG, GDF2, SMAD4, PTEN, PTPN11, PIK3CA, RASA1, TEK and AKT1; the sample presents Class 3 mutations, which do not still have clinical significance. |
Figure 2. The genetic investigation revealed in the patient's family 7 cases with autosomal dominant transmission over five generations
Circle=male, Rectangle=female, GG=Great-grandfather, GM=Grandmother, F=Father, U=Uncle, P=Patient, D=Daughter
Figure 3. Telangiectasis on the face

Figure 4. Telangiectasis on the lips and tongue
Figure 5. Telangiectasis on the larynx (a-examination in white light; b-examination in FICE spectrum)

Figure 6. Telangiectasis on the soft palate
Figure 7. Telangiectasia on the esophagus (a-examination in white light; b-examination in FICE spectrum)

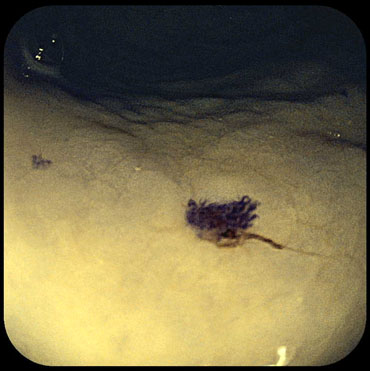
Figure 8. Telangiectasia on the gastric body (a-examination in white light; b-examination in FICE spectrum)
Figure 9. Telangiectasia on the pyloric antrum (a-examination in white light; b-examination in FICE spectrum)
Figure 10. Telangiectasia on the bulbar duodenum (a-examination in white light; b-examination in FICE spectrum)
Figure 11. Telangiectasia on the post-bulbar duodenum (a-examination in white light; b- examination in FICE spectrum)
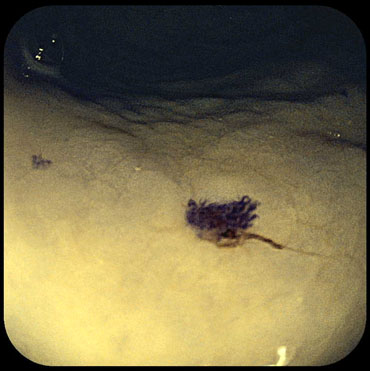
Figure 12. Telangiectasia on the sigmoid colon (a-examination in white light; b-examination in FICE spectrum)
Figure 13. Telangiectasia on the rectum (a-examination in white light; b-examination in FICE spectrum)
Considering that the patient meets all four international diagnostic criteria (Table 1), we appreciated that the patient suffered from HHT (Rendu-Osler-Weber disease).
With repeated and severe episodes of epistaxis and digestive hemorrhage, the patient has received blood transfusions several times or parenterally treatment with iron products.
Discussion
The case is interesting because it refers to a very low incidence in the world. Osler-Weber-Rendu disease is a rare genetic condition causing systemic fibrovascular dysplasia, epistaxis and digestive bleeding. Phenotypic variation is extreme ranging from asymptomatic to severely symptomatic, from cases with no or few mucocutaneous lesions to those with diffuse cutaneous telangiectasia. We discuss a case of Osler-Weber-Rendu disease causing diffuse cutaneous telangiectasia, epistaxis, digestive bleeding and iron deficiency anemia.
In addition, there are extensive vascular lesions of the digestive tract that we have been able to observe and record in detail, both in white light and in virtual FICE chromoendoscopy.
The FICE spectrum examination allows for better endoscopic evidence of erythrocytes, mucous and submucosa vessels, due to good penetration and different reflections of green light and blue light. Vascular lesions from various organs occur when the angiogenesis process is disturbed due to multiple genes, depending on which disease is classified into four types: HHT-1 (mutations of ENDOGLIN / ENG), HHT-2 (mutations of ALK-1), HHT-3 (mutations of RASA-1) and HHT-4 (mutations of SMAD-4).
Following the genetic profile of the patient, we determined that it suffers from type 2 disease (with ALK1 gene affection), a clinical form in which there are more frequent hepatic and less pulmonary vascular malformations.