Background: The most common condition treated by paediatric neurosurgeons is hydrocephalus. Despite having significant improvements in treatment and management, hydrocephalus continues to have a considerable impact on the long-term outcome in children. The objective of designing Electronic Integrated Text, Visual and Audio Questionnaire (EITVAQ) was to develop a child-friendly tool, anticipating it will be a better tool to measure child health status from a child’s perspective.
Methods: This was a prospective crossover pilot study that compared the outcome and completion rate between EITVAQ and a printed text 2-paged paper questionnaire (TEXT). Children with hydrocephalus from 8 years old to 16 years old were invited to participate in this study from November 2015 to June 2016. EITVAQ was created to be visual and audio automated using macros-enabled function in Microsoft PowerPoint. Time of completion for each format was recorded. All data were compiled and organized for statistical analysis using Software Package using Statistical Analysis (SPSS).
Findings: 24 children participated in this study. There was a 100% completion rate for EITVAQ with only 37.5% completing the TEXT format. The mean time to complete EITVAQ was 7 minutes and the mean time for TEXT was 15 minutes. The mean score for EITVAQ was 16% higher in comparison to a mean score of HOQ completed by proxy. The result suggested participants with more surgical procedures tend to have a higher incompletion rate of TEXT format by 18.9%. However, there was no correlation found between physical disabilities and the incompletion rate. Such results suggested that the incompletion rate in TEXT format is likely secondary to a central cause rather than a physical cause.
Conclusions: In this study, the results supported that EITVAQ is a better tool to evaluate the health status of paediatric hydrocephalus patients. Such encouraging results call for future research in this area to develop EITVAQ as a validated tool and to be used widespread across hydrocephalus patients to identify health status issues, to enable them to access appropriate early intervention and to improve their quality of life.
Abbreviations
ACHI: Australian Classification of Health Interventions; ACS: Australian Coding Standards; AVM: Arteriovenous malformation; BRIEF: Behavioral Rating Inventory of Executive Function; CHQ-CF-87: Child Health Questionnaire; CSF: Cerebrospinal fluid; CUH: Children University Hospital; EITVAQ: Electronic Integrated Text, Visual and Audio Questionnaire; ETV: Endoscopic third ventriculostomy; GMFCS: Gross motor function classification system; HOQ: Hydrocephalus Outcome Questionnaire; HRQOL: Health-related quality of life; HUI: Health Utilities Index; ICD-10-AM: International Statistical Classification of Diseases and Related Health Problems, Tenth Revision, Australian Modification; IQ: Intelligent Quotient; PEDSQL: Pediatric Quality of Life; SF36: 36-Item Short-Form Health Survey; SPSS: Software Package using Statistical Analysis; TACQOL-CF: TNO- AZL Netherlands Organization for Applied Scientific Research Academic Medical Centre Children’s Quality of Life; TEXT: Printed text 2-paged paper questionnaire; TORCH: Toxoplasmosis, Rubella, Cytomegalovirus, Herpes Simplex; VPS: Ventriculoperitoneal shunt
Definition
Hydrocephalus is an inappropriate accumulation of cerebrospinal fluid (CSF) within the brain ventricles. This occurs when there is an imbalance between the rate of production of CSF and the rate at which it is absorbed [1]. This results in cerebral ventricles enlargement, presenting with increased intracranial pressure signs and symptoms.
Incidence
Kahle KT stated that the most common condition treated by paediatric neurosurgeons is hydrocephalus [1]. The prevalence of infant hydrocephalus in a developed country is estimated to be one case per 1000 births [2], but this is undoubtedly higher in developing countries [3]. For example in sub-Saharan Africa, the new cases of infant hydrocephalus might exceed 200 000 per year [4].
Causes
Hydrocephalus has many causes as shown in Table 1 [2]. It can be acquired or congenital. Congenital causes include congenital aqueduct stenosis, neural tube defects, Arnold-Chiari malformation, developmental cysts and congenital foramen of Monroe atresia. Acquired causes are generally from pathological processes that disturb the ventricular outflow, subarachnoid space function, or cerebral venous compliance. These includes intracranial haemorrhage, infections, brain tumours and vascular malformation [2]. The common causes of hydrocephalus in developed countries are post-haemorrhagic hydrocephalus of prematurity, congenital aqueduct stenosis, myelomeningocele, and brain tumours [5,6].
Table 1. Causes of hydrocephalus
Causes of hydrocephalus |
|
Congenital |
Congenital aqueduct stenosis |
|
Neural tube defect |
|
Posterior fossa malformations |
|
Developmental cysts |
|
Congenital foramen of Monro atresia |
Acquired
|
Infections- Bacteria/ viral meningitis |
|
Haemorrhage-Intracranial Haemorrhage |
|
Neoplasm- parenchymal brain tumour, spinal cord tumour, choroid plexus tumour |
|
Vascular- Vascular malformation- arteriorvenous malformation |
Clinical presentations
Usually for hydrocephalus, clinical presentations vary with age.
It can be detected during antenatal anomaly scans between 18-20weeks gestations [7]. Detection of ventriculomegaly often prompts further investigations, including TORCH screening (toxoplasmosis, rubella, cytomegalovirus, herpes simplex), fetal Magnetic Resonance Imaging (MRI) and/or amniocentesis [8].
In infants, hydrocephalus commonly presents with an abnormal increased head circumference, irritability, vomiting, seizure, bulging of the anterior fontanelle and/or widening of the cranial sutures [1].
Beyond infancy, hydrocephalus typically presents with an array of findings that include a combination of headache, vomiting, delayed developmental milestones, diplopia (usually from a VI cranial nerve palsy), seizure and/or papilloedema [1].
Treatment
Current treatment options are mainly surgically approached. 60 years-post introduction of 'shunt', CSF shunting remains the standard approach [9]. It primarily involves an insertion of a Silastic tube using a valve mechanism to divert accumulating CSF [9]. The most common type of shunt is ventriculoperitoneal shunt (VPS), enabling draining of CSF from the ventricles to the peritoneal cavity. Other types of shunt involve other sites such as the right atrium of the heart and the pleural cavity [9].
In the 1990s, endoscopic third ventriculostomy (ETV) emerged as an alternative treatment for hydrocephalus, particularly in patients with non-communicating hydrocephalus. ETV is known as intracranial “CSF diversion” by allowing CSF to be diverted elsewhere to bypass an obstruction without inserting a shunt. Currently, this procedure is routinely carried out at most major paediatric neurosurgical centres in the developed world. ETV involves passing an endoscope into the frontal horn of the lateral ventricle, then through the foramen of Monro and into the third ventricle, allowing CSF to flow out of the blocked ventricular system into the interpenducular cistern (a normal CSF space) and thereby relieving pressure [10].
Outcome
With the current standard of care, the majority of children with hydrocephalus survive to adulthood. The long-term outcome of hydrocephalus in the paediatric population varies from individual to individual. There are many studies available exploring the surgical outcomes of hydrocephalus [11]. However, neurodevelopmental and neuropsychological studies on the outcome of children with hydrocephalus are limited because the sample selections are small and often restricted by the patients’ disabilities [12-15].
The degree of long-term cognitive dysfunction is dependent on the causal mechanisms of hydrocephalus and any underlying brain dysmorphology or primary injury from an inciting event such as infection or haemorrhage [16]. For example, it is noted that children with isolated aqueductal stenosis with no other brain anomaly have a cognitive level of normal healthy developing children [16]. In many children, cognitive dysfunction can be subtle and difficult to pick up. This includes impairment in overall intelligence, verbal intelligent quotient (IQ), spatial navigation, executive functioning, learning, memory and/or processing information [1,16-20].
A review by Kulkarni in 2010 stated that only 20% of children with hydrocephalus would lead a near-normal quality of life [21]. Otherwise, majority of children with hydrocephalus often suffered from various symptoms and signs affecting their quality of life. As many as 34% of patients treated in infancy for hydrocephalus were at risk of developing epilepsy in their later life [22]. Up to 20% of children with shunt often suffered from severe headaches [21]. Over 40% of children with shunted hydrocephalus often suffer from chronic headache [23]. Furthermore, 45% of individuals who were treated in infancy for hydrocephalus and had previous shunt insertion are were often depressed with 43% of them dependent on care and 43% of them remained unemployed when they enter adulthood [24-26]. This reflects that hydrocephalus made a huge impact on the quality of life. Moreover, with figures above suggests that this cohort of patients are a huge burden to the family, carer and the society.
The Hydrocephalus Outcome Questionnaire (HOQ) by Kulkarni was developed to measure the health status in children with hydrocephalus [25]. The questionnaire consisted of 51 questions taking parents 10-15 minutes to complete. Parents were thought to be the best candidate to assess their child health status [25]. However, HOQ underestimates cognitive and social competence from the patient’s perspective. Parents’ responses may be the closest answer, but their assessments are often biased. Furthermore, they cannot replace the voice of the patient.
Hansen D et al. stated that the emphasis on health-related quality of life (HRQOL) outcomes is increasing, along with a focus on evidence-based medicine [26]. However, there is a notable paucity of validated and standardized HRQOL instruments for the paediatric neurosurgical population [26-28].
Hence, gaps in information regarding the patient perspective of life and health status still exist. These aspects are difficult to measure and quantify as most hydrocephalus patients have an underlying disability (speech, hearing, cognitive and visual impairment) [27].
