The glandular odontogenic cyst is an infrequent cyst of odontogenic origin, seen in maxilla or mandible, with an unpredictable and possibly aggressive behavior. It also has the tendency to grow to a large size and predisposition towards recurrence. It is also known as Sialo-Odontogenic Cyst. GOC can be easily misdiagnosed microscopically as a central muco epidermoid carcinoma. The diagnosis of GOC can be extremely difficult due to the rarity of the cyst and lack of clear diagnostic criteria. This article reports a case of GOC in a 45-year-old male and discusses the clinical, radiological and histopathological features of GOC.
Odontogenic cyst, Glandular cyst, Mandible, Multilocular
Glandular odontogenic cyst (GOC) is an uncommon jaw bone cyst of odontogenic origin, first described in 1988 by Gardner et al. [1] as a distinct clinicopathologic entity. In 1987, Padayachee and Van Wyk et al. [2] reported two cases that were similar to Botryoid odontogenic cyst (BOC) but with a glandular element and proposed the term ‘Sialo odontogenic cyst’. The GOC is included in the WHO histologic typing of odontogenic tumors under the terms GOC or Sialo odontogenic cyst. To the best of our knowledge, less than 200 cases of GOC has been reported in the literature and Magnusson et al. [3] observed that only 0.012% of the cysts seen on the oral cavity have fulfilled the criteria of GOC microscopically. Clinically, the most common site of occurrence is mandibular anterior region, presenting as an asymptomatic slow growing swelling. GOC occurs mostly in the middle age and has a slight male predilection. Radiologically, these cysts may be unilocular or multilocular with a well-defined border. Radiologically, when the GOC shows multilocularity in the mandibular posterior area, many lesions such as ameloblastoma, odontogenic keratocyst, central giant cell granuloma, aneurismal bone cyst, radicular cyst, most importantly low-grade MEC, must be considered in the differential diagnosis. Histologically, GOC is characterized by a cyst wall lining of non-keratinized epithelium, with papillary projections, nodular thickenings, mucous filled clefts, and ‘mucous lakes’. It also includes cuboidal basal cells, sometimes vacuolated. Treatment of GOC includes curettage and enucleation, although some authors believe marginal resection to be more reliable treatment, due to tendency of the cyst to recur after curettage and enucleation.
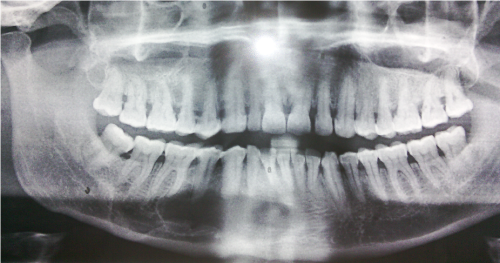
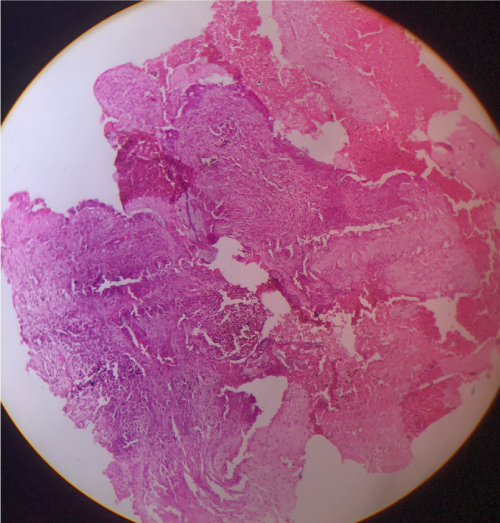
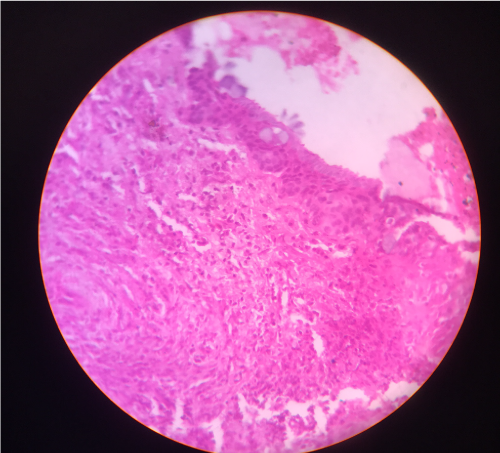
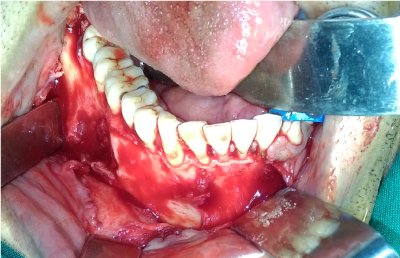
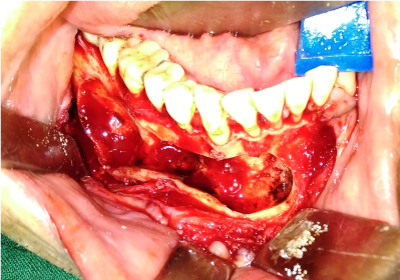