Background
In spite of significant advances in management, hydrocephalus in children continues to have a considerable impact on the long-term outcome [28]. Hydrocephalus mostly revolves around a complex medical condition for which multidisciplinary care is needed over an extended period of time. Children with hydrocephalus often require medical and surgical follow-up. Currently, studies are investigating the surgical outcomes of hydrocephalus mainly focusing on patient demographic, postoperative data and complication rates [11,27]. However, there are very limited amount reports on the functional outcomes and quality of life studies are still lacking [12-15,28].
The degree of long-term cognitive dysfunction varies from individual to individual. It is thought that the severity of it is dependent on the causal mechanisms of hydrocephalus and any accompanying brain dysmorphology [16].
For example, a study published by Holwerda JC et al. in May 2016 highlighted the importance of following up in patients who had hydrocephalus secondary to ventricular bleed [29]. Currently, there are studies that focus on the developmental and neuropsychological outcomes in preschool age. However, the results are thought to be unreliable [29-32]. There are also studies that concentrate on the outcome at school age; however they focus mainly on IQ [29]. Most studies showed patients that had hydrocephalus secondary to ventricular bleed during the neonatal period had a poorer performance IQ rather than verbal IQ [33-35]. Furthermore, it is noted that children that required surgical intervention is associated with lower IQ [29]. Holwerda JC et al. stressed the importance of focusing on the long term functional outcomes, which includes visual motor integration, executive function, motor skills and behavioural outcome among this cohort of patients. Results of the study showed that functional deficits were more prominent in children that had post-haemorrhagic ventricular dilatation in comparison with a normal population [29].
A paper published in 2012 by Lacy M et al., mentioned that children with hydrocephalus had executive function dysfunction when compared with healthy peers. Furthermore, parents of children with hydrocephalus noted that executive function deficit among their child were more obvious as age increases [18]. Another study published by Persson EK et al. in 2006 also noted that 47% of children with infantile hydrocephalus had various learning disabilities [22].
In 2005, a study in Sweden involving 73 participants with hydrocephalus described that one-third of patients had normal intelligence, 30% had lower average IQ, and 37% of the patients had learning disabilities. Interestingly, patients with normal intelligence still required special attention due to impaired perceptual and non-verbal abilities [36].
Hence, this highlights that children with hydrocephalus not only have a higher incidence of physical disabilities but also they might have subtle learning disabilities despite having a ‘normal’ intelligence. These results also pointed out that IQ is not an accurate marker in determining the neurodevelopment progress of a child with hydrocephalus. Furthermore, hydrocephalus have an enormous impact on a child’s learning pathway, which could cause a huge impact on their quality of life, especially entering adulthood.
There are different facets of health. The World Health Organization defines health as ‘‘a state of complete physical, mental and social well- being and not merely the absence of disease or infirmity’’ [37]. In today's health care environment it is important to aim to deliver a patient-centered health care to ensure adequate medical, social and education support given to children with hydrocephalus to ensure a smooth transition to adulthood.
It will be interesting to look at the quality of life for children with hydrocephalus. Currently, there are limited reports on health- related quality of life (HRQOL) outcomes using validated tools. HRQOL studies on hydrocephalus patient outcome are limited because the sample selections are small and restricted by the patients’ disabilities [12-15,26,28].
Hansen D et al. recently published a review reporting on the HRQOL questionnaire used over the last ten years [26]. There were 31 articles published using 46 different HRQOL questionnaires. HRQOL questionnaires that are commonly used in current literature include Pediatric Quality of Life (PedsQL), Health Utilities Index (HUI), the 36-Item Short-Form Health Survey (SF-36) and Hydrocephalus Outcome Questionnaire (HOQ). The HOQ and the SF-36 are the top 2 HRQOL questionnaire used in paediatric neurosurgical research. However, there are also various custom-designed, unnamed, or invalidated HRQOL questionnaire used, which indicate a lack of standardisation in the use of HRQOL instruments [26].
HRQOL Questionnaires can be classified as disease-specific or generic.
Generic instruments are designed to measure different facets of health that suits all populations. Therefore, they are appropriate for use across various paediatric populations including healthy populations and children with a medical and/or surgical illness covering a broader spectrum. On the other hand, disease-specific questionnaire measures specifically for patients with a particular condition or disease with questions tailored according to their condition or disease [38].
PedsQL
This questionnaire is made up of a primary set of 23 generic questions, with additional disease-specific questions. The main set of questions covers various aspects of health. PedsQL is appropriate for a child to self-report from ages 5–18 years and for parents to report by proxy. This questionnaire only takes less than 5 minutes to complete and it has a high reported reliability (> 0.88). Although PedsQL has a high reliability, this questionnaire is not child-friendly and it not suitable for patients with visual, hearing and speech impairment [39,40].
HOQ
HOQ was developed to measure objective health status in paediatric patients with hydrocephalus. It also has a high reported reliability (> 0.88). The questionnaire consists of 51 questions covering various facets of health looking at physical, social, emotional and cognitive aspects. The administration time required to complete the questionnaire by proxy is between 10-15 minutes [25,26].
HUI
This questionnaire is multidimensional, providing a score for each aspect of health (for example hearing, vision and linguistic competency) and an HRQOL score for overall health. Overall, HRQOL scores are on the conventional spectrum: dead (0.00) to perfect health (1.00). Multiple language translations are available. HUI is suitable for children aged five years or older. However, HUI accesses the vision, hearing and verbal competence which excludes children with hydrocephalus and disability from completing the questionnaire [41,42].
SF-36
This instrument was first released in 1990. It is a generic short-form survey with 36 questions, with an 8-scale profile of functional health and well-being. The questions assess multiple aspect of health, including function, distress, well-being and self-evaluations of health. Despite being used in numerous studies and countries, it is thought that this questionnaire is not suitable to be used by the paediatric cohort by the publishers of SF-36 [40].
Apart from the list above, currently, there are other quality of life questionnaires available from the child’s perspective such as the TNO- AZL Netherlands Organization for Applied Scientific Research Academic Medical Centre Children’s Quality of Life (TACQOL- CF) [43] and Child Health Questionnaire (CHQ-CF 87) [44]. Both are examples of general child health questionnaires, but they are not disease-specific. CHQ- CF 87 is a detailed test involving physical, mental and social-family measurements [44]. This questionnaire is lengthy and measures superfluous social family background that would not be suitable for a disease-specific patient like hydrocephalus patients. TACQOL-CF is a 15 minutes questionnaire that is designed for population age 6- 18 years. The test measures the following domains of health: body, motor, autonomy, cognitive and social-emotional [43]. However, children with hydrocephalus might find TACQOL-CF less child friendly and less interactive.
The main aim of health status questionnaire is to measure the quality of life from the patients’ perspective. However, this can be challenging in the paediatric cohort. In the case of normal children and adolescents, the children themselves can usually complete this. However, for majority patients with disability such as hydrocephalus, this might be a challenging task. Current studies tend to rely more on using proxy responders such as parents [45,46].
Parents’ and carer responses may be the nearest answer, but their assessments can be biased. For example, in children with spina bifida and hydrocephalus, patients’ appearances usually cause parents, carers and even teachers to underestimate their cognitive and social competence. This shows that parents or carers cannot replace the voice of a child. Besides, there have been significant concerns about the accuracy and acceptability of parent-proxy ratings of paediatric patients' HRQOL tool [26,47,48].
The utility of a generic HRQOL tool for children or adolescents has not been explicitly tested in patients with neurodevelopmental disorders [25,26,39,49-53]. There are very few paediatric neurosurgical clinical studies that use the HRQOL tools mentioned above to look into the clinical outcome of the patients [12-15,21,25,54]. These results were frequently found to be disappointing.
From the review by Hansen D et al., it is crucial to gather information about the HRQOL from patients’ experience and concerns, especially in surgical-related conditions to shape the future of health care delivery [26]. Secondly, it is important for us to prioritise autonomy of the patient, allowing appropriate and desirable patients' preferences and wishes to be taken into account in decision-making concerning their health care [26,46].
This stressed that gaps in information regarding the quality of life from patients’ perspective still exist. It is difficult to measure and quantify the quality of life from a child’s perspective, especially when children with hydrocephalus have an underlying disability (speech, hearing, cognitive and visual impairment) [27,55]. However, these gaps of information are crucial for health professionals in monitoring care and follow up especially when involving a multidisciplinary team.
The available studies concerning the quality of life of hydrocephalus patients are currently of low quality and lack standardisation. This could be secondary to the lack of a child-friendly validated questionnaire that accommodates their visual hearing and speech impairment [26].
At present, there are various learning style methods exist [56]. A study done by specific diagnostic studies concluded that 29% of elementary and high school students learn best through the visual aids, 34% through the auditory aids, and 37% through the tactile /kinesthetic aid [56]. It has shown that a child’s achievement and motivation improve when learning and teaching styles are matched [56]. This proposes that by using and applying visual, auditory and kinesthetic modes, children with hydrocephalus would be able to perform better in comparison to a printed text questionnaire.
Hence it is important for us to stop drawing attention to what children with hydrocephalus are unable to do and start focusing on how to create a better quality of life questionnaire that is tailored according to their needs and capabilities to ensure a more accurate collection of data among hydrocephalus patients.
Hence, this serves as a call for research to incorporate and fill in the gaps of information in designing a suitable questionnaires, leading to this research title: Will electronic integrated text, visual and audio questionnaire be a better tool to evaluate the health status of paediatric hydrocephalus patients?