A 45-year-old Indian male patient (Figure 1) was referred to our department with a chief complaint of pain swelling in the anterior mandible for the past 4 weeks. He gave a history of trauma to the chin 2 years back. Intraoral examination revealed obliteration of vestibule from 42 to 45 and swelling in 46 and 47 region (Figure 2). The swelling was soft and tender on palpation. The overlying mucosa was slightly inflamed. No pus discharge or ooze of any kind of fluid was observed. There was no sensory loss. Panoramic radiograph (Figure 3) revealed multilocular radiolucency extending from 42 to 47, with displacement of roots of 43, 42, 41 and resorption of roots irt 43, 44, 45 was observed. A CT scan (Figure 4,5) showed resorption of buccal cortical plate in the posterior mandible. The provisional diagnosis of Ameloblastoma and keratocystic odontogenic tumor were considered. Aspiration yielded a serous brownish red colored fluid. An incisional biopsy revealed nonkeratinized stratified squamous epithelium lining with a flat interface with subsequent stroma. The epithelium shows plaque-like thickenings and whirling pattern of squamous epithelial cells. Other areas of epithelium showed pseudo-glandular pattern with few ciliated and mucus cells. Histopathology (Figure 6,7) was suggestive of glandular odontogenic cyst. Complete enucleation with removal of entire cystic lining and curettage were performed under General Anaesthesia (Figure 8,9). Primary closure was possible. Specimen was sent for histopathology, which again revealed glandular odontogenic cyst. One-year follow-up the case has revealed no recurrence.

Figure 1. Pre-operative photo

Figure 2. Intra operative defect
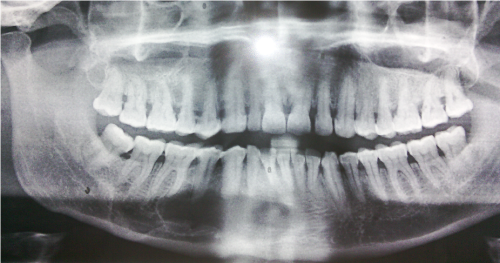
Figure 3. Pre-operative OPG

Figure 4. Pre-operative CT scan

Figure 5. Pre-operative CT scan – Showing buccal cortex erosion
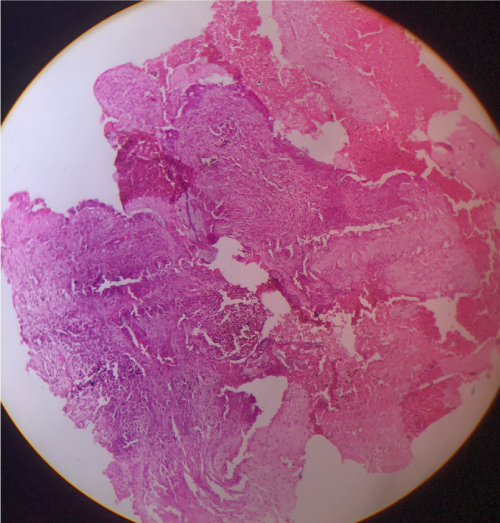
Figure 6. Histopathology picture 4x
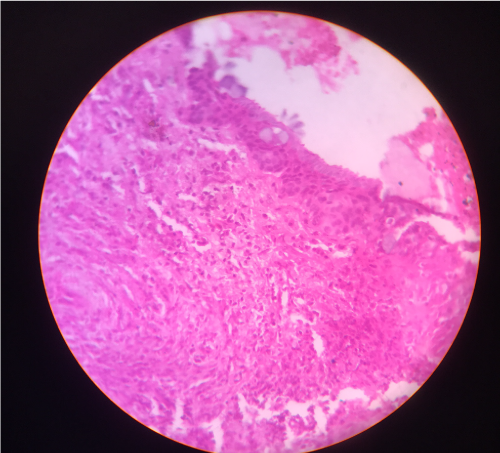
Figure 7. Histopathology picture 10x
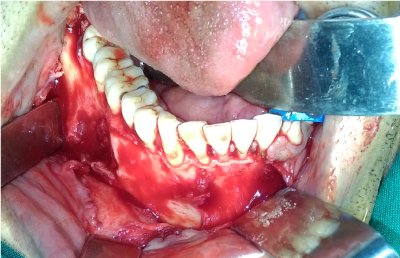
Figure 8. Intra operative defect after enucleation
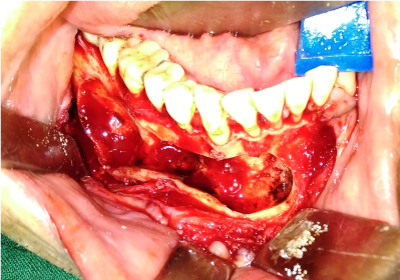
Figure 9. After closure
Glandular odontogenic cyst is an uncommon cyst of the jaw bone with only about 181 cases described till date, since it was first described by Padayache and Van Wyk [2] in 1987. They described two multilocular cystic lesions with histological features similar to that of botryoid odontogenic cyst with the lining epithelium containing areas of cuboidal or columnar epithelium and scattered foci of mucous cells and termed it as ‘‘sialo-odontogenic cyst’’. A year later Gardener et al. [1] described eight cases with similar histological features and suggested the term Glandular Odontogenic Cyst. In 1992, the second edition of the World Health Organization's (WHO) histological classification of odontogenic tumours recognized it as “a cyst arising in the tooth-bearing areas of the jaws and characterized by an epithelial lining with cuboidal or columnar cells both at the surface and lining crypts or cyst-like spaces within the thickness of the epithelium,” and retained the term glandular odontogenic cyst. The GOC is a rare lesion with a frequency rate of only 0.012% as observed by Magnusson et al. [3]. Faisal et al. [4] reported 181 GOC cases in their literature review.
GOC may mimic a wide clinicopathologic spectrum ranging from lateral periodontal cyst to a destructive malignant neoplasm such as Central Mucoepidermoid Carcinoma. There is a slight male predilection and commonly seen in middle age group and more predilection in mandible than maxilla was observed. Radiographic appearance is nonspecific. Radiographically, the GOC is localized intraosseously and may appear as a multilocular or unilocular radiolucent lesion with well-defined borders. Sometimes it may present with peripheral osteosclerotic border and scalloping, root resorption and displacement of the teeth. The clinical and radiographic findings of GOC are varied and often not pathognomonic and usually, it presents as asymptomatic slow growing lesion but occasionally may be accompanied by pain [5,6]. The water clear, low viscosity aspiration fluid content may be a helpful clinical indication of GOC, and a preoperative aspiration and fluid inspection may be advisable.
Histopathologically the present two cases consisted of certain characteristic features of GOC like non-keratinized stratified epithelium, epithelial whorls or spheres within the lining, eosinophilic cuboidal or columnar cells which are occasionally ciliated and presence of mucous cells with microcystic areas [6]. Histopathologically GOC should be differentiated from Lateral Periodontal Cyst, BOC, and Central Mucoepidermoid Carcinoma as they exhibit considerable overlap of histological features. LPC is a developmental odontogenic cyst lined by thin non-keratinized epithelium and also exhibits focal epithelial thickenings and glycogen rich epithelial cells, similar to those observed in GOC’s. BOC is a locally aggressive polycystic variant of LPC, shows similar histomorphologic feature with those of GOC, like epithelial plaques and areas of glycogen rich clear cells [7]. The differentiation of low grade Central Mucoepidermoid Carcinoma from GOC especially its multicystic variant is more important and difficult. Significant histological overlap exists between GOC and CMEC. Immunostaining with CK-18 and 19 and their positivity in GOC may help in differentiating GOC from CMEC.