Primary aims
- To design EITVAQ as an interactive, quick and easy tool to measure the health status of children with hydrocephalus.
- To design EITVAQ as a questionnaire in facilitating the needs of children with hydrocephalus, enabling them to complete the questionnaire
- To identify that EITVAQ is a better tool to measure health status when compared to a TEXT format
- To identify that EITVAQ has the potential to measure the health status of children with hydrocephalus from the patient perspective
Secondary aims
- To gain widespread usage of EITVAQ and collaborate with other research in forming a reliable and validated tool
- To gain widespread usage of EITVAQ by medical practitioners, physicians and neurosurgeons to evaluate and access health status of children with hydrocephalus
- To gain widespread usage of EITVAQ to provide baseline background information for multidisciplinary teams to allow smooth transition and integration to adult health services and community in the future
- To gain widespread usage of EITVAQ to shape a better delivery of care to children with hydrocephalus
Study design
This was a prospective crossover pilot study that was carried out in Temple Street, Children University Hospital (CUH), Ireland. CUH is a tertiary referral neurosurgical centre for all neurosurgical condition ranging from 0 months-16 years old. It accepts all children under 16 years old all over Ireland.
This study was held in the neurosurgical outpatient department, which was held every Thursday morning. The outpatient list consisted of patients with various neurosurgical conditions, such as hydrocephalus, spina bifida, brain tumours, arteriovenous malformation (AVM) and chronic headache. On average there were about 20 patients per clinic list, which was held every Thursday morning. In each clinic, there were around three hydrocephalus patients and one new referral. This study was conducted from November 2015 to June 2016. During the study period, it was targeted to gain at least 20 participants with hydrocephalus, whose parents were willing to sign consent and participate in this study at the neurosurgical outpatient department.
All participants needed to be well and stable when completing EITVAQ and TEXT so that they can concentrate and complete the questionnaire accurately. It was also important for them to be clinically stable to hear a true voice from their perspective on how hydrocephalus as made an impact in their life.
All patients in Temple Street, CUH are coded electronically according to the Irish Coding Systems: International Statistical Classification of Diseases and Related Health Problems, Tenth Revision, Australian Modification (ICD-10-AM), Australian Classification of Health Interventions (ACHI) and Australian Coding Standards (ACS), also known as the ICD-10-AM/ACHI/ACS 8th edition.
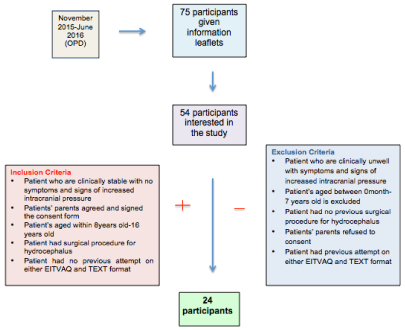
Upon checking in at the reception desk, all patients coded for hydrocephalus with shunt were given information leaflet about the study and were invited to participate in this study, as shown in Appendix 1,2 and 3. If they agreed to participate, clinical details of each participant were checked with inclusion and exclusion criteria applied. Finally, participants that qualified for the study would be recruited and were brought to a room to participate the study.
Patients were selected as per the following criteria:-
Inclusion Criteria:
- Patient who are clinically stable with no symptoms and signs of increased intracranial pressure
- Patients’ parents agreed and signed the consent form
- Patient’s aged within 8years old-16 years old
- Patient had surgical procedure for hydrocephalus
- Patient had no previous attempt on either EITVAQ and TEXT format
Exclusion Criteria:
- Patient who are clinically unwell with symptoms and signs of increased intracranial pressure
- Patients aged between 0month-7 years old is excluded
- Patient had no previous surgical procedure for hydrocephalus
- Patients’ parents refused to consent
- Patient had previous attempt on either EITVAQ and TEXT format
EITVAQ
EITVAQ was a survey covering four main domains of health and a satisfaction rating of the questionnaire:
1. Physical
2. Mental
3. Social
4. Cognitive
5. Patient Satisfaction Rating of the EITVAQ
These questions were set based on a literature review on previous hydrocephalus research outcome, previously validated health status questionnaire and previous child-centered health questionnaire available. The list of questions was compiled and reviewed by a multidisciplinary team including Neurosurgeons, Paediatrician, Staff Nurses, School Teacher, Neuropsychologist, Occupational Therapist and Social Worker.
The final questionnaire was presented to participants in both word document (TEXT) and PowerPoint file (EITVAQ).
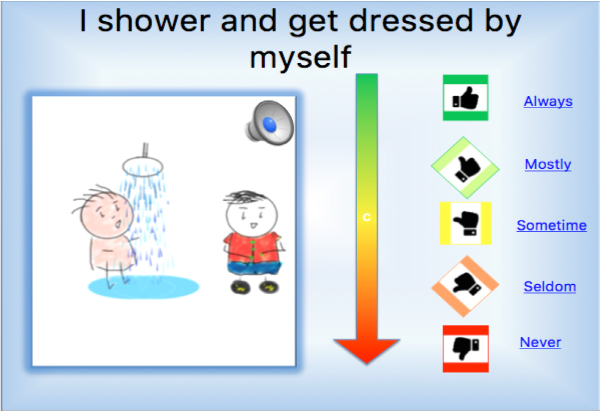
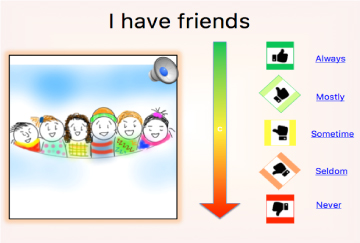
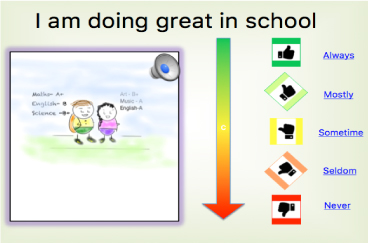
EITVAQ was created with one question per slide. In each slide, there would be a question projected with integrated audio, picture and text formats to accommodate patients with visual, speech or hearing disabilities. Each question stem would begin with the phrase “I …” or “We…”. For example, “I go to school” and “We visit each other. These questions were to be answered on 5-point scale ranging from 1 to 5 with a text, motion picture and audio format; 1 being ‘never’ to 5 being ‘always’. Each function was coded using the macros-enable function on PowerPoint. On each slide, the audio function could be presented, simply by scrolling the mouse pad onto the speaker icon available. Each question’s answer must be selected in order to progress on to the next question. The coding messages to set up EITVAQ all automated function are shown in Table 2. Samples of EITVAQ in PowerPoint slides and TEXT format are shown below in Figure 1-4 and Table 3.
Table 2. Coding messages on Microsoft PowerPoint Macros enabled
Dim number Always As Integer
Dim number Mostly As Integer
Dim number Sometimes As Integer
Dim number Seldom As Integer
Dim number Never As Integer
Sub Always Answer ()
Number Always = number Always + 1
ActivePresentation.SlideShowWindow.View.Next
End Sub
Sub Mostly Answer ()
numberMostly = numberMostly + 1
ActivePresentation.SlideShowWindow.View.Next
End Sub
Sub Sometimes Answer ()
numberSometimes = numberSometimes + 1
ActivePresentation.SlideShowWindow.View.Next
End Sub
Sub Seldom Answer ()
numberSeldom = numberSeldom + 1
ActivePresentation.SlideShowWindow.View.Next
End Sub
Sub Never Answer ()
numberNever = numberNever + 1
ActivePresentation.SlideShowWindow.View.Next
End Sub
Sub Start()
numberAlways = 0
numberMostly = 0
numberSometimes = 0
numberSeldom = 0
numberNever = 0
ActivePresentation.SlideShowWindow.View.Next
End Sub
Sub Results ()
MsgBox “You Got ” ‘ numberAlways ‘ “ Always Answers, “ ‘ numberMostly ‘ “ Mostly Answers, “ ‘ numberSometimes ‘ “ Sometimes Answers, “ ‘ numberSeldom ‘ “ Seldom Answers, “ ‘ numberNever ‘ “ Never Answers, “ ‘ vbaApplicationModal, “ Sample Quiz “
End Sub
Sub Results()
MsgBox (“You Got ” & numberAlways & “ Always Answers, “ & numberMostly & “ Mostly Answers, “ & numberSometimes & “ Sometimes Answers, “ & numberSeldom & “ Seldom Answers, “ & numberNever & “ Never Answers " ".")
End Sub
|
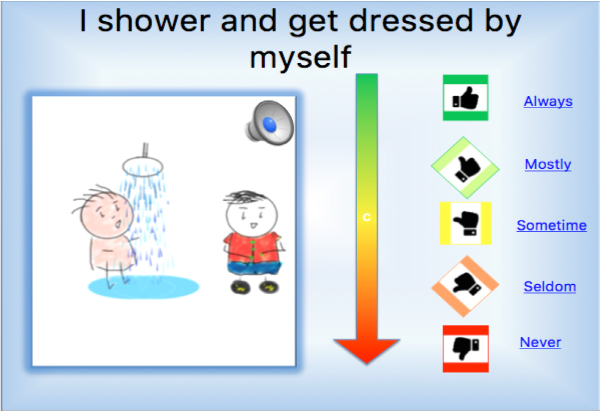
Figure 1. Sample of EITVAQ on the Physical section on Microsoft PowerPoint
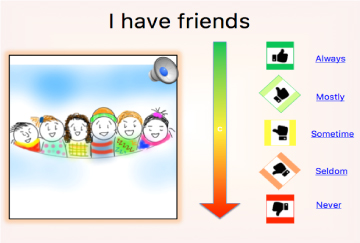
Figure 2. Sample of EITVAQ on the Social section on Microsoft PowerPoint

Figure 3. Sample of EITVAQ on the Emotion and Autonomy section on Microsoft PowerPoint
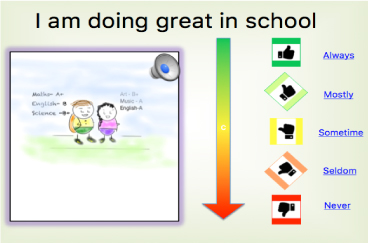
Figure 4. Sample of EITVAQ on Cognitive section on Microsoft PowerPoint
Finally, a timer would start the moment the participants clicks and initiates to begin the questionnaire.
Table 3. Sample of EITVAQ on a text version
Choose a suitable box to describe How True the following Statements are about you
I ………… |
Never 1 |
Seldom 2 |
Sometimes 3 |
Mostly 4 |
Always 5 |
Physical |
|
|
|
|
|
Get around by myself |
|
|
|
|
|
Can feed myself |
|
|
|
|
|
Go to toilet by myself |
|
|
|
|
|
Shower and get dressed by myself |
|
|
|
|
|
Can see the whiteboard clearly |
|
|
|
|
|
Can hear music clearly |
|
|
|
|
|
Can speak clearly |
|
|
|
|
|
Can write using a pen |
|
|
|
|
|
Social |
|
|
|
|
|
Go to school |
|
|
|
|
|
Have friends |
|
|
|
|
|
We play games together |
|
|
|
|
|
We watch movies together |
|
|
|
|
|
We have sleepovers |
|
|
|
|
|
We talk to each other |
|
|
|
|
|
We visit each other |
|
|
|
|
|
My family always give me the help that I need |
|
|
|
|
|
Emotional |
|
|
|
|
|
Love going to new places |
|
|
|
|
|
Love meeting new friends |
|
|
|
|
|
Like to be alone |
|
|
|
|
|
Don’t mind being different |
|
|
|
|
|
Feel bored |
|
|
|
|
|
Like to share my feelings with my friends |
|
|
|
|
|
Can take care of myself |
|
|
|
|
|
Can pay attention in class |
|
|
|
|
|
Cognitive |
|
|
|
|
|
Can follow instructions |
|
|
|
|
|
Remember what I ate for breakfast |
|
|
|
|
|
Know the date of my birthday |
|
|
|
|
|
Learn new things everyday |
|
|
|
|
|
Can count |
|
|
|
|
|
Can sing |
|
|
|
|
|
Am doing great in school |
|
|
|
|
|
My family and friends care for me |
|
|
|
|
|
Patient satisfaction Rating |
1 |
2 |
3 |
4 |
5 |
Find these questions easy to complete |
|
|
|
|
|
The TEXT format had the same question as EITVAQ. However, they were printed in 2 pages with no visual and audio aids. The primary investigator was in charged of measuring the time taken to complete the TEXT format.
Initial pilot testing
Five volunteers (staff nurses and junior doctors) in the neurosurgical unit were invited to participate in the pilot testing of the EITVAQ to ensure the questionnaire was straightforward and easy to complete without technical difficulty. Their suggestions for changes in wording or presentation style were discussed and implemented. The final list of questions was reviewed by paediatric neurosurgeons to ensure adequate breadth of coverage and appropriate categorization.
Cohort identification
Upon checking in at the main outpatient reception desk, all patients coded for hydrocephalus with shunt were given information leaflet about the study and invited to participate in this study during their waiting time in Neurosurgical outpatient department. Interested parents would approach the principal investigator at the Neurosurgical outpatient department with the signed consent forms. Inclusion and exclusion criteria were applied to all participants. All participants qualified for the study were brought to a room individually in the outpatient department and they were given EITVAQ, using a hospital- encrypted laptop and TEXT questionnaire. All participants were coded from X1-X24.
Each participant was given the choice to start with either format: EITVAQ or TEXT by their own preference. There was no time limit for each questionnaire to be completed but each format of the questionnaire was timed as described above. If any assistance was needed, they could ring the bell for help from either principal investigator or parents. The data from both questionnaires were collected for statistical analysis.
Cost
The capital cost for this trial was kept to the minimum as EITVAQ is a delivered in a PowerPoint file and it was paperless. All cost spent were only on the printing of consent forms, information sheets and questionnaires in TEXT format.
Data analysis
All data were collected from EITVAQ and TEXT both electronically and printed-paper. Both data were collected, entered and stored in Microsoft Excel. Each candidate was labeled from X1- X24 individually. Individual score sheet for EITVAQ and TEXT were stored on separate excel sheet labeled from X1-X24. All data set were compiled and organized according to the following variables:
- Participant Label: X1- X24
- Age
- Sex: Female and male
- GMFCS score :1-5
- Number of surgeries :1,2,3,4,>5
- Completion of EITVAQ: Yes/No
- Completion of TEXT: Yes/No
- Total time to complete EITVAQ
- Total time to complete TEXT
- Total Score of EITVAQ
- Total Score of TEXT
All data collected above were exported for statistical analysis using Statistical Analysis Software Package (SPSS).
The following steps were applied:
- Familiarizing with the data
- Generating initial codes and variables on SPSS
- Statistical analysis on SPSS
- Reviewing and compare both EITVAQ and TEXT
- Defining correlation between variables
- Writing and producing the report on data analyzed
Ethics
Approval from the ethics and research committee was sought from Temple Street, CUH. The study was approved and registered by the research team at Temple Street, CUH in September 2015. Signed consent from parents were obtained for those that participated in this study.
From November 2015 to June 2016, there were a total of 75 children with hydrocephalus on the neurosurgical outpatient list. All 75 parents were given information leaflets and consent forms while checking in at the reception. There were 54 participants interested in the study. However, after applying the inclusion and exclusion criteria, only 24 children participated this study. Figure 5 below explains the selection process.
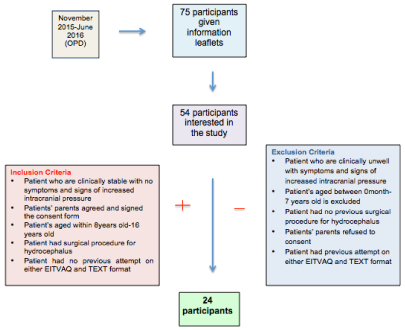
Figure 5. Participant Selection Process
Demographics
There were 14 girls and 10 boys with hydrocephalus recruited in this study. The age range was from 9-16 years old with a mean age of 12.67 and mode of 15. Out of the 24 participants, 11 (45.8%) had more than five surgical procedures, and 13 (54.2%) had less than five procedures done. Out of the 24 participants, 17 (70.8%) of the children had GMFCS of 1, 29.2% of the children had a GMFCS score of 2-4 and nobody had a GMFCS score of 5.
Statistical analysis of EITVAQ and TEXT
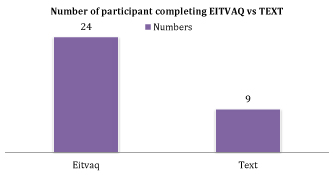
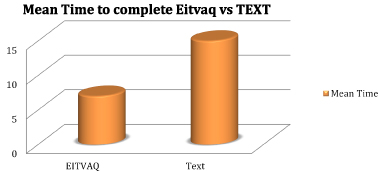
There was a 100% rate of completion for EITVAQ. However, only 9 (37.5%) of the patients managed to complete the TEXT format as shown in Graph 1. Those that completed EITVAQ required no assistance. However, those that completed the TEXT format requested assistance from parents. The mean time to complete EITVAQ was 7 minutes, whereas it took almost 15 minutes for the TEXT version to be completed with aid as shown in Graph 2.
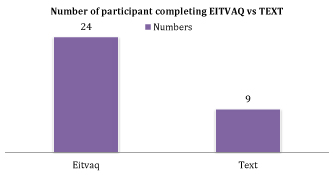
Graph 1. Number of participant complete EITVAQ vs. TEXT
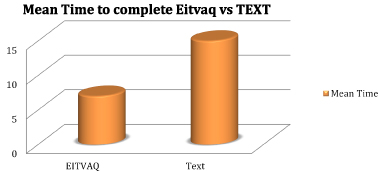
Graph 2. Mean time to complete EITVAQ vs. TEXT
EITVAQ
There were 32 questions found in EITVAQ involving 4 main domains of health: physical, mental, social and cognitive. Each domain had eight questions. Each question was scored from 1-5, where 1 = never and 5= always. The maximum score for this questionnaire was 160.
Out of 24 participants, we received 100 percent completions from all 24 participants. 92% of the participants were extremely satisfied with EITVAQ. The highest score obtained was 154 out of 160 and the lowest score obtained was 101. The mean score was 132.92. No missing data was found.