In their review Kaplan et al. [8]. divided the microscopic characteristic of GOC into major and minor criteria, to facilitate its diagnosis. According to this author, a certain diagnosis of GOC could be made with the presence of all the major signs.
The major criteria include: 1. Squamous epithelial lining, with a flat interface with the connective tissue wall, lacking basal palisading. 2. Epithelium exhibiting variations in thickness along the cystic lining with or without epithelial ‘‘spheres’’ or ‘‘whorls’’ or focal luminal proliferation. 3. Cuboidal eosinophilic cells or ‘‘hob-nail’’ cells. 4. Mucous cells with intraepithelial mucous pools, with or without crypts lined by mucous-producing cells. 5. Intraepithelial glandular, microcystic or duct-like structures.
The minor criteria include: 1. Papillary proliferation of the lining epithelium. 2. Ciliated cells. 3. Multicystic or multiluminal architecture. 4. Clear or vacuolated cells in the basal or spinous layers.
According to Kaplan et al. [8]. the aggressive biologic behaviour and propensity for recurrence might be associated with cell kinetics in the lining epithelium, i.e. infoldings, microcysts and plaques, which are suggestive of active cell proliferation. These areas of epithelial thickening may be comparable to the proliferative changes seen in dental lamina underlying the odontogenic nature of the GOC.
The principles of treatments are still conservative. Treatment recommendations for GOC in the literature are inconsistent and not evidence based due to the rarity of the condition, ranging from minor procedures, such as enucleation and curettage, to major surgery, such as marginal resection, peripheral ostectomy, and partial jaw resection [9].
In conclusion, GOCs are, though rare, should be considered in differential diagnosis of various jaw bone cysts. Scarce occurrence of GOC made it a diagnostic dilemma for pathologists and also challenging to study the biologic behaviour which in turn helps to implement an exact and precise treatment plan thereby precluding the recurrence of the cyst. They are common in middle age group, having predilection for mandible and trauma could be a precipitating factor for its occurrence. The authors agree with Kaplan et al. criteria for diagnosing the GOC. The increased recurrence rate reported in literature can be attributed to misdiagnosis and a conservative treatment with inadequate removal of cyst and lack of follow up. And yet the recurrence can be mainly due to its intrinsic biological behavior and multilocularity of the cyst.
All authors confirm their contribution towards this article.
None
None
- Gardner DG, Kessler HP, Morency R, Schaner DL (1988) The glandular odontogenic cyst: an apparent entity. J Oral Pathol 17: 359-366. [Crossref]
- Padayachee A, Van Wyk CW (1987) Two cystic lesions with features of both the botryoid odontogenic cyst and the central mucoepidermoid tumour: sialo-odontogenic cyst? J Oral Pathol 16: 499-504. [Crossref]
- Magnussson B, Goransson L, Odesjo B, Grondahl K, Hirsch JM (1997) Glandular odontogenic cyst: report of seven cases. Dentomaxillofac Radiol 26: 26. [Crossref]
- Faisal M, Ahmad SA, Ansari U (2015) Glandular odontogenic cyst – Literature review and report of a paediatric case. J Oral Biol Craniofac Res 5: 219-225. [Crossref]
- Noffke C, Raubenheimer EJ (2002) The glandular odontogenic cyst: clinical and Radiological features; review of literature and report of nine cases. Dentomaxillofac Radiol 31: 333-338. [Crossref]
- Economopoulou P, Patrikiou A (1995) Glandular odontogenic cyst of the maxilla: report of case. J Oral Maxillofac Surg 53: 834-837.
- Krishnamurthy A, Sherlin HJ, Ramalingam K, Natesan A, Premkumar P, et al. (2009) Glandular odontogenic cyst: report of two cases and review of literature. Head Neck Pathol 3: 153-158. [Crossref]
- Kaplan I, Anavi Y, Hirshberg A (2008) Glandular odontogenic cyst: a challenge in diagnosis and treatment. Oral Dis 14: 575-581. [Crossref]
- Oliveira Neto P, Sávio E, Bezerra TP, Avelar RL, Raimundo Rde C, et al. (2010) Anterior mandibular swelling. J Oral Maxillofac Surg 68: 436e441.