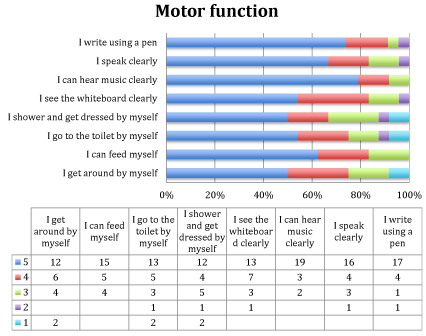
EITVAQ: Physical section
In the physical section, 50% of the participants would always mobilise and get dressed independently. 62.5% of the participants would always feed independently and 54% of the participants would always go to toilet independently. Almost 80% of the participants had no obvious hearing impairment. Nearly 50% of them had some visual problems. Over 70% of the participants could write using a pen. Graph 3 below, shows the detail findings from the physical section.
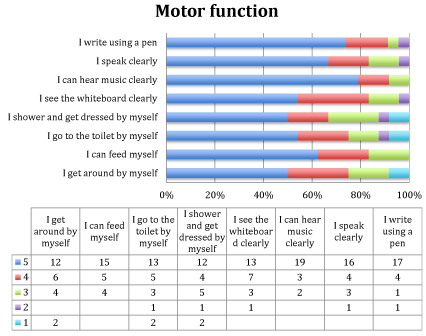
Graph 3. Results from Physical Section on EITVAQ.
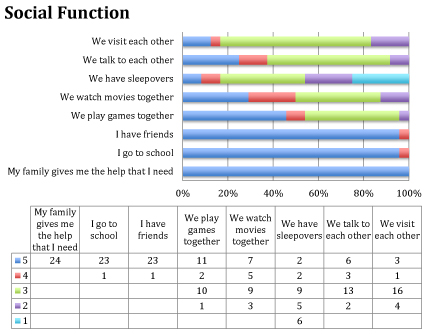
EITVAQ: Social section
In the social section, all of the participants would always get the help that they need from their family members. 96% of them claimed they would always go to school and they would always have friends. However, less than 50% of the participants would always get to socialise with their friends. Less than 50% of the participants would always get to play with their peers, only 29% would always get to watch movies together, 25% would always get to talk to their friends, 12.5% would always visit their friend, and only 8% would always get to do sleepovers. There were 25% of the participants never had a sleepover in their friend’s place. Graph 4 below, shows the detail breakdown of the Social section.
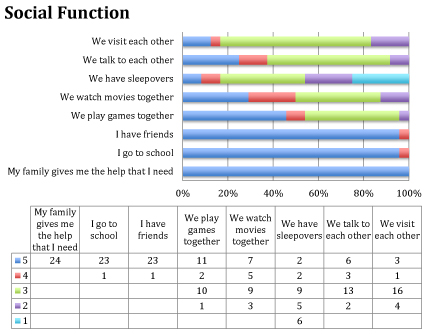
Graph 4. Results from Social Section on EITVAQ.
EITVAQ: Emotion and autonomy section
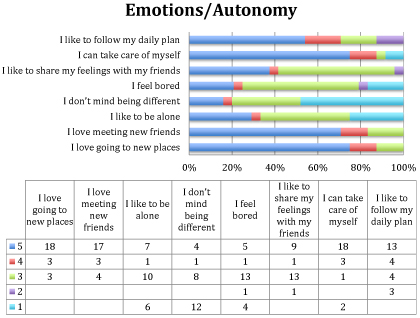
In the emotion and autonomy section, 75% claimed they could always take care of themselves and would always loved to go to new places. 54% of the participants did not mind following a daily routine. Over 70% enjoyed meeting new friends. 50% of them were self-conscious about their differences from the normal healthy peers. 21% of them would always feel bored with 54% of them feeling bored at times. 37.5% of them would always share their feeling with their friends and over 50% of them preferred to share their feelings at times. Below in graph 5, shows the breakdown details for the Emotion and Autonomy section.
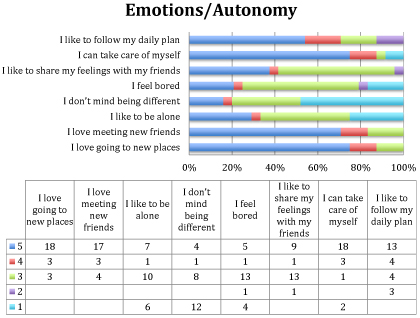
Graph 5. Results from Emotion and Autonomy Section on EITVAQ
EITVAQ: Cognitive section
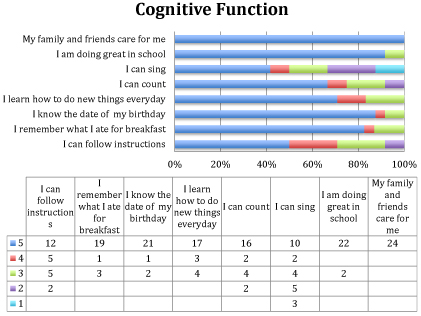
In the cognitive section, 50% of them would always be able to follow instruction. 80% of them would always remember what they ate for breakfast. 87.5% would always remember their birth date with 12.5% of them having some difficulty remembering. 92% of the participants claimed to be doing great in school. Over 70% of them were learning something new every day. 2/3 of the participants could always count with 1/3 of them having difficulty. 41.6% of the participant claimed that they could always sing with 12.5% claiming that they could never sing. All participants acknowledged that their family member and friends would always care for them. Graph 6 below, shows the detail findings from the cognitive section.
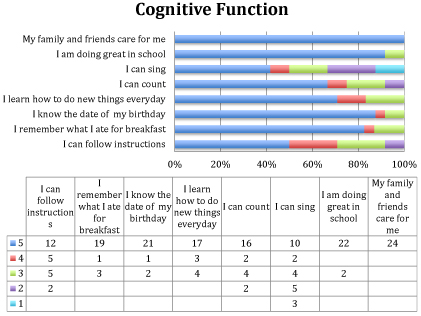
Graph 6. Results from Emotion and Autonomy Section on EITVAQ
There were 32 questions found in TEXT version involving physical, mental, social and cognitive which were the exact same set of questions as EITVAQ. The maximum score for the TEXT version was 160.
Out of 24 participants, only nine managed to complete the questionnaire. None of them were satisfied or extremely satisfied with the questionnaire. 66.7% of the participants gave a score of 3 out of 5 and the remaining 33.3% giving a score 1 out of 5. All of the participants for TEXT required parental guidance in completing the questionnaire. The 9 participants needed guidance in reading the questions to them and directing them to tick the right box. The highest score was 154 and the lowest score was 129 with a mean score of 144.22. No missing data was found in the nine sets of data obtained.
TEXT versus EITVAQ
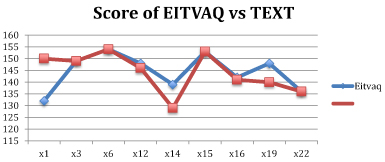
When comparing the TEXT and EITVAQ, only 4 out of the 9 participants have the same scores in both of the questionnaires. Out of the 5 participants with dissimilar scores, 4 of them were lower than EITVAQ and interestingly; one participant scored 18 points higher on TEXT in comparison to EITVAQ. The results above are described in the graph 7 below.
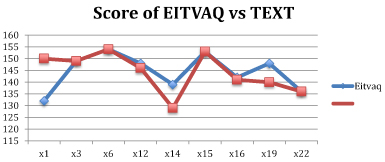
Graph 7. Scores of EITVAQ versus TEXT
Surgery versus TEXT
There were only 37.5% of the participants who had surgical procedure who were able to complete the TEXT format. Hence a statistical analysis was carried out to see if there was any correlation in the number of surgical procedures and the ability to complete the TEXT format.
There were 11 patients out of the 24 participants (45.8%) had more than five surgical procedures and 13 out of the 24 participants (54.2%) had less than five surgical procedures. Only 3 out of the 11 (27%) managed to complete the questionnaire on TEXT. Applying this data for statistical analysis, using Pearson Chi-Square Test on SPSS, the P-Value was 0.341. The results above are described in detail in Table 4.
Table 4. Results of Surgery Vs. TEXT
TEXT format |
Surgical Procedures Done in Hydrocephalus |
Total |
More than 5 Surgeries |
Less than 5 Surgeries
|
TEXT Not Complete |
8
72.7% |
7
53.8% |
15
62.5% |
TEXT Complete |
3
27.3% |
6
46.2% |
9
37.5% |
Total |
11
100.0% |
13
100.0% |
24
100.0% |
Strength and limitation (Technical and Clinical)
Strength
From reviewing current literature, there is no evidence of a health-related electronic questionnaire with visual and audio aids for children with hydrocephalus. It is shown in this study that there was a 100% rate of completion for EITVAQ and only 37.5% completion for TEXT. The completion time for EITVAQ was an average of 7 minutes whereas there the average time of completion on TEXT was almost 15 minutes. 92% of the participants in this study were extremely satisfied with EITVAQ. Such results provide an original study supporting promising results that suggest EITVAQ is a better tool to evaluate the health status of children with hydrocephalus.
There was a brief discussion with all 24 parents after they participated in the study. It was highlighted by all parents that they found their children to have the five common problems 1) poor concentration, 2) poor organisation skills, 3) short-term memory, 4) lack of flexible thinking and 5) poor self-monitoring. Despite having these educational issues, the majority of these participants attended mainstream school. Parents found them technologically savvy and had longer attention span with technology, such as video games, smartphones and laptops but often performed inadequately in school.
The top three reasons for failure to attempt of the TEXT version were 1) participants unable to concentrate, 2) participants gave up in attempting the TEXT version upon receiving it and 3) participants complaining of getting tired when trying to read the TEXT version.
Majority of the parents were surprised by the capability of their child to answer the questionnaire on EITVAQ. They were amazed by the vast difference of how quickly they could answer the questions on EITVAQ without aid. In comparison to the TEXT format, participant found it difficult to complete, leading to loss of interest to complete.
Two participants in particular had exceptional results. One participant, age 9 with a background of cerebral palsy with GMFCS score of 4 managed to complete the EITVAQ on his own in 6 minutes and 33 seconds. Participant’s parents and schoolteacher were amazed by the result achieved. Another participant with a background of spina bifida with multiple shunt revisions and very poor attention span, managed to complete EITVAQ in 6 minutes and 20 seconds.
The above findings in this study support and suggest that children with hydrocephalus requiring surgical intervention have executive function skills deficit. A paper written by Tarazi RA et al. in 2008 described a strong correlation between executive function skills deficit in patients with myelomeningocele and hydrocephalus [57]. In 2012, a study by Lacy M et al. stated that there is a strong relationship between hydrocephalus and executive function deficit [18].
All parents acknowledged the features shown on EITVAQ and suggested for further studies in using visual and audio aids as an educational tool to help better learning outcome. The study by Miller showed that different individual suits different learning methods, such as visual aids, audio aids, reading and kinesthetic aids. It was highlighted that a child’s achievement and motivation improve when learning and teaching styles are matched [56]. This suggests that if the needs of the children with hydrocephalus are met with visual and audio aids, these might help them not only to allow them to answer questionnaire or feedback from a child’s perspective but also able to help them to learn better reaching individual’s potentials.
EITVAQ and quality of life
EITVAQ was designed to be a disease-specific quality of life questionnaire for children with hydrocephalus. It looked at the physical, emotional, social and cognitive well being of a child with hydrocephalus. The highest score of EITVAQ was 156 out of 160 and the lowest score of EITVAQ was 101 out of 160. The mean score of the 24 participants were 132.9 /160, 83% satisfactory score.
This mean score is 16% higher than the mean score of HOQ 0.67 (ranging from 0-1) published by Kulkarni AV et al. in 2007. HOQ was used to assess quality of life among hydrocephalus patient completed by proxy. Such result highlights that parents tend to underestimate their cognitive and social competence from the patient perspective. This showed that parents or carers cannot replace the voice of the patient [58].
Almost 20% of the participants had some hearing impairment. Nearly 50% of them had some visual problems. Over 30% of the participants could not write using a pen. However, there was a 100% of completion rate of EITVAQ. This suggests that visual and audio aid like EITVAQ can facilitate their needs to overcome issues faced on a printed TEXT version.
Furthermore, it is also interesting to note that 70% of the participants could write using a pen but fell short in being able to complete the TEXT format. This suggests that failure to complete or attempt TEXT format is not secondary to a physical disability alone but probably a central cause, such as learning disability secondary to executive function deficits.
In the social section, all of the participants would always get the help that they need from their family members. 96% of them claimed they would always go to school, with one participant attending homeschool session leading to limited social circle. However, less than 50% of the participants got to socialise with their friends, such as playing with their peers, watching movies together, talking to their friends, visiting their friends and having sleepovers. The result above suggests that patients with hydrocephalus are well cared for by their family members. Despite 96% of the participants attending school and having friends, they were deprived of socialising activities. This is likely due to their complex medical condition that might cause an underestimation of their social capabilities and over protection from parental care. It is highly recommended that children with hydrocephalus should form a support group, organizing indoor and outdoor activities that are tailored according to their needs.
In the emotion and autonomy section, 75% claimed they could take care of themselves and always loved going to new places. Over 70% of them loved meeting new friends. 54% of the participants did not mind following a daily routine. 50% of them were self-conscious about their differences from the normal healthy peers and preferred to share their feelings at times. Such results implied that the participants were seeking autonomy and wish to take charge of their lives, exploring new places and meeting new people. However, due to the participants’ self awareness being different from their healthy peers, such emotions could have dampened their will to lead their life and subsequently depriving them from having a normal social life. Such results might suggest the possibility of parents or carers over protecting their child from a young age and also the possibility of children with hydrocephalus having a low self-esteem in comparison to healthy children.
In the cognitive section, all participants acknowledged that their family member and friends care for them. 50% of them would always be able to follow instruction with the other half having difficulty. 20% of them found to have short-term memory problems forgetting what they had for breakfast. 12.5% of them found to have long-term memory issue, forgetting their birthday. 1/3 of the participants claimed that they have difficulty counting. Interestingly, despite having the result above, 92% of them claimed to be doing great in school. This might suggest that children with hydrocephalus had a different of perception of a normal cognitive function when compared to a normal population. Also with 50% having difficulty following instruction and 1/3 having trouble counting with some having short and long-term memory problems emphasized the fact that children with hydrocephalus are likely to have executive function deficit. Such results are in keeping with study published by Lacy M et al. [16,18].
The overall health condition of hydrocephalus refrained patients of being entirely independent. Although majority of them used walking aids and/or wheelchair to mobilise, there were still limitations to being fully independent, such as going to the toilet independently. Children with hydrocephalus that required surgical intervention would often need close monitoring and regular check ups. Some of them experienced complications of shunt insertion causing them to be deprived of independence and socialising with their peers. This led them to feel bored, redrawn and more self-conscious about their differences affecting their emotions.
A lot of parents felt that their children often struggled to control their emotion and speech impulse when they were with their friends. They would overreact when receiving negative comments or critics. Also, they noticed that their children would often say inappropriate comments, which might sometimes cause misunderstanding among friends and new friends. All these subtle signs correlate with typical characteristic of a child with executive function deficit. Hence, this could explain why over 50% of the participants preferred not to share their feelings with their friends and over 35% of the participants preferred to be alone. This is likely because they are afraid to be judged, hurt and ‘alienated’ by their friends.
EITVAQ and TEXT
When comparing the scores between those that completed both EITVAQ and TEXT, there were four that had a lower score on TEXT and one scored 18 points higher than EITVAQ. The reason that explains a lower score on TEXT might be because of parents’ assistance and help affecting the actual score from the child’s perspective.
The participant that had a higher score on TEXT by 18 points in comparison to EITVAQ was a 10 year old girl with a background of autistic spectrum disorder, born at 30 weeks with congenital hydrocephalus and had 2 previous shunt revisions. No parental assistant were requested. It is very likely that the child’s answers were inaccurate, resulting in such score discrepancy.
Surgery and TEXT format
There were 11 patients out of the 24 participants (45.8%) had more than five surgical procedures and 13 out of the 24 participants (54.2%) had less than five surgical procedures. Only 3 out of the 11 (27%) managed to complete the questionnaire on TEXT. Using Pearson Chi-Square Test on SPSS, such statistical analysis was applied to see if there is any correlation between the number of surgery and the number of TEXT format completion. The P-Value found was 0.341.
Although the P –Value was not statistically significant, however in percentage, there was an 18.9% difference between the two groups: more than five surgeries and less than five surgeries.
Such percentage differences suggest to us that the number of surgical procedures affected the ability to complete. The current P-value in this study is not convincing likely because of the lack of samples in this study.
Physical disablities and TEXT format
Results in this study showed that 9 out of the 24 participants (37.5%) completed the questionnaire. Out of the 9 participants, 66.7% of them had normal physical mobility status and 33.3% of them had a physical disability. By applying statistical analysis, using Pearson Chi-Square Test on SPSS, the P-Value was 0.728. The P value was not statistically significant. This suggests that there were no relation between physical disability and the ability to complete the TEXT format.
TEXT, GMFCS and surgery
By looking at the relationship between the three variables, the result highlighted that the main issue of failure to complete the TEXT format is unlikely secondary to a physical cause but likely a central cause.
Although there were no missing data in this study but the main limitation to this study was small sampling. The study design could have been improved by doing a randomization on which format of questionnaire they get to do first. Although with such small sample it would not have made a tremendous impact, however it should be implemented for a better study design.
It could have been better to enlarge the sampling size by targeting children with hydrocephalus that attended in emergency department or admitted to the ward. However, in this study, children that were clinically unstable were excluded, as that could have been a confounding factor potentially affecting this study’s result.
It was clearly shown that there were 100% respondents for EITVAQ and only 37.5% respondents for the TEXT version, this showed that this study was a good qualitative study but poor quantitatively. With only 9 cases to compare between EITVAQ and TEXT, the small study sample for statistical analysis would be weak and unreliable.
Although there was 100% respondent for EITVAQ, there might be some inaccuracy of answers, as hydrocephalus patients would often have complex medical background with various cognitive function levels. Although there was only one participant found to have a significant discrepancy between two questionnaires’ score, however, this could not out rule the possibility of having other participants answering inaccurately.
The mean score of the 24 participants were 132.9/160, 83% satisfactory score. This result apperared to be 16% higher than the mean result published in 2007 by Kulkarni AV et al. [58]. Looking through EITVAQ, it was highlighted that in the social section that there were three redundant questions that enquired about the participation of children with hydrocephalus in the community versus an actual social activity question that could have extracted more socialising pattern in this study. These 3 redundant questions could have possibly contributed to an overall increased of mean score of EITVAQ when comparing with HOQ as published by Kulkarni AV et al.
The small sample and short duration of this study limited the possibilities of test and retest for the reliability of EITVAQ. Furthermore, with a larger sample and longer duration, EITVAQ could be developed into a validated tool in measuring a disease-specific health status questionnaire for children with hydrocephalus.
Nevertheless, this pilot study showed an encouraging result supporting the answer that EITVAQ is provisionally a better tool than TEXT questionnaire to evaluate the health status of paediatric hydrocephalus patients from the child’s perspective. Further study is necessitated to assess the reliability and validating of EITVAQ.
It is indeed encouraging to receive feedback from parents to support this study not only in developing a validated questionnaire but also highlighting the fact that children with hydrocephalus are associated to have executive function deficit. It is worth exploring the benefits of visual, audio and kinesthetic aids in the development of education tool for hydrocephalus patient. This will enable children with hydrocephalus to be able to learn and complete their education to their full potentials.
In summary, this study showed positive results suggesting that EITVAQ is a better tool in evaluating the health status of children with hydrocephalus, as it is tailored according to their disability needs. Future research is imperative in this area to validate this tool as there is a growing number of the survival rate of children with hydrocephalus. It will also be interesting to see how visual and audio aids will help in development of new skills and improve executive function.
Implications for practice
This was a pilot crossover prospective study to see if EITVAQ would be a better tool to evaluate the health status of paediatric hydrocephalus patients.
EITVAQ was designed to be disease-specific quality of life questionnaire by accommodating the needs of children with hydrocephalus. This study qualitatively proved that it is a better tool with a 100% respondent rate in comparison to the TEXT version.
However, being a pilot study, there were limitation on the numbers and the duration of the study. In the long term, EITVAQ is targeted to be tested and retested for its reliability and also to be validated as a useful tool to measure the quality of life and evaluate the long-term impact of children with hydrocephalus. After validating EITVAQ, potential refining and development of EITVAQ from PowerPoint format into an encrypted smartphone application will be the ultimate goal to enable widespread usage among registered practitioners neurosurgeons and paediatricians to assess the health status of the child with hydrocephalus. Potentially, EITVAQ will be applicable for other children with epilepsy, head injury and brain tumours.
Also, from the parents’ feedback, they were amazed by their child’s capability of answering the question without aid. All of the parents wished that further development of EITVAQ will enable an electronic, visual and audio automated education material to stretch the hidden potential of their child’s learning capability.
This study highlights the fact that EITVAQ is able to meet and to accommodate the disability of children with hydrocephalus. Interestingly in this study, the results were able to suggest that the inability to complete the TEXT format was not just purely due to physical disability but also a central cause, proposing the possibility of executive function deficit.
Implications for research
The results in this study creates a huge room for further research, which includes refining the questions of EITVAQ with more targeted and specific questions.
Additional extension of this study can be taken further in validating the tool and developed into a smartphone and/or smart tablet application. This will enable touch screen function for accommodating children with hydrocephalus that might have a GMFCS score of 5, covering a wider scope of participants (Table 5).
Table 5. Results of GMFCS score Vs. TEXT
TEXT format |
GMFCS Score |
Total |
1.00 |
>2.00 |
TEXT not completed |
11
64.7% |
4
57.1% |
15
62.5% |
TEXT completed |
6
35.3% |
3
42.9% |
9
37.5% |
Total |
17
100.0% |
7
100.0% |
24
100.0% |
It will be interesting to have future research in identifying executive function deficit among children with hydrocephalus using Behavioral Rating Inventory of Executive Function (BRIEF), a well validated tool to detect executive function deficit [59]. Children with hydrocephalus can be then taught a new skill using visual, audio and/or kinesthetic aid for a 6 weeks period. After developing the new skill, executive function can be retested during the 8th-week period. This will help to verify if children with hydrocephalus has executive function deficit. It will also verify if visual, audio and kinesthetic aids will enable children with hydrocephalus to learn a new skill effectively. Finally by repeating the executive function test, it will verify if visual, audio and/or kinesthetic aids help to stretch the potential of the learning capability and improve executive function skills of children with hydrocephalus.
Schraegle WA and Titus JB recently published a study about on the role of using BRIEF to screen executive dysfunction among children with epilepsy and how it could be used to identify those at risk of poor quality of life [60]. This study proposed that future study is crucial in verifying a relation between executive function skills improvement and how it might improve quality of life. This opens another research topic to verify if improvement in executive function skills will subsequently improves the total overall quality of life among patient by using EITVAQ. Having mentioned future studies above, EITVAQ can be potentially developed into a successful validated tool in measuring health status of children with hydrocephalus and applied in further research in assessing the long-term outcome among children with hydrocephalus.
In conclusion, the results of this pilot study over a seven months period were in favour of EITVAQ being a better tool to measure the health status in paediatric hydrocephalus patients.
In addition to the positive feedback, EITVAQ managed to exceed the expectation of parents and educators. This led parents to propose for further development of electronic, visual and audio aided education material to enhance the learning potential of their child’s learning capability.
Currently, on top of physical disabilities, children with hydrocephalus are often noted to have some degree of long term functional deficits, which includes visual motor integration, executive function, motor skills and behavioural outcome [29]. Although in this study it was noted that majority of these children would attend normal stream school and often fall short academically. The lack of awareness of such arising problem calls for future research by applying various technology aid similar to EITVAQ to bridge the gap and stretch their learning potentials and discovering their talents. This will help them to gradually build their future prospect academically, emotionally and financially, enabling them to fully integrate into the society in adulthood, gaining social independence.
In summary, the results of this study supported and suggested that EITVAQ is a better tool to evaluate the health status of paediatric hydrocephalus patients as it is tailored according to their disability needs. In the future, EITVAQ is hoped to be a validated, interactive and child friendly tool to be used widespread across hydrocephalus patients to provide baseline background information for multidisciplinary teams to allow smooth transition and integration to adult health services and community in the future.
View supplementary data
- Kahle KT, Kulkarni AV, Limbrick DD Jr, Warf BC (2016) Hydrocephalus in children. Lancet 387: 788-799. [Crossref]
- Tully HM, Dobyns WB (2014) Infantile hydrocephalus: a review of epidemiology, classification and causes. Eur J Med Genet 57(8): 359-368. [Crossref]
- Warf BC (2005) Hydrocephalus in Uganda: the predominance of infectious origin and primary management with endoscopic third ventriculostomy. J Neurosurg 102 (suppl): 1-15. [Crossref]
- Warf BC, Alkire BC, Bhai S, Hughes C, Schiff SJ, et al. (2011) Costs and benefits of neurosurgical intervention for infant hydrocephalus in sub-Saharan Africa. J Neurosurg Pediatr 8(5): 509-521. [Crossref]
- Stone SS, Warf BC (2014) Combined endoscopic third ventriculostomy and choroid plexus cauterization as primary treatment for infant hydrocephalus: a prospective North American series. J Neurosurg Pediatr 14(5): 439-446. [Crossref]
- Kulkarni AV, Riva-Cambrin J, Butler J, Browd SR, Drake JM, et al. (2013) Outcomes of CSF shunting in children: Comparison of Hydrocephalus Clinical Research Network cohort with historical controls: clinical article. J Neurosurg Pediatr 12(4): 334-338. [Crossref]
- Garne E, Loane M, Addor MC, Boyd PA, Barisic I, et al. (2010) Congenital hydrocephalus--prevalence, prenatal diagnosis and outcome of pregnancy in four European regions. Eur J Paediatr Neurol 14 (2): 150-155. [Crossref]
- Yamasaki M, Nonaka M, Suzumori N, Nakamura H, Fujita H, et al. (2011) Prenatal molecular diagnosis of a severe type of L1 syndrome (X-linked hydrocephalus). J Neurosurg Pediatr 8(4): 411-416. [Crossref]
- Drake JM, Kestle JR, Milner R (1998) Randomized trial of cerebrospinal fluid shunt valve design in pediatric hydrocephalus. Neurosurgery 43(2): 294-305. [Crossref]
- Kulkarni AV, Drake JM, Mallucci CL, Sgouros S, Roth J, et al. (2009) Endoscopic third ventriculostomy in the treatment of childhood hydrocephalus. J Pediatr 155: 254-259. [Crossref]
- Tuli S, Drake J, Lawless J (2000) Risk factors for repeated cerebrospinal shunt failures in pediatric patients with hydrocephalus. J Neurosurg 92(1): 31-38. [Crossref]
- Donders J, Rourke BP, Canady AI (1992) Emotional adjustment of children with hydrocephalus and of their parents. J Child Neurol 7(4): 375-380. [Crossref]
- Mari M, Carme J, Maria AP, Juan S (2001) Neuropsychological findings in congenital and acquired childhood hydrocephalus. Neuropsychol Rev 11(4): 169-178. [Crossref]
- Hampton LE, Fletcher JM, Cirino P, Blaser S, Kramer LA, et al. (2013) Neuropsychological profiles of children with aqueductal stenosis and Spina Bifida myelomeningocele. J Int Neuropsychol Soc 19(2): 127-136. [Crossref]
- Dalen K, Bruarøy S, Wentzel-Larsen T, Laegreid LM (2008) Intelligence in children with hydrocephalus, aged 4-15 years: a population-based, controlled study. Neuropediatrics 39(3): 146-150. [Crossref]
- Lacy M, Pyykkonen BA, Hunter SJ, Do T, Oliveira M, et al. (2008) Intellectual functioning in children with early shunted posthemorrhagic hydrocephalus. Pediatr Neurosurg 44(5): 376-381. [Crossref]
- Smith AD, Buckley MG (2012) Spatial navigational impairments in hydrocephalus. Cogn Process 13 (suppl 1): 329-332. [Crossref]
- Lacy M, Baldassarre M, Nader T, Frim D (2012) Parent ratings of executive functioning in children with shunted hydrocephalus. Pediatr Neurosurg 48(2): 73-79. [Crossref]
- Lindquist B, Persson EK, Uvebrant P, Carlsson G (2008) Learning, memory and executive functions in children with hydrocephalus. Acta Paediatr 97: 596-601. [Crossref]
- Lindquist B, Persson EK, Fernell E, Uvebrant P (2011) Very long-term follow-up of cognitive function in adults treated in infancy for hydrocephalus. Childs Nerv Syst 27: 597-601. [Crossref]
- Kulkarni AV (2010) Quality of life in childhood hydrocephalus: a review. Childs Nerv Syst 26: 737-743. [Crossref]
- Persson EK, Hagberg G, Uvebrant P (2006) Disabilities in children with hydrocephalus--a population-based study of children aged between four and twelve years. Neuropediatrics 37(6): 330-336. [Crossref]
- Rekate HL, Kranz D (2009) Headaches in patients with shunts. Semin Pediatr Neurol 16: 27-30. [Crossref]
- Gupta N, Park J, Solomon C, Kranz DA, Wrensch M, et al. (2007) Long-term outcomes in patients with treated childhood hydrocephalus. J Neurosurg 106: 334-339. [Crossref]
- Kulkarni AV, Rabin D, Drake JM (2004) An instrument to measure the health status in children with hydrocephalus: the Hydrocephalus Outcome Questionnaire. J Neurosurg 101(2 Supp): 134-140. [Crossref]
- Hansen D, Vedantam A, Briceño V, Lam SK, Luerssen TG, et al. (2016) Health-related quality of life outcomes and level of evidence in pediatric neurosurgery. J Neurosur Pediatr.
- Hoppe-Hirsch E, Laroussinie F, Brunet L, Sainte-Rose C, Renier D, et al. (1998) Late outcome of the surgical treatment of hydrocephalus. Childs Nerv Syst 14: 97-99. [Crossref]
- Jones HC, Klinge PM (2008) Hydrocephalus 2008, 17–20th September, Hannover Germany: A Conference Report. Cerebrospinal Fluid Research 2008. Cerebrospinal Fluid Res 5:19. [Crossref]
- Holwerda JC, Van Braeckel KN, Roze E, Hoving EW, Maathuis CG, et al. (2006) Functional outcome at school age of neonatal post-hemorrhagic ventricular dilatation. Early Hum Dev 96:15-20. [Crossref]
- Adams-Chapman I, Hansen NI, Stoll BJ, Higgins R (2008) Neurodevelopmental outcome of extremely low birth weight infants with posthemorrhagic hydrocephalus requiring shunt insertion. Pediatrics 121 (5): 1167-1177. [Crossref]
- Brouwer A, Groenendaal F, van Haastert IL, Rademaker K, Hanlo P, et al. (2008) Neurodevelopmental outcome of preterm infants with severe intraventricular hemorrhage and therapy for post-hemorrhagic ventricular dilatation. J Pediatr 152 (5): 648-654. [Crossref]
- Srinivasakumar P, Limbrick D, Munro R, Mercer D, Rao R, et al. (2013) Posthemorrhagic ventricular dilatation-impact on early neurodevelopmental outcome. Am J Perinatol 30(3): 207-214. [Crossref]
- Vollmer B, Roth S, Riley K, Sellwood MW, Baudin J, et al. (2006) Neurodevelopmental outcome of preterm infants with ventricular dilatation with and without associated haemorrhage. Dev Med Child Neurol 48(5): 348-352. [Crossref]
- Dalen K, Bruarøy S, Wentzel-Larsen T, Laegreid LM (2008) Intelligence in children with hydrocephalus, aged 4-15 years: a population-based, controlled study. Neuropediatrics 39: 146-150. [Crossref]
- Brouwer AJ, van Stam C, Uniken Venema M, Koopman C, Groenendaal F, et al. (2012) Cognitive and neurological outcome at the age of 5–8 years of preterm infants with post-hemorrhagic ventricular dilatation requiring neurosurgical intervention. Neonatology 101(3): 210-216. [Crossref]
- Lindquist B, Carlsson G, Persson EK, Uvebrant P (2005) Learning disabilities in a population-based group of children with hydrocephalus. Acta Paediatr 94: 878-883. [Crossref]
- World Health Organization (1946) WHO: WHO Definition of Health. New York.
- Eiser C, Jenney M (2007) Measuring quality of life. Arch Dis Child 92: 348-350. [Crossref]
- Varni JW, Seid M, Kurtin PS (2001) PedsQL 4.0: reliability and validity of the Pediatric Quality of Life Inventory version 4.0 generic core scales in healthy and patient populations. Med Care 39(8): 800-812. [Crossref]
- Vetter TR, Bridgewater CL, McGwin G (2012) An observational study of patient versus parental perceptions of health-related quality of life in children and adolescents with a chronic pain condition: who should the clinician believe? Health Qual Life Outcomes 10:85. [Crossref]
- Horsman J, Furlong W, Feeny D, Torrance G (2003) The Health Utilities Index (HUI®): concepts, measurement properties and applications. Health Qual Life Outcomes 1:54. [Crossref]
- Tarride JE, Burke N, Bischof M, Hopkins R B, Goeree L, et al. (2010) A review of health utilities across conditions common in paediatric and adult populations. Health Qual Life Outcomes 8:12. [Crossref]
- Vogel T, Verrips GHW, Koopman HM, Theunissen NCM, Fekkes M, et al. (2004) TACQOL Manual. Leiden: Leiden Centre for Child Health and Pediatrics Publishing.
- Raat H, Mangunkusumo RT, Landgraf JM, Kloek G, Brug J (2007) Feasibility, reliability and validity of adolescent health status measurement by the Child Health Questionnaire Child Form (CHQ-CF): Internet administration compared with the standard paper version. Qual Life Res 16(4): 675-685. [Crossref]
- Fitzpatrick R, Davey C, Buxton MJ, Jones DR (1998) Evaluating patient-based outcome measures for use in clinical trials. Health Technol Assess 2(14): 1-74. [Crossref]
- Schmidt LJ, Garratt AM, Fitzpatrick R (2001) Instruments for Children and Adolescents: A Review. Patient-reported Health Instruments Group to the Department of Health.
- Langeveld JH, Koot HM, Loonen MC, Hazebroek-Kampsch- reur AA, Passchier J (1996) A quality of life instrument for adolescents with chronic headache. Cephalalgia 16(3): 183-196. [Crossref]
- Ronen GM, Streiner DL, Rosenbaum P; Canadian Pediatric Epilepsy Network (2003) Health-related quality of life in children with epilepsy: development and validation of self-report and parent proxy measures. Epilepsia 44: 598-612. [Crossref]
- Apajasalo M, Rautonen J, Holmberg C, Sinkkonen J, Aalberg V, et al. (1996) Quality of life in pre-adolescence: a 17-dimensional health-related measure (17D). Qual Life Res 5: 532-538. [Crossref]
- Apajasalo M, Rautonen J, Holmberg C, Sinkkonen J, Aalberg V, et al. (1996) Quality of life in early adolescence: a sixteen-dimensional health-related measure (16D). Qual Life Res 5(2): 205-211. [Crossref]
- Raphael D, Rukholm E, Brown I, Hill-Bailey P, Donato E. (1996) The Quality of Life Pro le—Adolescent Version: background, description, and initial validation. J Adolesc Health 19(5): 366-375. [Crossref]
- Starfield B, Bergner M, Ensminger M, Riley A, Ryan S, et al. (1993) Adolescent health status measurement: development of the Child Health and Illness Profile. Pediatrics 91(2): 430-435. [Crossref]
- Stein RE, Jessop DJ (1990) Functional status II(R). A measure of child health status. Med Care 28 (11): 1041-1055. [Crossref]
- Rocque BG, Bishop ER, Scogin MA, Hopson BD, Arynchyna AA, et al. (2015) Assessing health-related quality?of life in children with spina bifida. J Neurosurg Pediatr 15 (2): 144-149. [Crossref]
- Hoppe-Hirsch E, Laroussinie F, Brunet L, Sainte-Rose C, Renier D, et al. (1998) Late outcome of the surgical treatment of hydrocephalus. Childs Nerv Syst 14: 97-99. [Crossref]
- Miller P (2001) Learning styles: The multimedia of the mind. Educational Resources Information Centre, US Department of Education. Report number: ED451140.
- Tarazi RA, Zabel TA, Mahone EM (2008) Age-related differences in executive function among children with spina bifida/hydrocephalus based on parent behavior ratings. Clin Neuropsychol 22(4): 585-602. [Crossref]
- Kulkarni AV, Shams I (2007) Quality of life in children with hydrocephalus: results from the Hospital for Sick Children, Toronto. J Neurosurg 107: 358-364. [Crossref]
- Schraegle WA, Titus JB (2016) Executive function and health-related quality of life in pediatric epilepsy. Epilepsy Behav 62: 20-6. [Crossref]